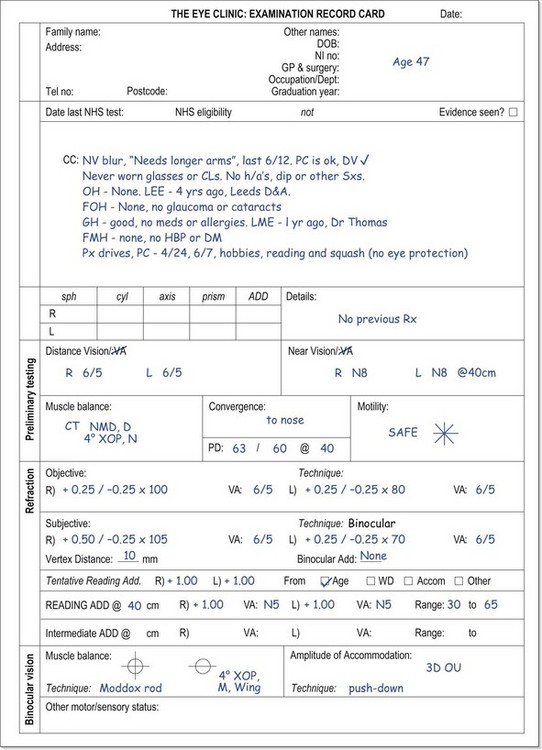
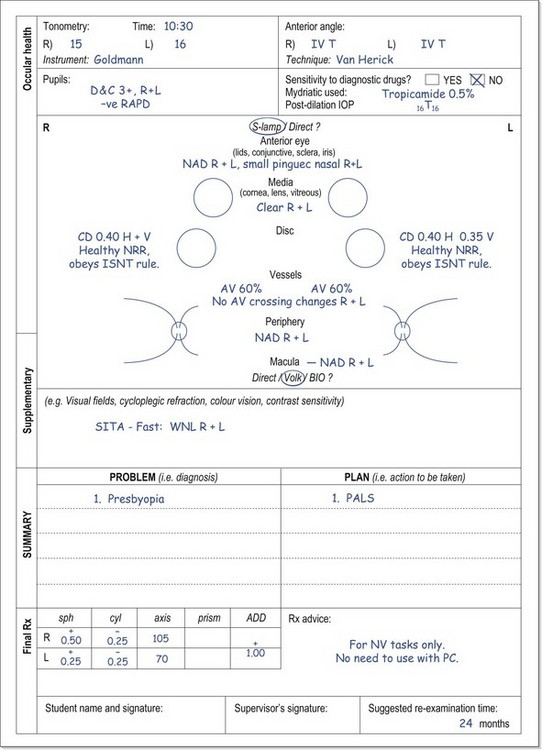
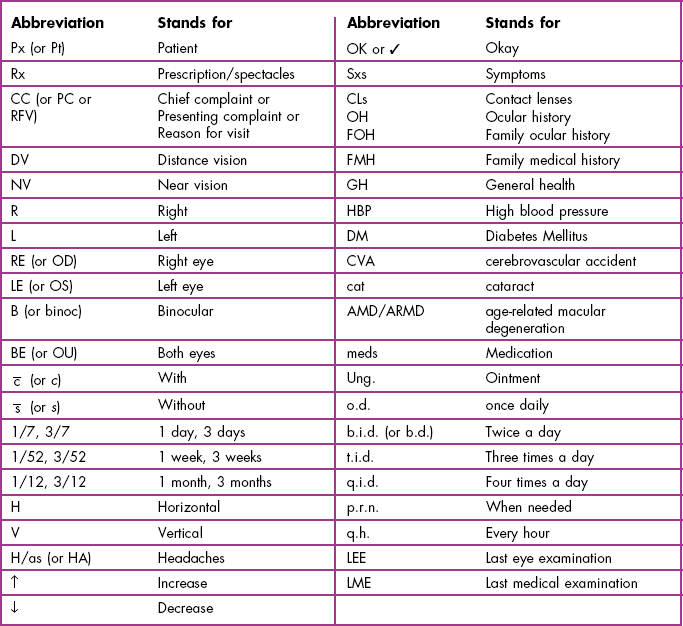
2 Patient satisfaction is vital for a thriving optometric practice as it is associated with greater patient retention, increased patient referrals, greater profitability and lower rates of malpractice suits.1 The medical research literature consistently indicates that patient satisfaction is linked with health care practitioners having good communication skills: being able to explain diagnoses, prognoses, treatment and prevention using clear, non-technical terms1 and being honest, empathic and able to listen well and address patient concerns.2 Poor patient satisfaction is linked with pre-consultation patient anxiety.3 A significant number of patients are anxious about attending for an optometric exam4,5 and particularly fear receiving ‘bad news’ of one form or another.5 Anxiety reduces patient–practitioner communication and causes reduced attention, recall of information and compliance with treatment.5 This limits the usefulness of the examination as an anxious patient is unlikely to provide a full case history and reveal all their visual problems, unlikely to attend appropriately to your instructions, could provide unreliable responses in the subjective refraction and could easily misinterpret or forget what you said about their diagnoses and management plans. Possible reasons for patient anxiety include: (a) Being told they need glasses.3 This can be a worry for both pre-presbyopic6 and presbyopic patients4 who are often concerned about the effect on their appearance. (b) Fear of vision loss. Particularly true of elderly patients where eye disease is a greater risk.4 This could be due to the fact that a friend or family member has lost their vision due to eye disease and this could even have been detected at a routine visit to their optometrist. (c) Cost issues. Some patients are very worried about the potential cost of glasses and contact lenses4,6 and even that they will be ‘sold’ glasses that aren’t necessary. (d) Fear of making a mistake. Some patients are worried about making mistakes during the subjective refraction part of the examination. This may be because they believe that a mistake on their part could lead to the provision of an incorrect refractive correction in their glasses and/or are worried about feeling foolish if they make a mistake (note that some patients can feel educationally inferior to the optometrist7). (e) Fear of increased ametropia. Young ametropes can worry that the increasing myopia or hyperopia will mean thicker and less attractive glasses. Vision-related quality of life has been shown to be reduced in pre-presbyopic spectacle wearers with high prescriptions.8 (f) Being told that they cannot wear contact lenses any more. Young contact lens wearers typically report a better vision-related quality of life than spectacle wearers8 and some may worry about being told that they cannot wear contact lenses any more. (g) Adaptation problems. Many patients report concerns about being able to adapt to their new glasses.4 (h) Fear of looking foolish. Some patients are very tentative about admitting some of their concerns about their vision in case they are made to look foolish by raising the issue. Concerns about vitreous floaters are a typical example of this. A good communicator will be able to relax an anxious patient and increase patient satisfaction with the eye exam.1,3 There are many ways to relax a patient and build a rapport and these include: (a) Provide information about the eye examination (via a leaflet or website, section 2.6) prior to the appointment as this can reduce anxiety and improve satisfaction with the consultation.3,9 (b) Provide a comfortable and welcoming setting in the practice waiting room. Comfortable chairs, a selection of magazines, some low level music, etc., can all help to relax the patient. Framed copies of your qualifications, either in the waiting room or the exam room, can provide reassurance to some patients. (c) Your attire is important and medical research suggests that patients prefer a formal, ‘professional’ appearance.10 This is linked with patients’ trust and confidence, particularly if providing sensitive information in the case history. (d) First impressions count and some practitioners like to greet a patient by name and escort them to the examination room. (e) Beware of making the examination room frightening to the patient. For example, a poster containing a cross-sectional diagram of the eye can be very useful for explanation purposes, but one that portrays a variety of eye diseases is not likely to relax the patient! (f) Change the chair height to ensure you are at the same eye level as the patient.7 (g) Some practitioners like to chat about non-clinical issues (weather, holidays, sports teams, parking, etc.) prior to the examination to help relax the patient. In this respect, it can be useful to make a note of any relevant information (a child’s favourite sport, sports player, team, author; the patient’s pets and their names, their children successes, etc.) to allow you to start a conversation at subsequent visits. (h) Your posture and style should be relaxed but attentive. Maintain regular eye contact and use the patient’s name at appropriate times during the eye examination. (i) An open question is typically used to start the case history (section 2.3.1) as this allows the patient to tell you about any problems with their vision or glasses. A balance is required between allowing the patient plenty of time to discuss their problems and not rushing them but at the same time retaining control of the discussion. You need to ensure that the patient feels that you have fully listened and understood their problems and you may even need to allow the patient to talk about information that you know is not necessary from a diagnostic viewpoint. However, you also need to develop the skill of being able to interrupt an overly talkative patient without appearing rude. (j) Some patients are very shy and an open question provides little information and may make the patient feel uncomfortable. Closed questions can be useful at the beginning of the case history with such patients. An open question can be used later in the case history if the patient relaxes and conversation becomes easier. (k) Listening is a hugely important communication skill. It is vital that you have fully listened to the patient and understood their problems (e.g. Dawn et al.2). There are a variety of ways that indicate to the patient that you are listening and these include maintaining eye contact and demonstrating attention by nodding and/or using affirmative comments such as ‘I see’, ‘I understand’, ‘OK, go on’, etc. Listening is also indicated by using follow up questions to comments, such as asking about the location, onset, frequency, etc., of headaches when the patient indicates that they suffer with them. Finally, summarising the patient’s problems at the end of the case history (section 2.3.1, step 11) is a very useful way of indicating to the patient that you have listened to what they have to say and fully understand what problems they are having, whilst it also provides the patient with an opportunity to inform you if you have missed anything. (l) Provide a brief explanation to the patient of each test that you use during the eye examination. Suggested information, in lay terms, is provided for each test described in later chapters. All students should gain adequate communication skills. You are taught which questions to ask during the case history, what instructions to give for each test, an explanation of why you are doing the test and what to record. In clinics, you will be taught how to provide diagnoses, prognoses and management plans. How do you become a better communicator? You can obviously read about what they are. A brief summary is provided here and further reading is suggested (e.g., Ettinger7). Video recording your case history and/or eye examination can be a valuable tool and will particularly highlight your non-verbal communication skills. Review the video with a colleague and critique your listening skills, your tone of voice, your attentiveness and your eye contact. A helpful quality about communication skills is that you can learn them anywhere and from anybody. Obviously observing an optometrist or other health professional who is popular with patients could be particularly beneficial. You can also learn by experience so that any summer job that involves working with the general public can be beneficial. Indeed, when supervising in student clinics, it is very obvious from the level of communication skills which students have had jobs that involved working with the general public and which ones have not. In the descriptions of clinical procedures in the following chapters, a subsection on recording is included in each case. It is essential that all test results (including the ‘results’ from case history) are recorded. If they are not recorded, subsequent legal analysis of the records will conclude that they were not performed. Clearly, it is important to write legibly on your record cards, for legal reasons and so that they can be read by colleagues who may examine the patient subsequently. Illegible record cards are a significant source of error in primary eye care.11 Similarly, it is hugely important to ensure that record cards are stored in an efficient and organised manner.11 The format of record cards can vary hugely. Many include various designated areas for certain test results that are commonly performed. This is an attempt to save time, as you do not have to write down the test or procedure used, but merely the result. As students will typically use the database style of examination, university clinic record cards (e.g. Figure 2.1) tend to include the majority of tests performed. More experienced optometrists will tend to use the problem-oriented examination which uses the acronym SOAP for its record format.12 The record card itself is a plain white sheet. This reflects the fact that this style of examination is distinguished by its variability, so there is little point in making boxes for individual tests. SOAP stands for Subjective, Objective, Assessment, and Plan. The subjective information is that obtained from the case history and the objective information is the various test results obtained during the examination. The assessment and plan refer to the problem-plan list that is described in detail in a later section. These sections must ‘close the loop’ and link the assessment and plan back to the complaints of the patient. Computer-based systems avoid the problem of illegible records and should reduce the likelihood of lost records (assuming appropriate backup arrangements), which are surprisingly common with paper records.11 Systems vary widely and will continue to improve, but other advantages of current systems include that information from a previous record can be uploaded and then amended with information from the current examination (this can also be done for the right and left eyes); they can be linked to digital ocular photographs; the systems typically learn the information you input and subsequently provide it in drop-down lists and referral letters are easier to produce and print. Disadvantages include the inability to sketch various features (e.g. cataract and fluorescein staining patterns) if digital photography of both the external and internal eye is not available; getting used to different systems can be difficult for locum optometrists; going to a complete computer system means that some companies scan old paper records which can become more illegible by that process; copying information from previous records or the other eye can mean that you forget to put in details; drop down lists can become very long and it can be difficult to get an overall picture of a patient because of the fragmented nature of the information. The latter can mean it is difficult to highlight important details as with a paper record card you can write it in large capitals/highlighter on the front page. 1. Make sure that the room lights are on before the patient enters the examination room. 2. Consider the patient’s age (gender and ethnicity may also be important) as this can provide useful clues to what their problems might be given the known epidemiology of certain ocular problems. For example, a 47-year-old patient attending for their first eye exam for many years is likely to complain of presbyopic-related symptoms. 3. Observe the patient’s stature, walking ability and overall physical appearance. Pay particular attention to any head tilt or obvious abnormalities of the face, eyelids and eyes that will require further investigation such as facial asymmetry, lid lesions, ptosis, epiphora, entropion, ectropion, a red eye or strabismus. 4. You should sit about 1 m from the patient at eye level. Your posture and style should be relaxed but attentive. Lean slightly forward towards the patient. Try to avoid long silences while writing notes and learn to write down answers in abbreviated form (see Table 2.1) as the patient is talking, while retaining intermittent eye contact. 5. Chief complaint (CC) or reason for visit (RFV): Determine the chief complaint by asking a very general open-ended question such as ‘Do you have any problems with your vision or your eyes?’ or ‘Is there any particular reason for your visit, Mr Smith?’ 6. In a patient who reports no problems to the question above and is attending for their regular annual/biennial examination, ask the following questions (see recording example in 2.3.3.a): (a) If the patient wears glasses (ask if you are unsure), you need a complete description of them. This may include: (i) ‘When do you wear your glasses?’ (ii) ‘How is your distance vision in your glasses?’ followed up by ‘Do you feel it is as good as it was when you first got them?’ This can be adapted to suit the patient. For example, a student could be asked ‘Any problems reading from the whiteboard?’ and ‘Is everything clear on the TV?’ (iii) ‘Any problems with reading with the glasses?’ (iv) ‘How is your distance/near vision without your glasses?’ (v) ‘How old are your glasses?’ (vi) ‘How many pairs of glasses do you have?’ (vii) ‘Where did you get these glasses from?’ (viii) ‘How old were you when you first wore glasses?’ (b) If you are unsure, ask if the patient wears contact lenses. If they do wear lenses, even if only occasionally, then you need a complete description of the contact lenses used: (i) ‘What type of lens are they?’ (soft, gas permeable, toric, multifocal, etc., and brand if known) (ii) If relevant (i.e. not single use lenses): ‘How often do you replace your lenses?’ and ‘What care solutions do you use?’ (iii) ‘How long do you usually wear the lenses each day?’ and ‘How many days per week?’ The first question can be confirmed by asking when they typically put their lenses on and when they typically remove them as average wearing times are typically underestimated. (iv) ‘How many hours of comfortable wear do you get with your contact lenses?’ (v) ‘How is your vision with contact lenses and how does it compare with the vision you get with your glasses?’ If the patient wears both glasses and contact lenses, you will have to ask about visual symptoms (i.e. distance blur, near blur, headaches, eyestrain, etc.) for both forms of correction. (vi) ‘Are you having any problems with your contact lenses currently?’ (vii) ‘When was your last contact lens aftercare and when is your next aftercare check scheduled for?’ (c) A patient who does not wear glasses or contact lenses should be asked about the clarity of the distance and near vision. (d) Complete a symptom check by asking about the most common symptoms: 7. Patient reporting visual symptoms (see recording examples in 2.3.3b). (a) L – Location/laterality. Examples: • ‘Is it more blurred in one eye or is it the same in both?’ • ‘In which part of the head is the headache located?’ For a frontal headache, ask ‘Is it above one eye more than the other?’ • ‘Is the double vision in all directions of gaze or just one?’ (c) F – Frequency/occurrence. Examples: • ‘How often do you get headaches?’ Prompt if the patient is unsure: ‘Every day? Once a week? Once a month?’, ‘Are they any better on weekends?’, ‘Do they tend to occur at any particular time of day? Morning mainly or evening?’ • ‘How often do you get double vision?’, ‘How long does it last?’, ‘Does the double vision occur after a lot of reading or at anytime?’ (d) T – Type/severity. Examples: • ‘Did the blurred vision start suddenly or gradually?’ If sudden vision loss, ask ‘Was the vision loss partial or total?’ • ‘Is it a throbbing, sharp or dull headache?’ • ‘Is the double vision one-on-top-of-the-other or side-by-side?’ (e) S – Self-treatment and its effectivity: • ‘How have you coped with the blurred vision?’(possibly by squinting, sitting at the front of the class, sitting close to the TV, using ready readers, borrowing a family member’s glasses, etc.) • ‘Does anything make the headaches go away?’ ‘Do you take any painkillers for the headaches?’ (f) E – Effect on the patient: • ‘How is your son’s school work progressing?’, ‘Does it affect your hobbies or sports?’, ‘Is your poor vision affecting how well you can do your job?’, ‘Have you restricted your driving?’, ‘How well do you manage driving at night?’ • ‘How badly do the headaches affect you?’, ‘Have you been to see your GP about the headaches?’ (g) A – Associated factors: ‘Are there any other symptoms associated with the problem?’ 8. Completion of information gathering for a patient with a chief complaint.
Communication skills
2.1 Turning anxious patients into satisfied ones
2.1.2 Understanding patient anxiety
2.1.3 Building a rapport: relaxing the patient
2.1.4 How to improve your communication skills
2.2 Record cards and recording
2.2.1 SOAP
2.2.2 Computer-based systems
2.3 The case history
2.3.1 Procedure (Summary in Box 2.1)
![]()
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


Communication skills