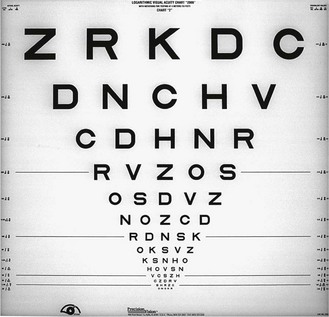
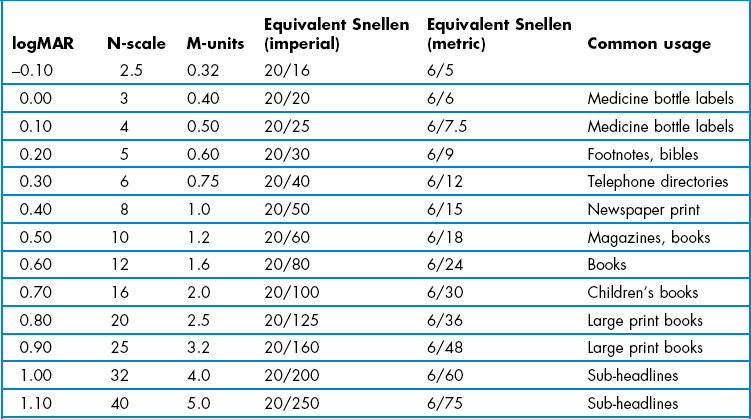
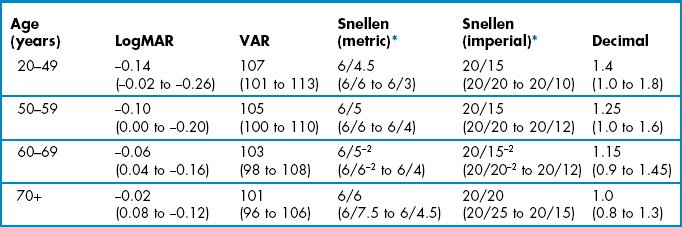
3 3.1 Differential diagnosis information from other assessments 3.3 Near visual acuity (and near vision adequacy) 3.4 Central visual field screening 3.5 Central visual field analysis 3.6 Peripheral suprathreshold visual field screening 3.7 Central 10 degree visual field analysis 3.8 Visual field assessment for drivers 3.9 Gross visual field screening 3.14 Potential vision assessment 3.15 Assessment of macular function 3.2.1 When should distance visual acuity be measured? There are three principal measures of VA: • Unaided VA, often called vision. • Habitual VA, with the patient’s own spectacles. • Optimal VA, with the best refractive correction, i.e. after subjective refraction. VA after objective refraction is also often recorded. Either vision and/or habitual VA should be measured immediately after the case history for legal reasons, to document the VA level prior to your examination. Habitual and optimal distance VA are routine measurements. Measuring distance unaided VA (vision) is optional, and should be measured with patients who: • have lost/broken their spectacles so that you cannot measure habitual VA; • do not wear spectacles for some distance viewing tasks (this information must therefore be obtained in the case history); • require the information for a report; • wear their spectacles all the time for distance and yet you suspect they may not need to (does the young low hyperope need to wear the spectacles for distance tasks?) LogMAR visual acuity (VA) charts (Figure 3.1) use the design principles suggested by Bailey and Lovie, including 0.1 logMAR progression of letter size from −0.3 to 1.0 logMAR (equivalent to 6/3 to 6/60 or 20/10 to 20/200), five letters per line, letters of similar legibility and per-letter scoring.1 Snellen charts were devised by the German ophthalmologist Hermann Snellen in 1862 and have been widely used ever since. There is not a standard Snellen chart and the letter size sequences, number of letters and/or numbers, varieties of letters, etc., vary from manufacturer to manufacturer. They typically contain one letter at a VA level of 6/60 (20/200; 0.1 logMAR) and increasing number of letters at smaller letter sizes with a typical bottom line of about 6/5 or 20/15 (~ −0.1 logMAR). The majority of Snellen charts have only one 6/60 or 20/200 letter, two 6/36 or 20/125 letters and three 6/24 or 20/80 letters. LogMAR charts typically have five letters on each of these lines and additional lines of letters at 6/30 or 20/100 (0.70 logMAR) and 6/48 or 20/160 (0.90 logMAR). Most logMAR charts have a ‘bottom line’ of −0.3 logMAR (6/3 or 20/10), whereas many Snellen charts have a bottom line of 6/5 or 20/15 and thus provide truncated data given that the average visual acuity of a young adult is about 6/4 (Table 3.1).2 Table 3.1 Normal age-matched visual acuity data for various notations.2 The average is shown with 95% confidence limits in brackets LogMAR charts are widely recognised as providing the most reliable and discriminative VA measurements and are standard for clinical research or clinical trials of ophthalmic devices or drugs.3,4 Visual acuity measurements using a logMAR chart have been shown to be twice as repeatable as those from a Snellen chart and over three times more sensitive to inter-ocular differences in VA and therefore substantially more sensitive to amblyopic changes for example.3,5 The Bailey–Lovie or ETDRS charts are the most commonly used logMAR charts for adults and the Glasgow Acuity Cards (commercially available as the Keeler logMAR crowded charts) have been designed specifically for children.4,5 1. Ensure the chart is at the appropriate distance and is calibrated correctly. 2. Leave the room lights on and illuminate the chart. The luminance of the chart should be between 80 and 320 cd/m2. Seat the patient comfortably with an unobstructed view of the test chart. You should sit in front and to one side of the patient in order to monitor facial expressions and reactions. 3. If you are going to measure both vision and habitual VA, measure vision first to avoid memorisation. To measure vision, ask the patient to remove any spectacles. To measure habitual visual acuity, ask the patient to put their distance vision spectacles on. 4. Measure the visual acuity of the ‘poorer’ eye first, if a poorer eye is known from previous records or from the case history (to avoid a patient memorising the letters seen with the better eye and giving a false visual acuity with the poorer eye. Note that this can be avoided with computer-based charts by randomising the letters prior to measurement). Otherwise, measure VA in the right eye first. 5. Explain what measurement you are about to take. This can be as simple as ‘Now we shall find out what you can see in the distance’. 6. Instruct the patient: ‘Please cover up your left/right eye with the palm of your hand/this occluder’. If using the patient’s hand, make sure that the palm is being used as otherwise the patient may be able to peek through their fingers. Some clinicians prefer to hold the occluder over the patient’s eye themselves to ensure it is properly occluded. 7. Ask the patient: ‘Please read the smallest line that you can see on the chart’ or similar. 8. Continually monitor the patient’s facial expressions and head position. Do not permit the patient to screw their eyes up or look around the occluder or through their fingers. 9. Once the patient has reached what they believe are the smallest letters they can see, they should be pushed to determine whether they can see any more. Use prompts such as ‘Can you see any letters on the next line?’ or ‘Have a guess. It doesn’t matter if you get any wrong’. Some patients are more cautious than others and only indicate those letters that they can see easily and clearly. Unless you push patients to guess, you could obtain different VA results depending on how cautious your patient is. Ideally, you should stop pushing patients to read more if they make four or more mistakes on a line of five letters.6 10. If the patient cannot see the largest letters on the chart, ask them to move closer to the letter until two or three lines can be seen (or use a printed panel chart at a reduced distance). The distance at which this occurs should be noted. This is a more accurate assessment than determining the position that the patient can ‘count fingers’.7 If the patient cannot see the letters even at the closest test distance, use the following test sequence. Stop at the level at which the patient can accurately respond. (a) Hand movements (HM) @ Y cm: The patient can see a hand moving from a certain distance. Some computerised VA tests can provide accurate measurements down to the hand movements level and these should be used when available.7 (b) Light projection (Lproj.): The patient can report which direction light is coming from when you hold a penlight about 50 cm away. Ask the patient to point to the light and note the areas of the field in which the patient has light perception. (c) Light perception (LP): The patient can see the light but not where it is coming from. If they cannot see light, the vision is recorded as no light perception or NLP. Amblyopia can be missed if single letters are used rather than a letter chart because of the lack of contour interaction. Ideally logMAR-based charts with contour bars at the end of lines, such as the logMAR crowded charts, should be used when measuring VA in children (Figure 3.2).8 The logMAR crowded charts have been shown to be over three times more sensitive to inter-ocular differences in VA than single letter Snellen charts and therefore substantially more sensitive to amblyopic changes.5 Crowded and standard and logMAR charts can even be used in children who do not know their letters by providing them with a key card that includes a selection of the letters from the chart. You then point to a letter on the chart and ask the child to identify the letter on their key card. For children that are unable to use a key card, charts are now available in logMAR format that include pictures rather than letters (Figure 3.2), such as the Kay crowded picture test, which has been shown to provide comparable results to the logMAR crowded charts.9 VA measurements can be scored in logMAR notation, using the visual acuity rating (VAR) score or converting scores to an equivalent Snellen value. Computer-based systems will typically convert VA values for you. LogMAR or VAR could be used on your own record cards. However, equivalent Snellen values should generally be provided when writing referral letters and reports, as Snellen notation is universally understood, whereas logMAR is not at present. In all cases, it is preferable to score using a by-letter system rather than measuring the lowest line at which the majority of letters were correctly read as it provides more repeatable and discriminative measurements.10 Comparisons of various logMAR scores with Snellen and other recording notations are shown in Table 3.2. Table 3.2 Distance visual acuity conversion table MAR, minimum angle of resolution; VAR, visual acuity rating. The fact that logMAR VAs better than 6/6 or 20/20 are negative is counterintuitive. The VAR score provides a simpler method for scoring logMAR charts. VAR = 100 − 50 logMAR. Therefore 0.00 logMAR = 100 VAR and each letter has a score of 1. For example if a patient reads all the letters down to the 100 row and gets one letter wrong on this row, their score is 99, two letters wrong 98, etc. If they read all of the letters on the 100 row and one letter on the row below, their score is 101, two letters on the line below 102, etc. A disadvantage of the VAR score is that it suggests that 100 (6/6) is normal VA, which is far from true for many patients with healthy eyes.2 The Snellen fraction is defined as: Test Distance/Distance at which the letters subtend 5 min of arc. Test distance can be provided in metres (typical 6m) or feet (typically 20 feet). Snellen VA can be labelled in either decimal or conventional Snellen notation (see Table 3.2 for comparison). Vision or visual acuity is recorded as the smallest line in which the majority of the letters are seen, irrespective of subjective blur. Errors are recorded by appending a minus one, two or three to the Snellen fraction or decimal notation. If additional letters are seen on the following line, the Snellen fraction or decimal notation can be appended by a plus (usually up to no more than 3). If the patient could not see the 6/60 letter at 6 m, but could at 2 m, record 2/60. Similarly if the patient could not see the 20/200 letter at 20 feet, but could see the 20/120 letter at 5 feet, record 5/120. Vision or ‘VA s Rx’ or VAsc or Vsc all mean visual acuity measured without a correction. VAs are recorded for the right eye (RE or OD), left eye (LE or OS) and binocular (BE or OU). This last example is given in decimal format, which is commonly used in parts of Europe. It should not be confused with logMAR. Any deviation from normal age-matched results, as shown in Table 3.1, should be noted. Note that the average VA for patients less than 50 is about −0.14 logMAR (6/4.5, 20/15) and that 6/6 or 20/20 represents reduced VA for the vast majority of patients. 6/6 or 20/20 only becomes the average VA for patients over 70 years of age with healthy eyes. You must also check whether there has been any change in VA from the previous examination. In patients with normal or near normal VA, a significant change in VA is more than 0.1 logMAR or one line.5,11 Also note any inter-ocular asymmetry of a line or more, or a binocular result that is worse than the monocular response.5 By comparing vision and optimal VA or habitual and optimal VA and using the one line of VA is equivalent to −0.25DS rule, an estimate of the mean spherical correction can be gained (section 4.1.5). If this estimate is widely different from the actual subjective refraction result, an error may be suspected and the subjective (and/or spectacle power) rechecked. 1. Allowing cautious patients to decide their acuity (i.e. not pushing them to guess). 2. Permitting the patient to screw their eyes up and improve their VA. 3. Permitting the patient to look around the occluder or through their fingers and view binocularly when measuring monocular VA. 4. Not recording the result immediately and guessing the result at the end of the examination. 5. Forgetting that patients could have VA better than your bottom line (of typically 6/5 or 20/15 with some Snellen charts). Near vision cards typically present sentences or paragraphs of words rather than isolated letters and can incorporate examples of near vision tasks such as sheet music, technical drawings and telephone directories (Figure 3.3). They are also now available on e-tablet and e-phones. There are five main types of notations used to measure near VA: logMAR, N-point, M-scale, equivalent Snellen, and Jaeger. LogMAR near charts have all the advantages of distance logMAR charts (section 3.2.2) and should be used whenever an accurate, non-truncated measurement of near VA is needed and particularly when distance VA and near VA may differ, such as with multifocal implants/contact lenses and patients with subcapsular cataract. Some near logMAR charts use isolated letters rather than words, but word charts are preferred, particularly in patients with conditions such as age-related macular degeneration as it relates better to reading performance and is typically worse than near letter VA.12 N-point uses the Times New Roman font and is the standard test in the UK and Australia. It is based on the ‘point size’ used by printers and word processing packages on modern computers, in which 1 point = 1/72 inch (~0.353 mm). This can be a useful aid when indicating to a patient the level of vision that would be provided for computer use by new lenses. N8 is approximately equal to 1.0 M and this eight times conversion holds for all print sizes. M-units are widely used in North America and indicate the distance in metres at which the height of a lower case ‘x’ subtends 5 minutes of arc. A 1.0 M letter ‘x’ is therefore 1.45 mm high. Equivalent Snellen notation is a confusing notation, especially when near VAs are not measured at the standard 16′: What does 20/20 near VA at 8′ mean? In addition, near vision adequacy should indicate what patients can see at their own near working distance, not an arbitrary standard of 16′ (working distances for reading in patients with normal vision range from 10′ to 20′13). Cards using Jaeger notation should not be used as there is no standardisation of what J1 or J5, etc., means and different charts can give totally different sizes of print with the same J-value. 1. Sit in front and to one side of the patient in order to monitor facial expressions and reactions. 2. Measurements should be made in similar lighting conditions to those the patient uses at home. Ask if the patient uses an anglepoise or goose-neck light at home, and if they do, use additional light for your near VA measurements. 3. Instruct the patient to place the near vision card (or e-tablet, e-phone or e-book reader) at their normal near working distance. Measure and record this distance. 4. Measure the near VA of the ‘poorer’ eye first, if a poorer eye is known from previous records or from the case history. Otherwise, measure the right eye first. Use an occluder or the patient’s palm of their hand to cover the other eye. If using the patient’s hand, make sure that the palm is being used as otherwise the patient may be able to peek through their fingers. 5. Explain to the patient what measurement you are about to take. This may be a simple: ‘Now we shall find out what you can see at close distances’. 6. Instruct the patient to read the smallest paragraph they can. 7. Unless the patient can see the smallest print, push them to determine whether they can see anymore. Prompts such as ‘Try and make out some of the words in the smaller paragraph’ may be useful. Some patients are more cautious than others and only indicate those letters that they can see easily and clearly. Unless you push patients to guess, you could therefore obtain different near VA results depending on how cautious your patient is. You should have asked the patient whether they use additional lighting, such as an anglepoise or goose-neck light, to read in their home. If they do not and you subsequently find they cannot easily read N5 (or 0.4 M) at the end of the reading addition part of the refraction, they should be encouraged to obtain additional light for near tasks in their home. It is very useful to demonstrate how helpful such additional light can be. The main objective of people with vision impairment is to be able to read and a majority can be successfully helped in primary eye care using high reading additions, simple magnifiers and additional lighting.14 Note that although near VA levels can be associated with a range of near tasks (Table 3.3), the poorer near VAs are threshold measurements (measurements of N5, 0.4 M and 20/20 may be truncated and not thresholds as discussed earlier) so that patients would not be able to read print of that size comfortably for any length of time. For example, to allow somebody to read newspaper print comfortably requires a near VA better than N8 or 1.0 M which is the typical size of newspaper print (Table 3.3) as a ‘reading reserve’ of 2 : 1 is needed and a near VA of N4 or 0.5 M.15 Note the working distance and then record the smallest paragraph size seen by the right and left eyes and binocularly. For approximate equivalents to other notations see Table 3.3. Some clinicians do not note the working distance unless it is different from the ‘norm’. However, even patients with good vision present a wide range of normal working distances (22 cm to 50 cm for reading,13 and further away for computer use), and as stated earlier a reading acuity is meaningless without a working distance. It can also be useful to record the working distance(s) used to determine near VA with the patient’s own spectacles to allow a comparison with the one used to determine the reading add. This can also be useful for comparison if patients return to your practice dissatisfied with the near vision in any new spectacles. These cases are often due to problems with working distance determination rather than an incorrect refraction. When determining a reading addition, do not assume you have the correct add just because a patient can see the smallest text on your near chart such as N5, 0.4 M or 20/20. At 40 cm 0.4 M is equivalent to about 20/20 or 6/6 distance VA and N5 is equivalent to 6/9 or 20/30. Therefore, a patient could have reduced distance VA and still read N5, 0.4 M or 20/20 at near. Apart from this truncation effect, near VA can be expected to be similar to distance VA in most cases provided that the eye is accommodating normally or that the reading addition is correct. Notable exceptions include patients with multifocal intra-ocular lenses (IOLs) or wearing multifocal contact lenses or patients with posterior sub-capsular cataract. Patients with some eye disorders, such as amblyopia, age-related macular degeneration (ARMD) and macular oedema, can have significantly worse reading VA than distance VA and isolated-letter near VA.12 Perimetry enables the assessment of visual function throughout the visual field, the detection and analysis of damage along the visual pathway, and the monitoring of disease progression. Central visual field analysis using standard automated perimetry (SAP) can be a lengthy procedure and quicker and simpler techniques can be used for screening the central visual field. Central visual field screening should not be performed on patients with minimal risk factors (such as patients over 40 years of age without other risk factors, high myopes) due to the problems of false positive results when testing healthy patients (section 1.2).16 For example, the most commonly used screening programme for Frequency Doubling Perimetry is the N-30-5. The −5 in the programme title indicates that there is a 5% chance of a positive test being from a patient with a normal visual field, so that specificity is set at 95%. With a POAG prevalence of about 2%; out of 1000 patients, 20 would have POAG, but 980 would be healthy and 5% of them (49) would have a positive test result (49 false positives, ~72% of those with a positive result). Central visual field screening can be considered for patients who are asymptomatic with minor risk factors, such as patients with normal looking discs and intra-ocular pressures (IOP) but who have a primary family history of glaucoma, or who over 75 years, or over 30 years of age and black (African Caribbean, African American) where the prevalence of POAG is higher and false positives less of an issue (section 1.2).16 This is particularly true when positive tests are repeated. For patients exhibiting significant risk factors for glaucoma (abnormal appearing discs, high IOP), neurological disease, certain types of retinal disease or symptomatic patients, it is more appropriate to perform a central visual field analysis rather than use a screening technique. The speed and accuracy of contemporary fast threshold estimation strategies have made several of the traditional screening techniques somewhat redundant. Fast thresholding strategies can produce an estimation of visual field sensitivity in a time (2.5–4 minutes per eye) similar to single stimulus, suprathreshold screeners. All of the fast central field analysis techniques have the advantage over suprathreshold screening techniques in that they are better able to detect early visual field defects, and can give an idea of defect depth and area. They have the disadvantage of taking longer than some suprathreshold techniques. They are similar in sensitivity and specificity for glaucoma as frequency doubling perimetry, but much better at detecting other types of visual field defect.17,18 When compared to techniques for full central field analysis they are quicker but less precise and with worse test-retest characteristics.19 The Humphrey Field Analyser (HFA) II, SITAFast (Swedish Interactive Thresholding Strategy), Central 24-2 tests 58 locations over the central 25° in a 6° grid pattern that straddles the horizontal and vertical mid-lines, i.e. targets are located 3° either side of the mid-lines. In addition there are targets located on the nasal field between 25° and 30°. The SITAFast, 24-2 programme rarely takes more than 3.5 minutes in a normal patient, and can be as quick as 2.5 minutes. Most modern perimeters have similar fast thresholding central visual field programmes. 1. Explain the test and the reasons for performing the assessment to the patient. 2. When performing visual field screening pupils should be 3 mm or greater, whenever possible. It is considered acceptable to perform visual field testing whilst a pupil is dilating, provided the pupil is at least 3 mm at the start of the test. Note the position of the upper lid (i.e. possible blepharoptosis or dermatochalasis) and consider taping if it is obstructing the field of view. 3. Reduce ambient illumination and turn on the instrument. 4. For most visual field screeners: Contact lens wearers should perform the visual field test in their lenses. This is particularly useful for aphakes and high ametropes. Full aperture trial case lenses should otherwise always be used. Reduced aperture lenses and masked cylindrical lenses (i.e. those with opaque masks running along the direction of the axis) can result in visual field artefacts. Similarly bifocal and progressive addition glasses and those with small frames should be avoided. Best sphere should be used for any cylinder less than 1.50 D. If the cylinder is greater than 1.50 D then place the appropriate spherical lens in the back cell of the lens holder and the cylindrical lens in the cell immediately in front of the sphere. You should use a translucent occluder if the patient has latent nystagmus. 5. Seat the patient at the instrument and adjust the height of the instrument to ensure patient comfort. Over-extension of the neck and a bent back with hunched shoulders and neck should both be avoided. 6. Select ‘Central 24-2’ and then subsequently select ‘Change Parameters’ and ‘Test Strategy’ to ensure ‘SITAFast’ is used. 7. Select the eye to be tested first, and unless otherwise indicated select ‘Right’. 8. Enter the patient ID. Let the patient adapt to the bowl luminance while entering the data. This is a very important but frequently overlooked procedure, as it ensures a consistent level of retinal adaptation over the duration of the test. Enter as much patient data as possible but always include patient name using the surname first, date of birth (this is often formatted as month-day-year) and patient file number if appropriate. It is often useful to enter the prescription lenses used and pupil size. It is also possible to enter a diagnostic code, VA, IOP and cup-to-disc ratio. 9. Occlude the left eye and give the patient the response button. 10. Place the patient’s head in the headrest. Explain the test to the patient: ‘I want you to keep looking at the yellow light in the middle of the bowl. When you see a light flashing off to the side of the yellow light, please press this button. There will be times during the test when you will not be able to see any lights flashing and this is normal. Remember to keep looking at the yellow light in the middle of the bowl all the time’. 11. Align the patient using the video eye monitor. 12. Ensure that the vertex distance of the trial lens is adjusted appropriately and the trial lens is centred in front of the eye. 13. Select ‘Demo’ for a naive patient. Repeat until you are happy that the patient understands the procedure. 15. Some models will have a Gaze Monitoring feature. Once initialised, select ‘Start’. 16. Monitor fixation, check that the patient’s forehead has remained touching the rest and encourage the patient throughout the test. Use phrases such as ‘you are doing well’, ‘over half way now’, ‘keep looking straight ahead…that’s good’ or ‘you’ve nearly finished’. Do not leave the patient unattended. 17. When the test is completed, store the result on disk then select ‘Test Other Eye’. Occlude the patient’s right eye and align the left eye with the appropriate correction having been placed in the lens holder. 18. When the left eye is completed, store the results on disk and print the results if required. If no test locations are highlighted on the Total and Pattern Deviation probability plots then record ‘SITA-Fast: WNL (within normal limits) R and L’. If there is a field defect, repeat the test, print and store both fields of both eyes and attach to the record card. SITA-Standard (or equivalent) could be used instead of SITA-Fast for the repeated field. The single field analysis of the repeated field should accompany any referral to the secondary eye care system. The single field analysis printout illustrates the data as an interpolated greyscale, raw data in decibels, and Total and Pattern deviation plots. It also summarises the field using the Glaucoma Hemifield Test, Global Indices, Reliability Indices, and Gaze Tracking plots (section 3.5.4). These are interpreted in exactly the same way as the strategies for full central field analysis (section 3.5.4). It is important to be aware of the possible causes of artefact in cases where it would appear that a new defect has been detected, particularly in a patient with no previous experience of visual field screening or no history of field loss. A new defect is not a defect until it is repeated, ‘if in doubt always repeat’. The effect of learning and fatigue can be dramatic.20 Note that when the Glaucoma Hemifield Test classifies the field as having a ‘general reduction of sensitivity’, the Mean Defect/Deviation is abnormal and/or the Total Deviation probability plot shows a majority of test locations as being outside of normal limits, care should be taken when interpreting the results. There is usually an obvious clinical reason, with the most likely association being with cataracts or small pupils. 1. Using an inappropriate spectacle or lens type. 2. Poorly aligning the patient. 3. Providing poor patient instruction: It is worth investing time to ensure that the naïve patient understands what is expected of them. If necessary, repeat the test until you are satisfied that the patient has performed adequately. 4. Failing to encourage and communicate with the patient. The most commonly used perimeter and programmes for central visual field analysis is the Humphrey Field Analyser (HFA) SAP programmes 30-2 and 24-2. The 30-2 programme tests 76 locations over the central 30° in a 6° grid pattern that straddles the horizontal and vertical mid-lines, i.e. targets are located 3° either side of the mid-lines.21 Equivalent programmes can be found on most perimeters. The 24-2 programme examines the central 25°, with the addition of more peripheral targets in the nasal step region, and consequently testing time is reduced by up to 20% compared to the 30-2 strategy. It is often used in follow-up assessments and to lessen the likelihood of any fatigue effect. Analysis of the central visual field should be performed on all patients with: • Significant risk factors for glaucoma (compare with section 3.4) including, but not limited to, combinations of IOP >21 mmHg, old age, family history, narrow angles, vertical elongation of the optic nerve head, notching of the neural rim tissue of the optic nerve head, disc haemorrhage, nerve fibre layer defect, exfoliative syndrome, pigment dispersion, optic nerve head asymmetry. • Abnormal screening test (e.g. positive screening test, confrontation or Amsler). • Symptoms consistent with neurological disease (for example, headache including migraine, dizziness, tingling of limbs) or neuro-ophthalmic disease. • Symptoms consistent with central field loss, e.g. non-refractive reduced vision, positive scotoma, scintillating scotoma. In addition threshold fields are always required when monitoring a known defect, and they should always be included in protocols for the management of glaucoma. The instrument should be capable of monitoring fixation, providing full threshold fields in less than 8 minutes, providing reliability indices and analysing the results. A rapid threshold estimation algorithm, such as the HFA’s SITAStandard or the Octopus Dynamic Strategy is recommended. These strategies take approximately 7 to 9 minutes per eye, without compromising the accuracy or repeatability of the result.22,23 The use of faster, less repeatable, thresholding strategies (e.g. HFA SITAFast and Octopus TOPs; section 3.4) may be considered as an alternative for some patients with a demonstrated history of fatigue. There has been discussion that SITA should not be used in patients suspected of conditions other than glaucoma as they are optimised specifically for glaucoma. However, clinically the advantage of the reduced test time makes such a compromise worthy of consideration, and no evidence has been presented that suggests a reduction in diagnostic capability for non-glaucomatous defects. The procedure for central visual field analysis is the same as that for central visual field screening (section 3.4.2) except that: • At the ‘Main Menu’ select ‘Central 30-2’ (or ‘Central 24-2’). • Select ‘Change Parameters’, followed by ‘Test Strategy’ and ensure ‘SITAStandard’ is selected. If a full threshold strategy is considered appropriate, select ‘Full Threshold’. • If false negative catch trials are noted, advise the patient to rest by keeping the response button pressed down which will pause the test. • If false positive catch trials are noted, pause the test by keeping the response button pressed down and re-instruct the patient.
Assessment of visual function
3.1 Differential diagnosis information from other assessments
3.2 Distance visual acuity
3.2.2 LogMAR versus Snellen
3.2.3 Procedure
3.2.4 Alternative procedures to assess VA in children
3.2.6 Recording for logMAR and Snellen charts
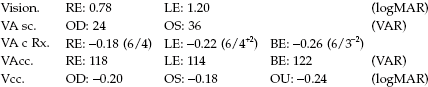
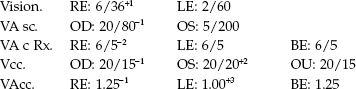
3.2.7 Interpretation
3.2.8 Most common errors
3.3 Near visual acuity (and near vision adequacy)
3.3.1 Comparison of different near vision charts
3.3.2 Procedure: logMAR near VA and M or N-notation near vision adequacy
3.3.3 Adaptation for older patients
3.3.4 Recording
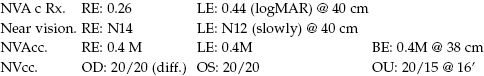
3.3.5 Interpretation
3.4 Central visual field screening
3.4.1 Comparison of tests
3.4.2 Procedure
3.4.3 Recording
3.4.4 Interpretation
3.4.5 Most common errors
3.5 Central visual field analysis
3.5.1 Comparison of tests
3.5.2 Procedure
Assessment of visual function