Figure 7-1 Schematic representation of an eye undergoing conductive keratoplasty, which delivers radiofrequency energy to the cornea through a handheld probe inserted into the peripheral cornea. (Courtesy of Refractec, Inc.)
For the treatment of hyperopia, the surgeon inserts the tip into the stroma in a ring pattern around the peripheral cornea. The number and location of spots determine the amount of refractive change, with an increasing number of spots and rings used for higher amounts of hyperopia. The CK procedure is performed using topical anesthesia and typically takes less than 5 minutes. The collagen shrinkage leads to visible striae between the treated spots, which fade with time (Fig 7-2).
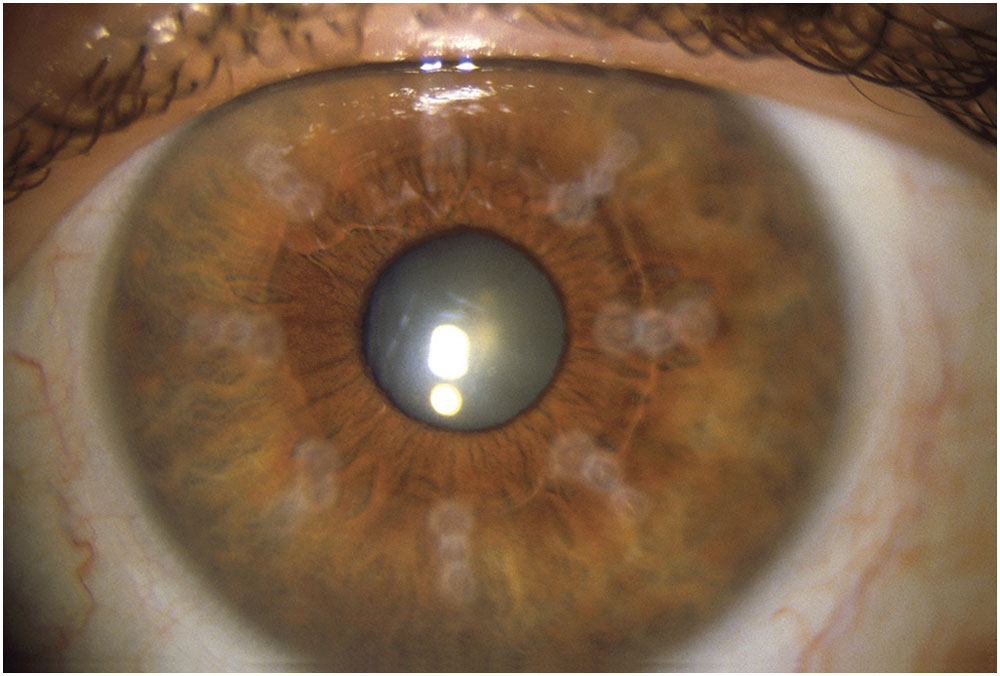
Figure 7-2 One month after a 24-spot conductive keratoplasty treatment in a patient with +2.00 D hyperopia, the spots are beginning to fade. Three sets of 8 spots each were applied at a 6.0-, 7.0-, and 8.0-mm optical zones. (Courtesy of Refractec, Inc.)
Patient selection
The Refractec system is FDA approved for the temporary reduction of spherical hyperopia in patients 40 years or older with a spherical equivalent of +0.75 to +3.25 D and ≤0.75 D of astigmatism. The treatment is not advised for use in patients who have undergone radial keratotomy, and it is not FDA approved for use in patients with keratoconus, ectatic disorders, or significant irregular astigmatism. An upper limit of +1.50 D (spherical equivalent) appears to be the current treatment ceiling for this technology, and repeat applications over time or increased number of spots does not seem to enhance or increase that limit.
Safety
In the principal FDA clinical trial to date, no patient had a worse outcome than 20/40 visual acuity, and none lost more than 2 lines of vision. One patient of a total of 391 had >2.00 D of induced cylinder, and no patient with a preoperative corrected distance visual acuity (CDVA; also called best-corrected visual acuity, BCVA) of ≥20/20 had <20/25 at 1 year. Although induced cylinder of >2.00 D is an FDA safety variable, smaller amounts of induced cylinder were apparent. At 1 year, 6% of patients had >1.00 D of induced cylinder. The magnitude of the induced cylinder decreased with time. No central corneal haze was noted at 12 months, and endothelial cell counts were similar before and after the study.
Results
The clinical trial included 12-month data for 401 eyes; mean cohort age was 55.3 years (range, 40.2–73.9 years). The mean cycloplegic spherical equivalent was +1.86 ± 0.63 D. By 12 months postoperatively, 92% of study patients had achieved uncorrected distance visual acuity (UDVA; also called uncorrected visual acuity, UCVA) of 20/40 or better, 74% achieved 20/25 or better, and 54% had 20/20 or better. By 24 months postoperatively, 93% of study patients had achieved UDVA of 20/40 or better, 76% achieved 20/25 or better, and 52% had 20/20 or better. There was a slow, continued drift toward increasing hyperopia, with regression of +0.21 D and +0.48 D at 12 and 24 months, respectively. Overall, there was a 20% loss of effect after 2 years. This loss of effect is probably a combination of true regression and the normal hyperopic drift that occurs as people age. The results in the FDA CK trial for presbyopia were similar.
Despite initial reports of refractive stability, long-term follow-up has revealed regression and/or lack of adequate effect with CK. In a long-term (mean, 73.1 months; range, 44–90 months) follow-up of patients enrolled in the phase 3 multicenter trial of CK, Ehrlich and Manche found nearly complete regression of treatment effect in the 16 eyes (of the original 25 eyes) available for follow-up.
Ehrlich JS, Manche EE. Regression of effect over long-term follow-up of conductive keratoplasty to correct mild to moderate hyperopia. J Cataract Refract Surg. 2009;35(9): 1591–1596.
Hersh PS. Optics of conductive keratoplasty: implications for presbyopia management. Trans Am Ophthalmol Soc. 2005;103:412–456.
Kymionis GD, Kontadakis GA, Naoumidi TL, Kazakos DC, Giapitzakis I, Pallikaris IG. Conductive keratoplasty followed by collagen cross-linking with riboflavin-UV-A in patients with keratoconus. Cornea. 2010;29(2):239–243.
McDonald MB. Conductive keratoplasty: a radiofrequency-based technique for the correction of hyperopia. Trans Am Ophthalmol Soc. 2005;103:512–536.
Other applications
Other potential off-label uses also exist for CK. In cases of overcorrected myopic LASIK and myopic photorefractive keratectomy (PRK), CK can be used to correct hyperopia. In these procedures, CK obviates the need to lift or cut another flap. In one report, CK was used to treat both keratoconus and post-LASIK ectasia. Although corneal irregularities improved immediately, with some improvement in visual acuity, some cases showed regression of effect at 1 month. Larger studies with additional follow-up are needed.
In postcataract or postkeratoplasty patients with astigmatism, CK can be used to steepen the flat axis, because each spot is individually placed. The overall effect is still a myopic shift, so CK is particularly useful when the spherical equivalent is hyperopic. In a study of 16 patients who had CK for hyperopia after cataract surgery, 1-year follow-up data showed that CK for low to moderate postcataract hyperopia was effective and safe.
Some surgeons have also used CK in combination with collagen crosslinking in an attempt to correct the corneal curvature abnormalities in keratoconus.
Conductive keratoplasty appears to have advantages both in cost and in allowing flexible (off-label) treatment patterns because the tip can be placed anywhere on the cornea. More experience and long-term data will be required to determine how important CK will be in the refractive surgeon’s armamentarium. Currently, however, its use remains fairly limited because of the high rate of refractive regression.
Alió JL, Ramzy MI, Galal A, Claramonte PJ. Conductive keratoplasty for the correction of residual hyperopia after LASIK. J Refract Surg. 2005;21(6):698–704.
Claramonte PJ, Alió JL, Ramzy MI. Conductive keratoplasty to correct residual hyperopia after cataract surgery. J Cataract Refract Surg. 2006;32(9):1445–1451.
Kolahdouz-Isfahani AH, McDonnell PJ. Thermal keratoplasty. In: Brightbill FS, ed. Corneal Surgery: Theory, Technique, and Tissue. 3rd ed. St Louis: CV Mosby; 1999.
Kymionis GD, Kontadakis GA, Naoumidi TL, Kazakos DC, Giapitzakis I, Pallikaris IG. Conductive keratoplasty followed by collagen cross-linking with riboflavin-UV-A in patients with keratoconus. Cornea. 2010;29(2):239–243.
Collagen Crosslinking
The corneal collagen crosslinking procedure combines riboflavin (vitamin B2), which is a naturally occurring photosensitizer found in all human cells, with ultraviolet A (UVA) light to strengthen the biomechanical properties of the cornea. Riboflavin alone has no crosslinking effect. Its function as a photosensitizer is to serve as a source for the generation of singlet oxygen and superoxide anion free radicals, which are split from its ring structure after excitation by the UVA irradiation and which then lead to physical crosslinking of the corneal collagen fibers. In the presence of riboflavin, approximately 95% of the UVA light irradiance is absorbed in the anterior 300 µm of the corneal stroma. Therefore, most studies require a minimal corneal thickness of 400 µm after epithelial removal in order to prevent corneal endothelial damage by the UVA irradiation. Thinner corneas may be thickened temporarily with application of a hypotonic riboflavin formulation prior to UVA treatment.
Although there may also be a slight flattening of the cornea, the most important effect of collagen crosslinking is that it appears to stabilize the corneal curvature and prevent further steepening and bulging of the corneal stroma. There is no significant change in the refractive index or the clarity of the cornea. The primary clinical application of collagen crosslinking is as a treatment to prevent the progression of keratoconus and post–corneal refractive surgery ectasia.
Corneal collagen crosslinking was first described by Spörl and colleagues in 1997. In the performance of this procedure, riboflavin solution is continually applied to the eye for 30 minutes (in most studies), and the riboflavin is then activated by illumination of the cornea with UVA light for 30 minutes, during which time application of the riboflavin solution continues. The corneal epithelium is generally removed before application of the riboflavin so that riboflavin penetration is increased. Alternative riboflavin formulations and crosslinking techniques that avoid epithelial removal are being evaluated and seem promising.
Corneal collagen crosslinking is approved for use in many countries but not currently in the United States. An FDA clinical trial evaluating collagen crosslinking for the treatment of keratoconus and corneal ectasia is ongoing. In one US clinical trial, all patients with either keratoconus or post-LASIK ectasia had their corneal epithelium removed, which was followed by a 30-minute application of riboflavin (0.1% diluted in 20% dextran) every 2 minutes, and a subsequent 30-minute UVA treatment (365 nm; 3 mW/cm2 irradiation), with concomitant administration of topical riboflavin as a photosensitizer (Fig 7-3). Two control groups—sham and fellow eye—were included in the study, and all patients were monitored for 1 year. Treated eyes initially showed a slight steepening of the cornea with a decrease in CDVA, followed by corneal flattening of approximately 1.00–2.00 D, which peaked at between 1 and 3 months after crosslinking. In addition to a reduction in corneal cylinder, a transient compaction of the cornea and an increase in CDVA were observed. There appears to be stabilization in most treated eyes. Some eyes may require re-treatment, and there have been rare cases of loss of 2 or more lines of best-corrected distance visual acuity in these studies, however.



