 Congenital Uveal Lesions
Congenital Uveal LesionsIntraocular Lacrimal Gland Choristoma
General Considerations
There are a several congenital abnormalities that can affect the uvea, such as coloboma and aniridia, but most of them are not directly related to the differential diagnosis of intraocular tumors. The relationship between sporadic aniridia and nephroblastoma is well known, but it is not associated with intraocular neoplasms. Other than the systemic hamartomas and retinoblastoma, which are discussed in subsequent chapters, there are only a few congenital abnormalities of the uvea that have importance in the field of ocular oncology. Congenital iris cysts, which can simulate iris tumors, are more appropriately discussed in Chapter 4, which covers both congenital and acquired cysts. The two that are discussed here are intraocular lacrimal gland choristoma and congenital ocular melanocytosis.
Ectopic lacrimal gland tissue can occur in the orbit, conjunctiva, or eye (1, 2, 3, 4, 5, 6, 7, 8). Intraocular lacrimal gland choristoma is rare; most such lesions have occurred in the iris and a few in both the iris and ciliary body. Several theories on the pathogenesis of intraocular lacrimal gland choristoma have been published (2).
Clinical Features
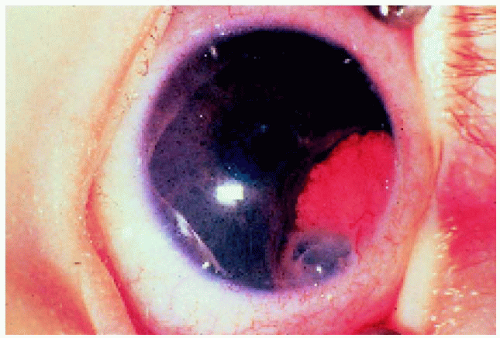
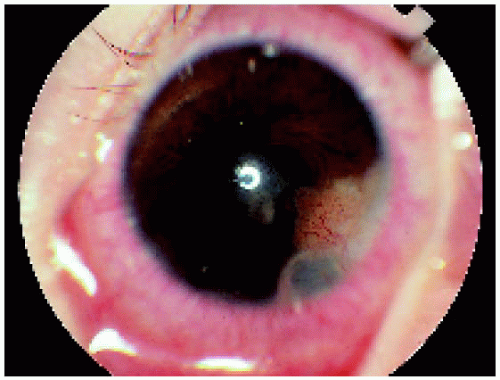
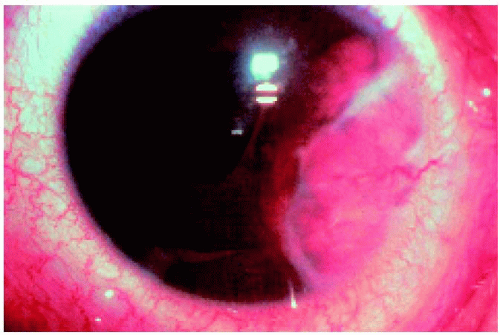
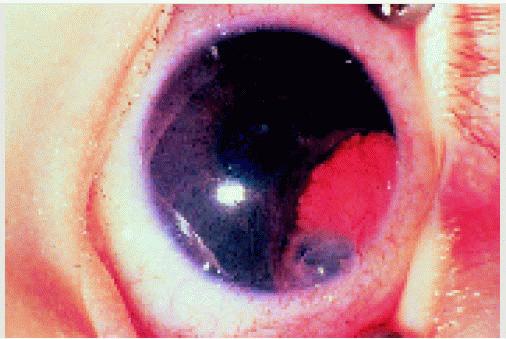
Clinically, intraocular lacrimal gland choristoma usually is recognized in early infancy as a fleshy reddish pink mass of the iris and/or ciliary body (2, 3, 4, 5, 6, 7, 8). It has a slightly lobulated surface that appears almost identical to the normal lacrimal gland as visualized at the time of orbital surgery. Clear cysts can sometimes appear within the lesion early in the clinical course. These have been likened to lacrimal gland cysts (dacryops). With regard to the natural course of intraocular lacrimal gland choristoma, the main mass does not tend to grow significantly, but the cysts within the lesion can progressively enlarge and cause iris atrophy, secondary glaucoma, and cataract. The differential diagnosis includes iris nevus, melanoma, juvenile xanthogranuloma, and other iris granulomas. Although our experience has been limited to larger lesions, it is quite possible that lacrimal gland choristoma can occur as a small, asymptomatic lesion that may remain clinically insignificant.
Pathology
Histopathologically, intraocular lacrimal gland choristoma is a mass composed of normal-appearing lacrimal gland tissue. On occasion, the ducts or acini within the lesion become dilated due to accumulation of clear fluid, probably consistent with tears, in the lumen. This explains the “cysts” that are sometimes seen clinically. On occasion, the diagnosis has been made cytopathologically after fine needle aspiration biopsy (FNAB) (8).
Management
Because iris lacrimal gland choristoma is usually diagnosed in young children and is often stationary or slow growing, periodic observation is often an acceptable initial management. As mentioned earlier, FNAB has been employed to make the diagnosis based on recognition of typical benign epithelial cells consistent with lacrimal gland. In such cases, observation may be initially employed because many cases remain fairly stable. However, we believe that the appearance of a progressively enlarging cyst within the lesion should prompt early surgical removal of the mass to prevent glaucoma and visual impairment. If surgical excision of the lesion is necessary, iridocyclectomy may be required to remove the entire lesion (2). It is feasible that aspiration of the cyst could be a temporizing procedure, although we have not yet performed cyst aspiration in this rare condition.
Selected References
1. Green WR, Zimmerman LE. Ectopic lacrimal gland tissue. Report of eight cases with orbital involvement. Arch Ophthalmol 1967;78:318-327.
2. Shields JA, Eagle RC Jr, Shields CL, et al. Natural course and histopathologic findings of lacrimal gland choristoma of the iris and ciliary body. Am J Ophthalmol 1995;119:219-224.
3. Conway VH, Brownstein S, Chisholm IA. Lacrimal gland choristoma of the ciliary body. Ophthalmology 1985;92;449-453.
4. Morgan G, Mishin A. Ectopic intraocular lacrimal gland tissue. Br J Ophthalmol 1972;56:690-694.
5. O’Donnell BA, Martin FJ, Kan AE, et al. Intraocular lacrimal gland choristoma. Austral NZ J Ophthalmol. 1990;18:211-213.
6. Kluppel M, Muller W, Sundmacher R. Lacrimal gland choristoma of the iris. Arch Ophthalmol 1999;117:110-111.
7. Shields JA, Hogan RN, Shields CL, et al. Intraocular lacrimal gland choristoma involving iris and ciliary body. Am J Ophthalmol 2000;129:673-675.
8. Kobrin EG, Shields CL, Danzig C, et al. Intraocular lacrimal gland choristoma diagnosed by fine needle aspiration biopsy. Cornea, in press 2007.
▪ Intraocular Lacrimal Gland Choristoma
Intraocular lacrimal gland choristoma has characteristic clinical features and is generally managed by local resection, which can be difficult in some cases due to the size and extent of the lesion. Two clinicopathologic correlations are shown.
1. Shields JA, Eagle RC Jr, Shields CL, et al. Natural course and histopathologic findings of lacrimal gland choristoma of the iris and ciliary body. Am J Ophthalmol 1995;119:219-224.
2. From Shields JA, Hogan RN, Shields CL, et al. Intraocular lacrimal gland choristoma involving iris and ciliary body. Am J Ophthalmol 2000;129:673-675.
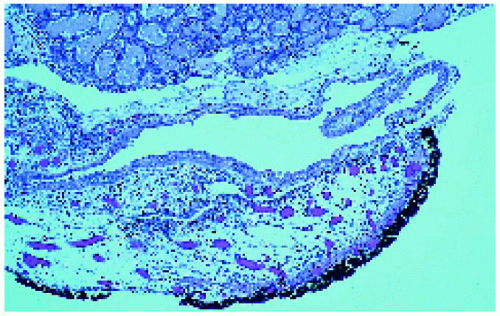 Figure 1.3. Low-magnification photomicrograph showing glandular mass (above) and irregular, partially collapsed cyst (below). (Hematoxylin-eosin ×10.) |
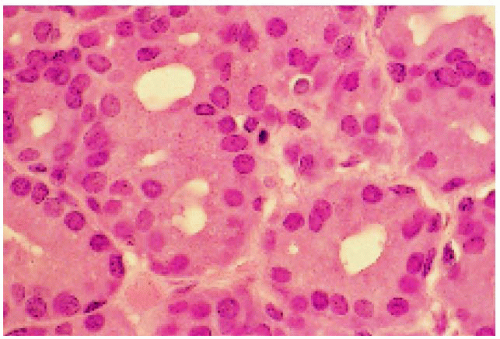 Figure 1.4. Photomicrograph of the solid portion of the lesion, showing glandular tissue identical to normal lacrimal gland. (Hematoxylin-eosin ×200.) |
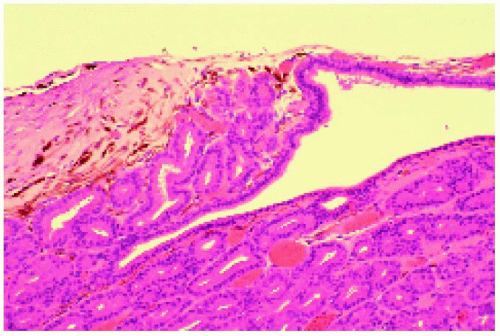 Figure 1.6. Histopathology of lesion seen in Figure 1.5, showing dense fibrous tissue (above) and normal lacrimal gland tissue (below). (Hematoxylin-eosin ×40.) |
Congenital Ocular Melanocytosis
General Considerations
Congenital ocular melanocytosis is a well-known clinical entity that has been the subject of many reports, mainly because of its relationship to uveal melanoma (1, 2, 3, 4, 5, 6, 7, 8, 9, 10, 11, 12, 13, 14, 15, 16, 17, 18, 19, 20, 21, 22, 23, 24, 25). This entity can be divided into ocular melanocytosis and oculodermal melanocytosis, or nevus of Ota (1,2). They have identical episcleral and uveal pigmentation, but the latter has periocular cutaneous pigmentation as well. Both predispose to uveal melanoma, as well as melanoma of the ipsilateral skin, orbit, meninges, and central nervous system, in areas where there are excess melanocytes as a part of this condition. It has been estimated that about 1 in 400 individuals with ocular melanocytosis will develop uveal melanoma (4). Conversely, about 1% of patients with uveal melanoma will have ocular melanocytosis (3).
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree