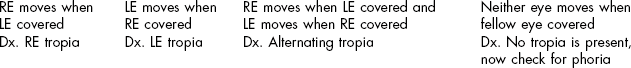
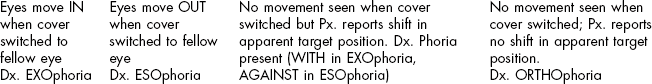
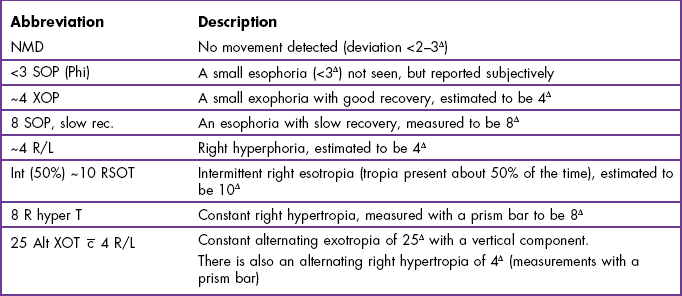
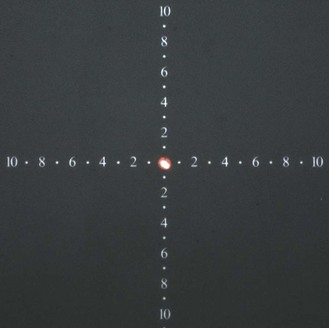
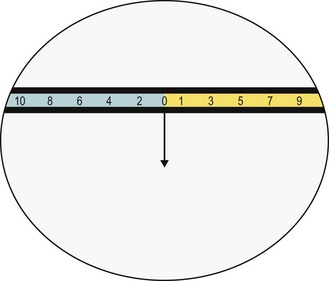
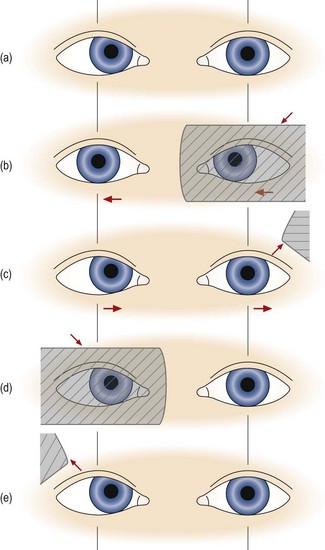
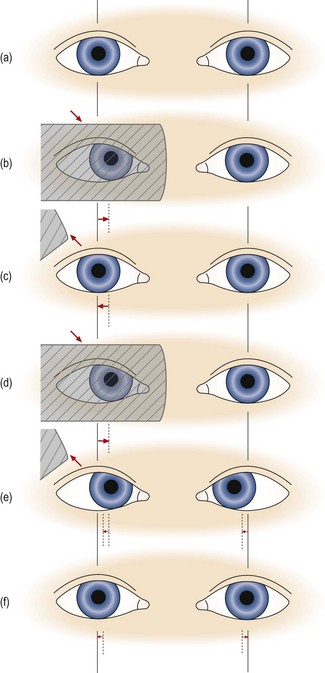
6 6.1 Relevant information from case history and assessments of other systems 6.3 Other tests for the detection and measurement of heterotropia 6.4 Other tests for the detection and measurement of heterophoria 6.6 Convergence ability: Near point of convergence (NPC) and jump convergence 6.8 Vergence facility: Prism flippers 6.9 Amplitude of accommodation 6.12 Accommodative convergence/accommodation (AC/A) ratio 6.15 Motility test and other tests for diagnosing/measuring incomitancy 6.16 Identifying the defective muscle: Parks 3-step test 6.17 Assessment of eye movements 6.18 Considering test results in combination Tests that assess the binocular vision and accommodation systems are described in this chapter. Rather than group these tests in terms of preliminary/pre-refraction and post-refraction tests, tests are grouped together depending on the aspect of binocular vision or accommodation that they help to assess. This is because the organisation of the book is directed towards the assimilation of a problem-oriented approach (section 1.3.3). Although the chapter contains a large number of tests that may at first appear independent of one another, a systematic, problem-oriented approach is advocated in which only the most appropriate tests are conducted. In the final section (section 6.18) a brief overview is provided of how the results from different tests can be considered in combination in order to aid diagnosis and thus inform management. (a) Simple observation of the patient can highlight a strabismus or head turn or tilt. Parents or carers may also inform you that they have noticed that their child occasionally has an ‘eye turn’ or perhaps an abnormal head posture. Any suggestion of a strabismus requires a careful cover test and a stereopsis test in addition to looking for amblyopia and possible causes of the strabismus such as hyperopia. (b) Symptoms of blurred vision, headaches or asthenopia at distance and/or near can indicate a decompensated heterophoria or accommodative insufficiency or excess at that distance. (c) Complaints of ‘double vision’ could suggest a heterophoria breaking down into a heterotropia (typically horizontal diplopia, occurring especially when tired), a remote near point of convergence (section 6.6), the angle of strabismus changing so that the retinal image falls out of the suppression area or an incomitant deviation (section 6.15). An appropriate line of questioning during the case history will help in this differential diagnosis. Beware that children sometimes complain of ‘double vision’ when they mean blurred vision. Note that cortical cataract and occasionally posterior subcapsular cataract can cause monocular diplopia (or polyopia) and should be considered in elderly patients by determining if the diplopia persists if one eye is covered. (d) Signs or symptoms of fluctuations in distance vision and, in particular, symptoms of distance blur after near work, suggest problems of accommodation and tests that assess accommodative function should be employed (sections 6.9–6.11). (e) No symptoms: It is worth remembering that a lack of symptoms does not, in itself, mean that the binocular system is normal. For example, patients with suppression or long-standing heterotropia almost certainly will not experience binocular vision symptoms. (f) Poor reading ability and poor progress at school could also be due to an accommodation or binocular vision problem. Children especially might not complain because they often think everyone sees the way they do. It is also useful to ask the child’s parent/carer about the pregnancy and birth history. There is a high prevalence of ocular abnormality, in particular strabismus, in children born prematurely, those with low birth weight or disorders of the central nervous system, and in children with significant birth complications (e.g. forceps delivery).1 It is, therefore, recommended that the following questions be posed to the parent/carer during the case history examination: Was the child a full-term baby or were they born prematurely? What was the birth weight? (Less than 2500 grams or 5.5 pounds is a significant risk factor for strabismus, in particular esotropia).2 Were there significant complications at the child’s birth? Is the child’s current and past general health good? Since birth, has the child been investigated or received treatment for any medical condition? In cases where the acuities in the right and left eyes are similar or identical, it is usual to find that binocular visual acuity (VA) is ½ to one line better than monocular acuity.3 Of course, it is not possible to find this improvement if monocular VA equals the ‘bottom line’ of the Snellen chart you are using (section 3.2.2). When using a non-truncated chart, a binocular VA that is equal or worse than the monocular VA can indicate a binocular vision problem. A poor patient reaction to the restoration of binocular vision after an occluder has been removed following monocular subjective refraction can also indicate a binocular vision problem. Fluctuations in retinoscopy, retinoscopy results more than 1.00 D more positive than subjective refraction and/or fluctuations in subjective refraction suggest fluctuations in accommodation and/or latent hyperopia or pseudomyopia and should be investigated using assessments of accommodation (sections 6.9 to 6.11) and/or cycloplegic refraction (section 4.13). The cover test, in combination with the motility test (section 6.15), represents the corner-stone of the assessment of oculomotor alignment. The aim of the test is very simply to allow you to observe what happens when binocular vision is suspended by covering one eye whilst the patient has been instructed to view a near, intermediate or distant target. It is often important to determine the effect of any refractive error on the deviation, so an assessment of binocular status is often required in the unaided state, with the patient’s own spectacles and with the optimal refractive error. While the cover test must always be carried out, it is usual for it to be conducted prior to the refraction. It is not generally repeated post-refraction (although it can be) because other tests of heterophoria are typically employed after the subjective refraction has been completed. These tests are described in section 6.4. The cover/uncover test is the only method by which an ocular deviation can be distinguished as either a heterotropia (also called a ‘tropia’, ‘strabismus’ or a ‘squint’) or a heterophoria. The test has the advantage of being an objective test (i.e. one that requires co-operation but no response from the patient) although the subjective response of the patient while performing the test can provide valuable additional information. The cover test provides considerable information about a deviation including its direction and size. In addition, the pattern of movements observed may enable you to form an opinion about the stability, constancy, laterality or control of a deviation. The test is quick and simple to perform. One disadvantage of the test is that even experienced practitioners cannot detect very small deviations (up to 2–3Δ).4 Since even small vertical heterophorias can be clinically significant, it is likely that you would miss these if just using the objective cover test. However, small deviations of any variety may be identified using the subjective cover test. The only real disadvantage of the cover test is that it requires considerable practice before accurate observations can be made. In addition, it is vital to be systematic in your approach (Box 6.1). FIRST: Search for the presence of a heterotropia. If one exists, then by definition, a heterophoria cannot be present simultaneously. SECOND: If there is no heterotropia, search for a heterophoria using the alternating cover test and/or the cover/uncover test. THIRD: If no heterophoria is evident you should perform a subjective cover test. 1. Keep the room lights on and, if necessary, use localised lighting so that the patient’s eyes can be easily seen without shadows. 2. Explain the purpose of the test to the patient: ‘I am now going to find out how well your eye muscles work together’. 3. The following targets should be used: (a) For the distance cover test, isolate a single letter of a size one line larger than the patient’s VA of the poorer eye. For example, if monocular VAs are 6/4.5 (20/15) and 6/9 (20/30), use a 6/12 letter (20/40) as a target for the distance cover test. The patient must be able to easily see the letter with both eyes, but it should be a target that requires accurate fixation and accommodation. If you are using a computer-based or projector chart, isolate a single letter on the appropriate line. If you are using a printed chart, then ask the patient to look at a letter at the end (or beginning) of a line, as it will be easier to locate after the eye has been uncovered and crowding effects are lower. If the monocular VA in either eye is 6/18 (20/60) or worse, a spotlight may be used for fixation. (b) For the near cover test, a fixation stick should be used that contains letters or pictures of various sizes (Figure 6.1). A single letter of a size one line larger than the patient’s near VA of the poorer eye should be chosen. As most near VA charts are truncated to N5 or 0.4 M (20/20), this will tend to be N6 or 0.5 M (20/25). The fixation stick should be held at the patient’s near working distance (this may be at an intermediate difference if you wish to assess their binocular status at a distance at which they view a computer screen). 4. Irrespective of whether you are carrying out a cover test during distance or near viewing, you should sit directly in front of the patient, at a distance of 25–40 cm away. This will place you close enough to be able to critically note eye movements. When performing the cover test for distance viewing, you should be very careful not to block the patient’s view of the fixation target. (a) For the distance cover test, the patient should have their head erect and eyes in the primary position of gaze. (b) For the near cover test, the eyes should be in a slight downward gaze (similar to the position for reading). 5. Instruct the patient: ‘I would like you to look at the letter * at the other end of the room (or the letter * on this stick). Please keep watching the letter as closely as you can. In a moment I will place this cover in front of your eye. If the letter appears to move please follow it with your eyes and keep it as clear as possible at all times’. 6. Before starting the cover test take the opportunity to observe the fixational stability of the patient’s eyes as they view the letter. You can gain a good impression of the stability of their fixation simply by observing their eyes for a period of a few seconds (e.g. 5–10 seconds) as you remind them to keep looking closely at the letter. 7. Perform the cover/uncover (unilateral cover) test to look for a heterotropia (Figure 6.2): Fig. 6.2 Cover test in a patient with a right esotropia. (a) The right eye deviates inwards slightly, but this may not be obvious depending on its size and your experience. (b) As the left eye is covered, the right eye is seen to move out to take up fixation. Behind the cover, the left eye moves to the right, obeying Hering’s law. (c) As the left eye is uncovered, it moves out to take up fixation as it is the non-strabismic eye. (d) When the right eye is covered, the left eye does not move. (e) When the right eye is uncovered, neither eye moves. Reprinted with permission from Pickwell D (1989). Binocular vision anomalies. Butterworth-Heinemann. (a) Place the cover before the left eye. As you do so, observe the response of the right eye that has not been covered. Repeat this procedure two or three times before you arrive at any decision. If the right eye moves when the left is covered, then a tropia is present in the right eye. The movement observed occurs to take up fixation. You should allow the eye time to take up fixation, which may be as long as 2–3 seconds. If the eye moves out to take up fixation, then in the binocular situation it must have been directed inwards and so an ESOtropia is present. If the eye moves in to take up fixation an EXOtropia is present. If the eye moves up to take up fixation, then in the binocular situation it must have been directed downwards and so a HYPOtropia is present. If the eye moves down to take up fixation, a HYPERtropia is present. (b) Repeat the cover/uncover test by placing the cover over the right eye and look for a heterotropia in the left eye. Once again, repeat the procedure two or three times. If neither eye moves when the other is covered there is no heterotropia and you should go to step 8 below. (c) In a unilateral strabismus, when the deviating eye is covered and then uncovered, the non-tropic ‘normal’ eye will continue to fixate and will not move. If there is a unilateral heterotropia present, there is frequently amblyopia so that the visual acuity is reduced in that eye. (d) Eyes with strabismus and amblyopia may not take up fixation immediately when the fellow eye is covered. Give them time to fixate and actively encourage them to do so. Note and record any fixation instability or tremor (nystagmus) when the patient attempts to fixate with the eye that normally deviates. (e) Note that some heterotropias may be intermittent. Typically these are large heterophorias that sometimes break down into a heterotropia. If you suspect an intermittent tropia, use the alternating cover test to investigate whether the tropia is evident when the alternating cover test is concluded. If a tropia is now present, this indicates that the patient may develop a strabismus (i.e. and potentially therefore experience double vision) when tired or under stress. (f) Repeat the test from the beginning to confirm your diagnosis. (g) If a heterotropia is present there is no need to search for a heterophoria. You should record your result and move on to the next test (e.g. cover test in different refractive correction, or at a different viewing distance). Note that it is not meaningful to speak of ‘recovery’ movements in relation to tropia movements because there is no fusion reflex to bring the eyes back into alignment. When the cover is removed and habitual viewing is restored the movements that are seen have no diagnostic value in the way that recovery movements are valuable in patients with heterophoria (see 10(d) below). 8. If no heterotropia was found you should now begin the search for a heterophoria. There are two possible alternatives here and both have their advocates. Some practitioners will continue to use the cover/uncover test that was used for heterotropia investigation in the search for a heterophoria. If this is your preferred approach then go to step 9 below. An alternative approach is to switch now to the alternating cover test. If this is your preferred approach then go to step 10. Some practitioners use both techniques to evaluate heterophoria. There is no research to support one approach over the other. 9. If no heterotropia is present, perform the cover/uncover test to look for a heterophoria (Figure 6.3): Fig. 6.3 Cover test in a patient with esophoria. (a) to (c) show the simple pattern of movements that are usually seen, and (d) to (f) show the more rare versional pattern of movements that can occur when one eye is dominant. (a) Both eyes look straight ahead. (b) The right eye is covered and the left eye does not move, indicating that there is no strabismus in the left eye. Behind the cover the right eye moves inwards. (c) The right eye is uncovered and the right eye moves out to resume fixation with the other eye. Note that during the movements of the right eye, the left eye has not moved, and disobeys Hering’s law to maintain fixation. (d) The right eye is covered as before and it moves inwards behind the cover. (e) The right eye is uncovered and both eyes move right by the same amount, obeying Hering’s law. (f) Both eyes diverge by the same amount, again obeying Hering’s law, and take up fixation. Reprinted with permission from Pickwell D (1989). Binocular vision anomalies. Butterworth-Heinemann. (a) In heterophoria, the eye being covered will move out of alignment with the other eye because sensory fusion is being prevented. It will then retake up fixation when the cover is removed. Some practitioners attempt to observe both the movement of the eye that is under cover and the recovery movement of that eye when the cover is removed. This requires some dexterity on your part and care must be taken to ensure that the ‘cover’ is really covering the patient’s view of the target. Other practitioners only attempt to observe the eye’s recovery movement when the cover is removed. If you choose to do the latter, then go directly to step (c). (b) Place the cover before the left eye in a manner that prevents the patient from viewing the target but allows you to continue viewing the covered eye. Observe the response of the left eye behind the occluder when it is first covered. If a heterophoria is present then the covered eye will drift outwards in EXOphoria, inwards in ESOphoria, upwards in HYPERphoria and downwards in HYPOphoria. (c) Observe the response of the covered eye as the cover is removed. Remove the cover in a manner that allows you to view the eye continuously as it is being uncovered. In other words don’t move the occluder away from the patient’s eye in a fashion that causes you to temporarily lose sight of it. For example, you can remove the cover from in front of the patient’s right eye by moving the cover diagonally downwards and temporally. Note the recovery movement of the eye will be opposite to that which took place behind the cover. For example, in EXOphoria the eye moves back in when the cover is removed as it drifted out (away from the nose) behind the cover. (d) In a small number of patients, generally with large phorias or when a highly dominant eye is uncovered, the fixating eye undergoes a flick or wobble as the cover is removed from the other eye. This is due to the eyes more closely following Hering’s law of equal innervation (Figure 6.3d–f). (e) Since it is not possible to observe the two eyes at once when the cover is removed, you should repeat this cycle several times, watching first one eye and then the other and comparing the movement of the two. However, you should leave several seconds between each cycle to avoid inadvertently performing an alternating cover test. (f) Repeat the observations when covering and uncovering the right eye. If an esophoria was present in the left eye, it should be present and similarly sized in the right. It does not make sense to state that a patient has, for example, ‘esophoria of the right eye’ since esophoria of the same or very similar magnitude will almost always be present when the left eye is covered. There are some rare exceptions to this rule, such as in patients with uncorrected or residual anisometropia, where greater accommodative convergence in one eye influences the movements. Because the presence of a vertical heterophoria signals a tendency for the eyes to drift out of vertical alignment, a hypophoria evident in one eye will be evident as a hyperphoria in the fellow eye. Once again, however, the deviations will usually be of a similar size in the two eyes. (g) Estimate or measure the magnitude of the deviation. Deviations can be measured by placing prisms of increasing power in front of one eye until no movement is observed during the cover/uncover test. The prism is normally placed in front of one eye only. Base-in prism power is used to measure EXOphorias/EXOtropias, and base-out to measure ESOphorias/ESOtropias. A prism bar is most conveniently used for this purpose, although estimates made by experienced practitioners can be in good agreement with measurements made using prism bars.5 10. If no heterotropia is present, perform the alternating cover test. (a) Place the occluder before one eye for 2–3 seconds and then transfer it quickly to the other eye, without pausing. Keep the occluder in front of the eye for 2–3 seconds, and allow the other eye to take up fixation, and then repeat the cycle. The patient must not view the target binocularly at any time and thus rapid movement of the cover between the eyes is required. For this reason, the occluder should be moved along a horizontal line between the eyes rather than in an arc-shaped pattern. In order to facilitate swift transfer of the cover between the eyes it is best if your hand that holds the cover is held close to the patient’s forehead or alternatively, close to the tip of the patient’s nose. (b) If there is a deviation of the eyes, it will be seen as a re-fixation eye movement when the cover is transferred from one eye to the other. The eyes will move outwards in ESOphoria/ESOtropia, and inwards in EXOphoria/EXOtropia, etc. (c) Estimate or measure the magnitude of the deviation. Deviations can be measured by placing prisms of increasing power in front of one eye until no movement is observed during the alternating cover test. The prism is normally placed in front of one eye only. Base-in prism power is used to measure EXOphorias and base-out to measure ESOphorias. A prism bar is most conveniently used for this purpose, although estimates made by experienced practitioners can be in good agreement with measurements made using prism bars.5 To help you make better estimates of deviation sizes, ask your patient to look from the first to the last letter on the Snellen 6/12 (20/40) line at six metres (20 ft) with one eye occluded. The movement observed is equivalent to 4 prism dioptres and using this as a guide provides a good way for you to estimate other deviation sizes. (d) Unlike in cases of heterotropia, observe the latency and the speed of the fusional recovery movement on uncovering, since this may give clues as to the strength of the fusion reflex. The movement should be smooth and fast. Poor fusion reflexes are slow and hesitant, with jerky movements. 11. If no heterophoric movements are seen during the alternating cover test, perform the subjective cover test. If you cannot see any movement of the eyes during step 10 and the patient can provide good subjective responses, continue to perform the alternating cover test and ask the patient if the target appears to move when the occluder is switched from one eye to the other. Subjectively reported movements of the target are called ‘phi’ (pronounced as ‘fy’ as in ‘why’) movements. Small amounts of phoria (1–3Δ) may be detected in this way. Any reported vertical phi movement should be further investigated using other tests, such as the modified Thorington technique (section 6.4). The type of deviation present can be inferred according to whether the target appears to move in the same or opposite direction as the cover. For example, esophoria will cause the target to move ‘against’ the movement of the occluder and an exophoria will cause the target to move ‘with’ it. 1. When examining children: Pictures can be used to retain attention, but they should be of an appropriate size. Pictures (or letters) that are too large do not provide an accurate stimulus for fixation or accommodation and this is essential for an accurate cover test. In order to check compliance with your instructions, it is useful to occasionally move the stick a short distance to one side. If the eyes are seen to follow the target then you can be confident that your instructions are being followed. 2. If a heterotropia is suspected in a patient with equal VA in the right and left eye: (see online video 6.6) 3. In patients with an abnormal head posture (head turn or tilt): Ask the patient to straighten their head position before testing commences. If the abnormal head position is a permanent feature for a particular patient, the cover test should be carried out with the head in the habitual (i.e. turned/tilted) position and again when the head is straightened. If the deviation differs markedly with adjustment of the head position, it is possible that the head is being turned/tilted to address an underlying binocular vision issue. This can be further investigated if the head is tilted/turned in the opposite direction to the direction that the patient typically exhibits. If the deviation becomes even more pronounced, an incomitancy is certainly present and you can conclude that the abnormal head posture is linked to a binocular vision condition rather than to another, non-visual cause. 1. Record NMD (No Movement Detected) if this was the case and if no assessment of ‘phi’ movement was conducted. NMD is preferred to ‘ortho’ (i.e. orthophoria) or similar, as even experienced practitioners cannot detect very small eye movements (up to 2–3Δ).4 Hyperphorias of this size can be significant and cause the patient problems, so you must not assume that the patient does not have a significant phoria based on detecting ‘no movement’ using the cover test. 2. Record ‘ortho’ (orthophoria) or similar ( 3. If heterotropia is detected, then record: • The constancy (if intermittent is not recorded, the tropia is assumed to be constant. If the deviation is intermittent, note the percentage of time that the eye deviates). • Which eye is deviated (right, left or alternating; abbreviated to R, L or Alt)? • The direction (exo, eso, R hyper or hypo, L hyper or hypo, excyclo, incyclo). Exo and Eso are abbreviated to XO and SO, respectively. • Add the suffix tropia (abbreviate to T, e.g., SOT, XOT). • An indication of the size of the tropia, either measured with a prism bar or estimated (if estimated, precede your result with the symbol ‘~’), e.g. ~20 Δ L XOT. Remember that it is not meaningful to attach significance to (or record) ‘recovery’ movements in patients with a tropia. • Heterotropias can also be defined as following an A- or V-pattern or other varieties of alphabet pattern (e.g. Y or inverted Y). By definition such deviations are of the incomitant variety and their presence will emerge during the motility test (section 6.15). Examples are given in Table 6.1. 4. If heterophoria is detected, then record: • The direction (exo, eso, R/L or L/R). Exo and Eso are abbreviated to XO and SO, respectively. R/L indicates a right hyperphoria, which is the same as a left hypophoria. L/R indicates a left hyperphoria/right hypophoria. • Add the suffix phoria (abbreviate to P, e.g., SOP, XOP). • An indication of the size of the phoria, either measured with a prism bar or estimated (if estimated, precede your result with the symbol ‘~’). • Any recovery movements that were slow, hesitant and/or jerky. Normal, smooth and fast recovery movements are generally not recorded. • Heterophorias that were found using the subjective cover test, but not seen by you, should be recorded in the usual manner and followed by the term ‘phi’. • A and V patterns may also be seen in patients with heterophorias and, as in the case of heterotropias, this also signifies the presence of an incomitant deviation (section 6.15). Examples of appropriate test recordings are given in Table 6.1. Hering’s law states that the innervation to synergist muscles of the two eyes is equal. This would imply that the eyes would always move by equal amounts (in the same direction in version movements and in the opposite direction in vergence movements). The common cover test response, in which the fixating eye remains still and the uncovered eye moves to restore fusion thus contravenes Hering’s law. Hering’s law would predict that when one eye is uncovered, both eyes would make a version movement equal to half the deviation, and then both eyes would make an equal fusional (vergence) movement, to restore bifoveal fixation. This response does occur in some patients and should not be confused with heterotropic movements (Figure 6.3). Note that heterotropic cover test movements are in one direction and take place when the cover is introduced to the other eye whereas, when they occur, Hering’s law movements have the appearance of a ‘wobble’ and take place when the cover is removed from the other eye (see online videos 6.7 and 6.10) Most children show no movement on the cover test at distance and either no movement or a just visible exophoria at near.6 There appears to be little information regarding cover test results for normal adults in the research literature. Textbooks suggest that the majority of adults will also show either no movement or a just visible exophoria or esophoria (up to about 4Δ) on the distance cover test.7 At near, a small amount (3Δ to 6Δ) of exophoria is considered normal (physiological exophoria) and this is likely to increase with age (exophoria measured with the Maddox wing increased from a mean of zero at age 20 to 5Δ at 65).8 As even experienced practitioners cannot detect very small eye movements (up to 2–3Δ), small hyperphorias will be missed with the objective cover test, and any hyperphoria that is detected will be abnormal.4 The movements made by each eye are usually similar in heterophoria. In cases where the heterophoria movement is greater in one eye than the other, suspect poor technique (and re-assess), uncorrected or residual anisometropia or incomitancy (section 6.15). 1. Not positioning yourself appropriately to allow a clear and unimpeded view of the patient’s eyes. 2. Blocking the patient’s view of the target that you have instructed them to fixate upon. This is only a problem during the distance cover test. 3. Covering and uncovering the eyes so rapidly that the eyes do not have time to make the movements consistent with the deviation that is present. In the alternating cover test, you should leave the cover in place for at least 2–3 seconds before removing it or transferring it to the other eye. 4. Arriving at your diagnosis too quickly. Repeat the test two or three times in quick succession to confirm your diagnosis. Fixational instability can cause a misleading result on a single test. 5. Using a fixation target that is too large. 6. Using large, sweeping lateral movements of the occluder when covering/uncovering. This is distracting for the patient, and during an alternating cover test, may mean that binocular vision isn’t being fully suspended. Small but swift movements with the occluder are required. 7. Diagnosing a heterotropia when there is a temporary loss, but then a quick recovery, of fixation of an eye when the fellow eye is uncovered (Figure 6.3e and f). 8. Failing to record information about the speed and/or smoothness of recovery in patients with a heterophoria in patients in whom the recovery is slow or jerky. Conversely, recording information about recovery in heterotropia patients. The Hirschberg test compares the position of the corneal reflexes (the first Purkinje images) of the two eyes that are formed by a pentorch. It is quick and easy to perform, and requires little co-operation on the part of the patient, but can really only be performed at near, the penlight target provides a poor stimulus to accommodation and it is relatively inaccurate. Choi and Kushner found that even experienced practitioners can obtain results that differ by up to 10 prism dioptres.9 This is because a deviation of just 1 mm is equivalent to ~22 Δ. The Krimsky test extends the Hirschberg test by using prisms to equalise the positions of the corneal reflexes in the two eyes. The Bruckner test relies upon a comparison of the brightness of the retinal reflex in the two eyes. In the presence of a strabismus the reflex can be brighter and whiter in the deviating eye as compared to the reflex from the fixing eye due to fundal reflections from a deviating eye being greater than from the darkly pigmented macular area of a normally fixating eye. The usefulness of the Bruckner test is, however, controversial.10,11 Given their limited accuracy, the cover test (section 6.2) should be used in preference to these tests as soon as the child can co-operate with the cover test requirements. 1. Keep the room fully illuminated. Additional use of localised lighting is recommended so that the patient’s eyes can be easily seen without shadows. 2. Remove any spectacles that the patient may be wearing. However, if it is felt that the refractive correction will alter the result (e.g. in cases of significant hyperopia), the test should also be performed through the correction. 3. Hold a penlight horizontally 40 to 50 cm from the patient with the light aimed at the bridge of the patient’s nose. The back of the penlight should be very close to the tip of your nose. 4. Ask the patient to look at the light with both eyes open. Young children will automatically tend to look toward the bright light but may need a little encouragement. 5. Note the location of the corneal reflex in each eye individually. In order to do this you should briefly cover each eye in turn; you can do this with the palm of your hand. Remember that the reflex is frequently decentred about 0.5 mm nasally with respect to the centre of the pupil because angle kappa is normally positive. 6. Now compare the location of the corneal reflexes as the patient views habitually (i.e. without any occlusion). The eye that has the same angle kappa as in the monocular test is the fixing eye. The location of that reflex should be considered the reference position. 7. If there is a heterotropia present, the corneal reflex of the other eye will have shifted in a direction opposite to that of the ocular deviation. For example, in the case of an ESOtropia, the corneal reflex will be displaced temporally on the patient’s cornea relative to the position of the reflex in the fellow eye. 8. Hirschberg: Estimate the magnitude of the deviation from the displacement of the reflex in millimetres (mm) relative to the reference position using the approximation of 1 mm = ~22Δ. 9. Krimsky: Use a prism bar in front of the fixating eye in order to centre the corneal reflex in the deviated eye. Measures of the angle of heterotropia obtained using the Krimsky test rely upon the assumption that the deviating eye fixates centrally rather than eccentrically. While this assumption may not be valid in many instances, the error it introduces is likely to be small in relation to the overall size of the deviation. 1. Turn down the lights so the room is dimly lit. 2. Remove any spectacles that the patient may be wearing. However, if it is felt that the refractive correction will alter the result (e.g. in cases of significant hyperopia), the test should also be performed through the correction. 3. Hold a penlight horizontally 1 m from the patient with the light aimed at the bridge of the patient’s nose. The back of the penlight should be very close to the tip of your nose. 4. Ask the patient to look at the light with both eyes open. Young children will automatically tend to look toward the bright light but may need a little encouragement. 5. Compare the colour and brightness of the fundus reflexes. 1. Hirschberg and Krimsky: Basing your decision upon the absolute position of a single reflex relative to the pupil centre rather than on a comparison of the relative locations of the corneal reflexes in the two pupils. 2. Not viewing the patient’s eyes from a position which is directly behind the penlight for the Hirschberg and Bruckner tests or from directly in front of the deviating eye in the case of the Krimsky test. 3. Placing too much emphasis on the accuracy of the estimates provided by these tests. 4. Not realising that these tests may fail to detect a small angle heterotropia. While the cover test must always be carried out, it is usual for this to be conducted prior to refraction and for other tests of oculo-motor alignment to be employed after the subjective refraction has been completed. The assessment of heterophoria requires that fusion is suspended and the eyes dissociated. This is achieved using vertical prism power which is too high for the eyes to overcome (von Graefe and Howell-card methods); viewing dissimilar images (a streak in one eye, a spotlight in the other as in the Maddox rod and modified Thorington tests) or using a septum (Maddox wing). Heterophoria tests are more repeatable with a trial frame than with a phoropter.12 In addition, since the use of a phoropter will limit the patient’s ability to adopt a habitually abnormal head position, the measurement of vertical phorias is best performed using a trial frame or a hand-held rod in free space. Because the cover test can be difficult to perform when using a phoropter or reduced aperture trial case lenses, all of the techniques described in this section offer advantages over the cover test for assessment of oculomotor alignment post-refractive correction. Also since the objective cover test can’t reveal small eye movements below about 2–3Δ, the subjective tests are useful for checking for small vertical heterophorias that may be clinically significant.4 The modified Thorington technique is a very simple and quick technique that can be used in a phoropter, trial frame or free space. It produces the most repeatable results of the most commonly used techniques.12–14 The modified Thorington overcomes the Maddox rod’s problem of lacking an accommodative target by using a target of small letters or numbers (Figure 6.4). It is principally used at near, but Thorington cards are available for both distance and near. In view of its many advantages it is somewhat surprising that it is not more widely used at present. Normative data from large study populations of children have been published.15 The Maddox wing provides a simple and relatively fast technique for the measurement of heterophoria at near. However, the figures used on the scale are relatively large with the result that accommodation does not need to be precisely controlled. This may lead to overestimation of an exo-deviation, to underestimation of an eso-deviation or to variable results. There are claims that changing to smaller letters improves test reliability.16 In addition, the eyes may not be fully dissociated because the septum may allow peripheral fusion to occur. Finally, the instrument uses a standard, fixed centration distance between the lenses and a fixed testing distance of 25 cm and it would be very difficult to use with a phoropter. The von Graefe technique is widely used and can be easily performed in a phoropter with a projector chart and no additional equipment. Unfortunately, it is the least reliable technique of those commonly available and its results correlate poorly with the cover test, especially in the case of horizontal phoria measures.12–14,17,18 This may result from variable amounts of prism adaptation, phoropter-induced proximal accommodation, a head tilt behind the phoropter leading to an induced vertical deviation or a reduction in peripheral fusion.12 In addition, it is a relatively lengthy procedure, can be difficult for patients to understand and cannot easily be used with a trial frame. The technique does not appear to warrant its widespread use and other more reliable techniques such as the modified-Thorington or Howell card methods should ideally replace it.12–14,17 The Howell card method provides a simple and quick technique that can be used in a phoropter, trial frame or free space and it can be used for measurement of horizontal phorias at distance or near. It cannot be used to measure vertical phorias. Although it appears to be popular, the method has not been subjected to many comparisons with other techniques but a study by Wong et al. suggests that the Howell phoria card method has a better inter-examiner repeatability than the von Graefe method.17 1. Inform the patient about the test: ‘This test is to check how your eye muscles work together with the new prescription’. 2. Measure near phorias immediately after the distance heterophoria measurements in pre-presbyopic patients and after inclusion of the required reading addition in presbyopes. 3. For near phoria measurement, adjust the trial frame/phoropter to the near centration distance. 1. Place the Maddox rod in front of one eye making sure that the ‘grooves’ are horizontal. Note that it is conventional to place the Maddox rod before the right eye. Dim the room lights. 2. Shine the light from a penlight through the central aperture of the Thorington near card. The near cards are usually calibrated for 40 cm and because the cards feature a tangent scale it is vital that the viewing distance is correct. 3. Direct the patient to look at the letters and keep them clear. Ask them to then look at the spotlight, and tell you whether the vertical red line is seen to the right, left or straight through the spotlight. 4. Some patients have difficulty seeing the red line initially. If they cannot see the red line, cover each eye in turn to demonstrate that one eye sees the spotlight, letters and numbers and the other sees the red line. Once they are aware of the test format they are often able to see the red line and spotlight, letters and numbers simultaneously. Placing a green filter before the eye viewing the spotlight can also help the patient to perform the test. If difficulty is still experienced, place the Maddox rod in front of the left eye and try again. If the spotlight and red line cannot be seen together then suppression may be present and follow up tests should be performed (section 6.13). 5. With the Maddox rod in front of the right eye the following responses may be given: (a) If the line is seen to pass through the spotlight the patient has no horizontal phoria. (b) If the line is to the left of the spotlight (crossed images) the patient has an exophoria. If the line is to the right of the spotlight (uncrossed images) the patient has an esophoria. (c) Determine the size of the deviation by asking the patient which number on the horizontal series of letters on the Thorington card the line passes through. This is the number of prism dioptres of horizontal heterophoria. 1. Rotate the Maddox rod so that the ‘grooves’ are vertical. 2. Ask the patient if the red line is seen above, below or straight through the spot. 3. With the Maddox rod in front of the right eye the following responses may occur: (a) If the line is seen to pass through the spotlight the patient has no vertical phoria. (b) If the line is above the spotlight the patient has a right hypophoria. It is possible to specify vertical heterophorias with respect to the right or left eye. Thus, a right hypophoria can also be called a left hyperphoria. As above, the size of the deviation is determined by asking the patient which number on the vertical series (number or letters) of letters on the Thorington card that the line passes through. 1. Ensure the patient is wearing their optimal near refractive correction and adjust the phoropter/trial frame to the near centration distance. 2. Ensure the card (Figure 6.5) is 33 cm away from the patient’s eyes. This is important because the tangent scale is calibrated for this exact distance. A piece of string of the appropriate length provides a simple means to establish that the viewing distance is correct. 3. Hold the stick-mounted or loose vertical prism in front of the right eye. This will generate vertical diplopia so the patient should see two scales and two arrows. The prism power used is 6Δ and it is introduced with base direction vertically oriented. 4. Ask the patient ‘Do you see two arrows and two sets of numbers?’ 5. Next ask the patient to do the following: ‘Please look at the top arrow and you will see it points downwards from the ‘0’ on the top set of numbers. Please follow it down with your eyes, and tell me which number on the lower set of numbers it points to. If it points between two numbers, please tell me between which two numbers it seems to point’. 6. Since the scale is a tangent scale, the number corresponds to the magnitude of the phoria. 7. Assuming the prism is placed base UP in front of the right eye, if the arrow points down towards an odd number, the patient is EXOphoric. If it points to an even number the patient is ESOphoric. Since the patient may extrapolate between two numbers, you should ask if the numbers appear on the yellow or blue part of the scale. Numbers on yellow are odd and those on the blue part of the scale are even. 1. Place the Maddox rod in front of the right eye making sure that the ‘grooves’ are horizontal. 2. Provide a spotlight target at distance using the wall/projector chart and then dim the room lights. 3. Ask the patient to look at the spotlight, and to indicate if the vertical (red) line is seen to the right, left or straight through the spotlight. 4. Some patients have difficulty seeing the red line initially. If this occurs, try the following: (a) Make sure that there are not other sources of light that will each produce a line image. (b) Cover each eye in turn to demonstrate to the patient that one eye sees the spotlight while the other sees the line. Once they are aware of the test format they are often able to see the line and spotlight simultaneously. (c) Placing a green filter before the eye viewing the spotlight may also help the patient perform the test, presumably because the brightness difference between the spot and streak is reduced relative to the normal white/red condition.
Assessment of Binocular Vision and Accommodation
6.1 Relevant Information From Case History and Assessments of Other Systems
6.1.1 Observations and symptoms
6.1.4 Birth history
6.1.5 Binocular visual acuity
6.1.6 Retinoscopy and subjective refraction
6.2 the Cover Test
6.2.1 Comparison of tests
6.2.2 Procedure
6.2.3 Adaptations to the standard procedure
![]() . In such cases the possibility of an alternating heterotropia should be investigated. Note that patients with a marked difference in VA between the eyes will not alternate. With an alternating heterotropia, the right eye will exhibit the tropia if the left eye fixates during the cover test and the left eye will exhibit the tropia if the right eye fixates during the cover test. The difficulty with diagnosing an alternating tropia is that the tropia movement only occurs during the first cover/uncover assessment. When the cover/uncover assessment is repeated a second and third time, the eye being observed does not now move as it has now become the fixating eye. The other eye has now become the deviating eye and the tropia will appear in the first cover/uncover assessment of the other eye. When asked to view binocularly after completion of the cover/uncover test, some patients with an alternating heterotropia will continue to fixate with the eye that fixated the target during the last iteration of the cover test procedure. In some cases, there is no preferred fixating eye. In other cases, there is a definite preference for fixation with one eye over the other and although the non-preferred eye might continue to fixate for a short period (e.g. a few seconds) after the cover had been removed, fixation then switches back to the preferred eye. Some patients with alternating tropia can switch eyes at will if you ask them to and some may even anticipate which eye is to be covered and switch eyes prior to you using the occluder. These tropias can be very confusing to diagnose.
. In such cases the possibility of an alternating heterotropia should be investigated. Note that patients with a marked difference in VA between the eyes will not alternate. With an alternating heterotropia, the right eye will exhibit the tropia if the left eye fixates during the cover test and the left eye will exhibit the tropia if the right eye fixates during the cover test. The difficulty with diagnosing an alternating tropia is that the tropia movement only occurs during the first cover/uncover assessment. When the cover/uncover assessment is repeated a second and third time, the eye being observed does not now move as it has now become the fixating eye. The other eye has now become the deviating eye and the tropia will appear in the first cover/uncover assessment of the other eye. When asked to view binocularly after completion of the cover/uncover test, some patients with an alternating heterotropia will continue to fixate with the eye that fixated the target during the last iteration of the cover test procedure. In some cases, there is no preferred fixating eye. In other cases, there is a definite preference for fixation with one eye over the other and although the non-preferred eye might continue to fixate for a short period (e.g. a few seconds) after the cover had been removed, fixation then switches back to the preferred eye. Some patients with alternating tropia can switch eyes at will if you ask them to and some may even anticipate which eye is to be covered and switch eyes prior to you using the occluder. These tropias can be very confusing to diagnose.
6.2.5 Recording
 for horizontal orthophoria,
for horizontal orthophoria,  for vertical orthophoria and
for vertical orthophoria and  for both vertical and horizontal orthophoria) only if no movement was detected using the cover test AND no phi movement was reported.
for both vertical and horizontal orthophoria) only if no movement was detected using the cover test AND no phi movement was reported.
6.2.6 Interpretation
![]() .
.
6.2.7 Most common errors
6.3 Other Tests for the Detection and Measurement of Heterotropia
6.3.1 Comparison of tests
6.3.2 Procedure: Hirschberg and Krimsky
6.3.3 Procedure: Bruckner test
6.3.6 Most common errors
6.4 Other Tests for the Detection and Measurement of Heterophoria
6.4.1 Comparison of tests
6.4.2 Initial procedure for all tests
6.4.3 Procedure: Modified Thorington test
Vertical near heterophoria
6.4.4 Procedure: Howell cards
6.4.5 Procedure: Maddox rod
![]()
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree