Figure 6-1 Wavefront analysis depicting higher-order aberrations after laser in situ keratomileusis (LASIK), including coma and trefoil. (Courtesy of Steven I. Rosenfeld, MD.)
Pallikaris IG, Kymionis GD, Panagopoulou SI, Siganos CS, Theodorakis MA, Pellikaris AI. Induced optical aberrations following formation of a laser in situ keratomileusis flap. J Cataract Refract Surg. 2002;28(10):1737–1741.
Tran DB, Sarayba MA, Bor Z, et al. Randomized prospective clinical study comparing induced aberrations with IntraLase and Hansatome flap creation in fellow eyes: potential impact on wavefront-guided laser in situ keratomileusis. J Cataract Refract Surg. 2005; 31(1):97–105.
Waheed S, Chalita MR, Xu M, Krueger RR. Flap-induced and laser-induced ocular aberrations in a two-step LASIK procedure. J Refract Surg. 2005;21(3):346–352.
Central Islands
A central island appears on computerized corneal topography as an area of central corneal steepening surrounded by an area of flattening that corresponds to the myopic treatment zone in the paracentral region (Fig 6-2). A central island is defined as a steepening of at least 1.00 D with a diameter of >1 mm compared with the paracentral flattened area. Central islands may be associated with decreased visual acuity, monocular diplopia and multiplopia, ghost images, and decreased contrast sensitivity.
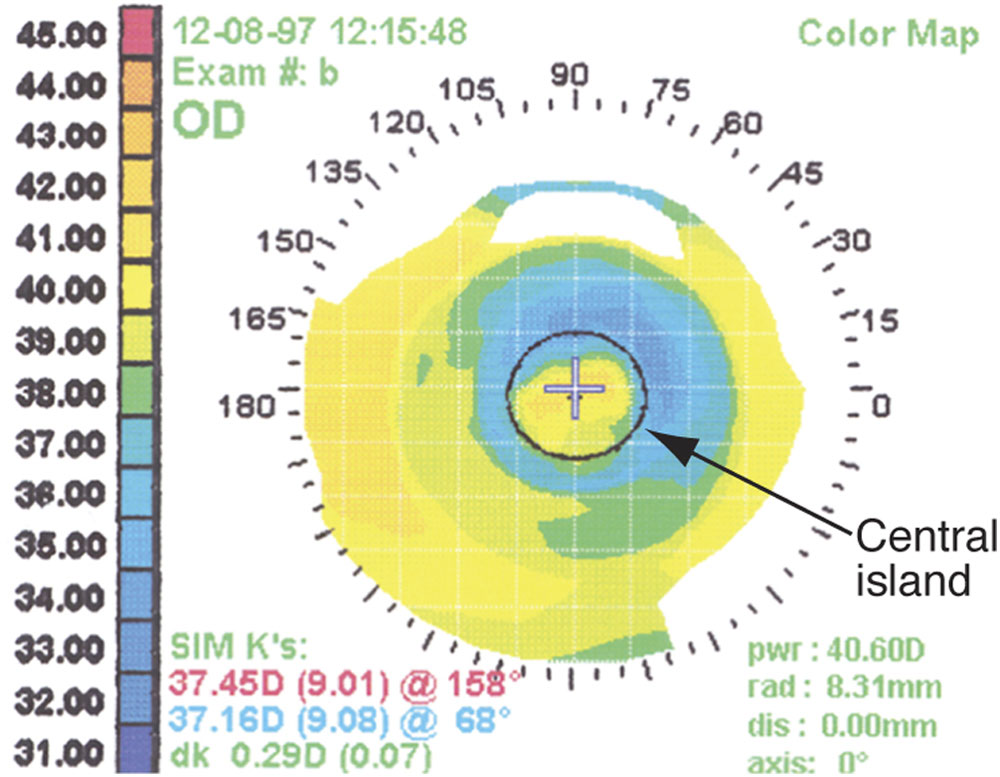
Figure 6-2 Corneal topography findings of a myopic ablation (blue) with a central island (yellow) in the visual axis. (Courtesy of Roger F. Steinert, MD.)
The occurrence of central islands has been reduced significantly through the use of scanning and variable-spot-size lasers and is now rarely encountered with modern laser technology. Fortunately, most central islands diminish over time, especially after surface ablation, although resolution may take 6–12 months. Treatment options such as topography-guided ablations may be helpful in treating persistent central islands.
Decentered Ablations
Accurate centration during the excimer laser procedure is important in optimizing the visual results. Centration is even more crucial for hyperopic than myopic treatments. A decentered ablation may occur if the patient’s eye slowly begins to drift and loses fixation or if the surgeon initially positions the patient’s head improperly; if the patient’s eye is not perpendicular to the laser treatment, parallax can result (Fig 6-3). The incidence of decentration increases with slow eye tracking, hyperopic ablations, and higher refractive correction, due to longer ablation times. Decentration may be reduced by ensuring that the patient’s head remains in the correct plane throughout the treatment—that is, perpendicular to the laser (parallel to the ground)—and that there is no head tilt. Treatment of decentration with topography-guided technology may be effective.
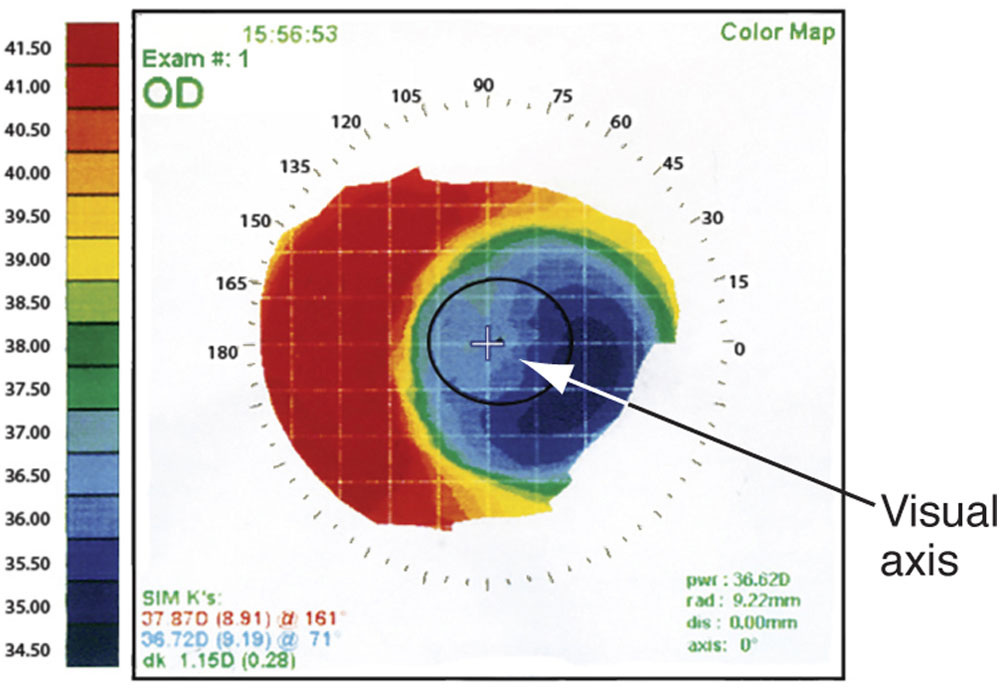
Figure 6-3 Corneal topography findings of a decentered ablation. (Courtesy of Roger F. Steinert, MD.)
Corticosteroid-Induced Complications
The incidence of increased intraocular pressure (IOP) after surface ablation has been reported to range from 11% to 25%. Occasionally, the IOP may be quite high. In 1 study, 2% of patients had IOP greater than 40 mm Hg. The majority of cases of elevated IOP are associated with prolonged topical corticosteroid therapy. Accordingly, postoperative steroid-associated IOP elevations are more likely to occur after surface ablation (after which steroid therapy may be used 2–4 months to prevent postoperative corneal haze) or after complicated LASIK cases. Corticosteroid-induced elevated IOP occurs in 1.5%–3.0% of patients using fluorometholone but in up to 25% of patients using dexamethasone. The increase in IOP is usually controlled with topical IOP-lowering medications and typically normalizes after the corticosteroids are decreased or discontinued. Because of the changes in corneal curvature and/or corneal thickness, Goldmann tonometry readings after myopic surface ablation and LASIK are artifactually reduced (see Glaucoma After Refractive Surgery in Chapter 11). Several alternative techniques of measuring IOP have been suggested, but dynamic contour tonometry is the only technique shown to have sufficient reproducible accuracy in eyes after refractive ablation. Other corticosteroid-associated complications that have been reported after surface ablation are herpes simplex virus keratitis, ptosis, and cataracts.
Central Toxic Keratopathy
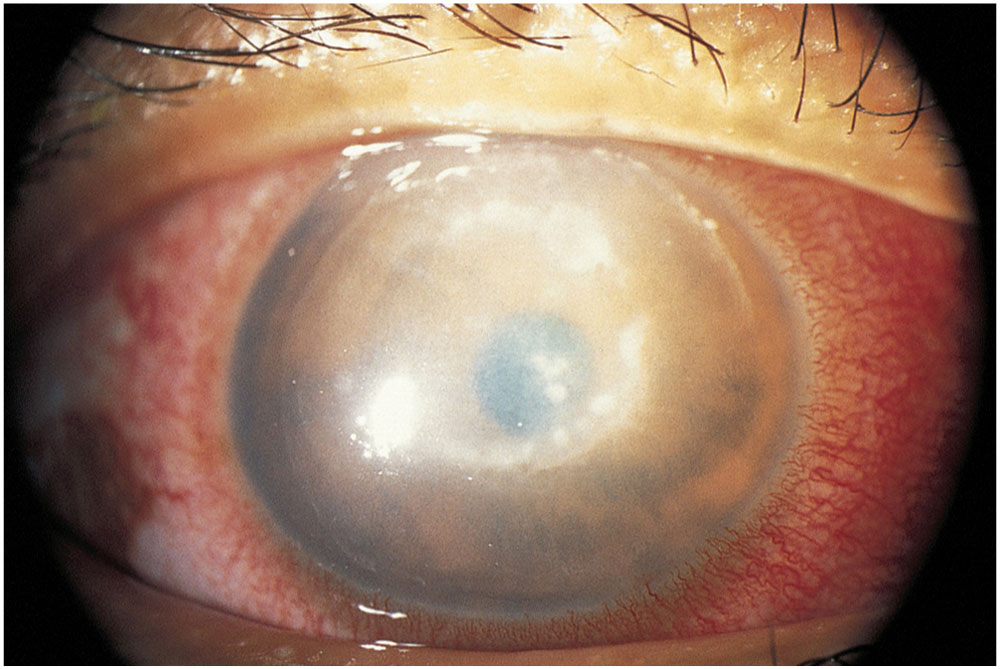
Central toxic keratopathy is a rare, acute, noninflammatory central corneal opacification that can occur within days after uneventful LASIK or PRK (Fig 6-4). The etiology is unknown but may be related to enzymatic degradation of keratocytes.
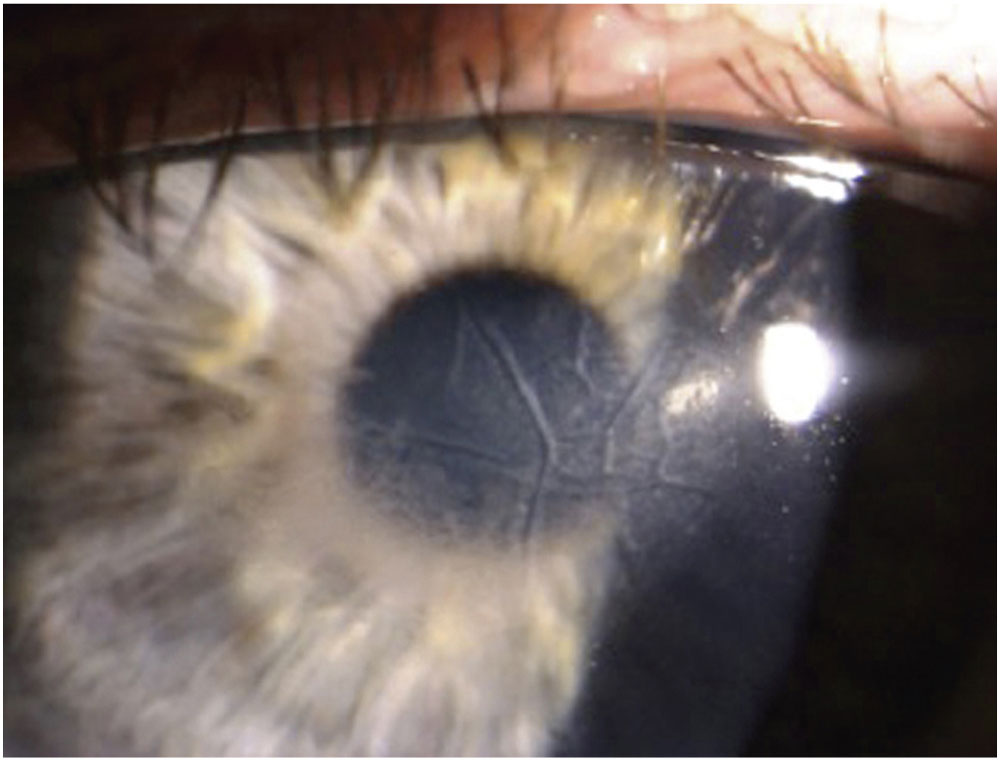
Figure 6-4 Clinical photograph of central toxic keratopathy, a rare, acute, noninflammatory central corneal opacification that can occur within days after uneventful LASIK or photorefractive keratectomy (PRK). (Courtesy of Parag Majmudar, MD.)
Confocal microscopy has demonstrated activated keratocytes without inflammatory cells, with initial keratocyte loss from the stromal bed and gradual repopulation over time. Central toxic keratopathy has been reported to demonstrate anterior curvature flattening without alteration of posterior curvature in anterior segment tomography; however, some cases do appear to alter all tomographic findings, likely as measurement artifact. The onset is acute without worsening over time, unlike in most other interface entities.
Moshirfar M, Hazin R, Khalifa YM. Central toxic keratopathy. Curr Opin Ophthalmol. 2010; 21(4):274–279.
Thornton IL, Foulks GN, Eiferman RA. Confocal microscopy of central toxic keratopathy. Cornea. 2012;31(8):934–936.
Infectious Keratitis
Infectious keratitis may occur after surface ablation procedures or LASIK, as both types of surgery involve disturbance of the ocular surface, although infections are significantly more common after surface ablation. The risk of infection varies depending on the specific technique. The most common etiologic agents for these infections are gram-positive organisms, including Staphylococcus aureus, methicillin-resistant Staphylococcus aureus (MRSA), Streptococcus pneumoniae, and Streptococcus viridans. Although health care workers and others exposed in hospital and nursing home settings may be at greatest risk for MRSA infection, MRSA infections have been diagnosed in increasing numbers of cases without known risk factors. Atypical mycobacteria, Nocardia asteroides, and fungi have also been reported to cause infectious keratitis after surface ablation and LASIK (Fig 6-5).
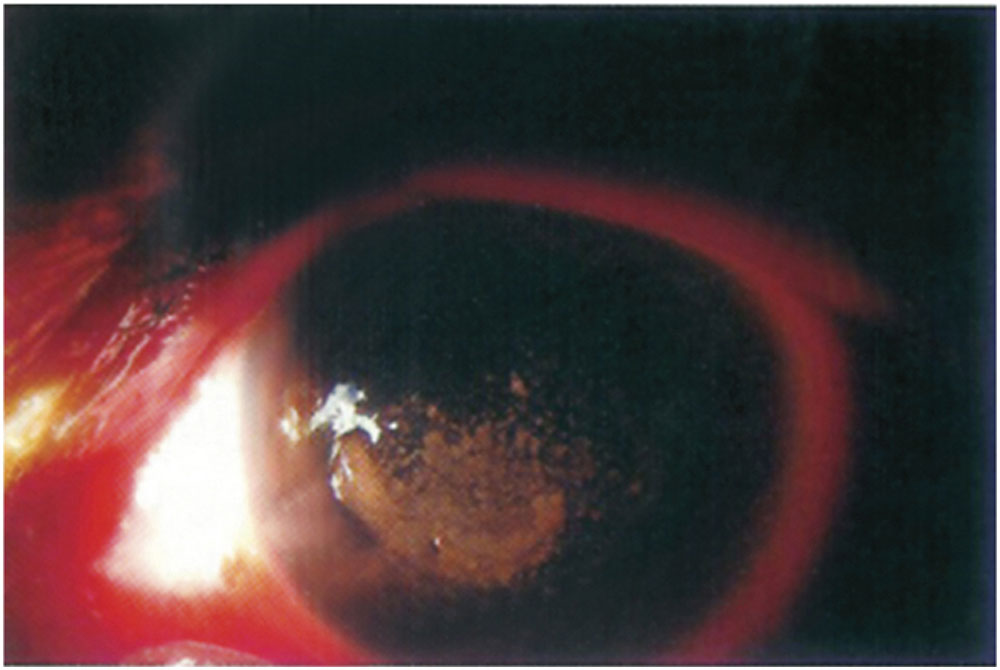
Figure 6-5 Slit-beam image of Mycobacterium chelonae interface infection presenting 3 weeks after LASIK; this infection was initially treated as diffuse lamellar keratitis with topical corticosteroids. (Courtesy of Christopher J. Rapuano, MD.)
PRK and other surface ablation techniques involve creation of an iatrogenic corneal epithelial defect that may take 3–5 days to heal. During this time, the risk of postoperative infectious keratitis is greatest because of exposure of the stroma, use of a bandage contact lens, and administration of topical steroid drops, all of which increase the opportunity for eyelid and conjunctival bacterial flora to gain access to the stroma. Treatment of postoperative infectious keratitis consists of culture and sensitivity testing of contact lens and corneal scrapings and institution of appropriate intensive, topical, broad-spectrum antibiotic coverage, being cognizant of the higher prevalence of keratitis secondary to gram-positive organisms. Antibiotics may include a combination of the following: fourth-generation fluoroquinolones, polymyxin B–trimethoprim, fortified vancomycin or cefazolin, and for tified tobramycin or gentamicin. Fungal keratitis can also occur, especially with concomitant corticosteroid use. With that in mind, cultures should include fungal assays, and treatment for keratitis should include antifungals in suspected cases.
During or shortly after LASIK, which involves creation of a corneal flap, eyelid and conjunctival flora may enter and remain sequestered under the flap. The antimicrobial components in the tears and in topically applied antibiotic drops have difficulty penetrating into the deep stroma to reach the organisms (Fig 6-6). If a post-LASIK infection is suspected, the flap should be lifted and the stromal bed scraped for culture and sensitivity testing. Intensive treatment with topical antibiotic drops, as described previously, should be started pending culture results. If there is lack of clinical progress, additional scrapings may be obtained, the flap may be amputated, and the antibiotic regimen altered.
Llovet F, de Rojas V, Interlandi E, et al. Infectious keratitis in 204,586 LASIK procedures. Ophthalmology. 2010;117(3):232–238. Epub 2009 Dec 14.
Moshirfar M, Welling JD, Feiz V, Holz H, Clinch TE. Infectious and noninfectious keratitis after laser in situ keratomileusis: occurrence, management, and visual outcomes. J Cataract Refract Surg. 2007;33(3):474–483.
Mozayan A, Madu A, Channa P. Laser in-situ keratomileusis infection: review and update of current practices. Curr Opin Ophthalmol. 2011;22(4):233–237.
Solomon R, Donnenfeld ED, Perry HD, et al. Methicillin-resistant Staphylococcus aureus infectious keratitis following refractive surgery. Am J Ophthalmol. 2007;143(4):629–634. Epub 2007 Feb 23.
Wroblewski KJ, Pasternak JF, Bower KS, et al. Infectious keratitis after photorefractive keratectomy in the United States Army and Navy. Ophthalmology. 2006;113(4):520–525. Epub 2006 Feb 17.
Complications Unique to Surface Ablation
Persistent Epithelial Defects
Usually, the epithelial defect created during surface ablation heals within 3–5 days with the aid of a bandage soft contact lens. A frequent cause of delayed re-epithelialization is keratoconjunctivitis sicca, which may be treated with increased lubrication, cyclosporine, and/or temporary punctal occlusion. Patients who have undiagnosed autoimmune connective tissue disease or diabetes mellitus or who smoke may also have poor epithelial healing. Topical nonsteroidal anti-inflammatory drugs (NSAIDs) should be discontinued in patients with delayed re-epithelialization. Gentle epithelial debridement and oral tetracyclines may be beneficial for persistent epithelial defects. Temporary discontinuation of other potentially toxic topical drugs, such as glaucoma drops, may also help in re-epithelialization. The importance of closely monitoring patients until re-epithelialization occurs cannot be overemphasized, as a persistent epithelial defect increases the risk of corneal haze, irregular astigmatism, refractive instability, delayed visual recovery, and infectious keratitis.
Sterile Infiltrates
The use of bandage contact lenses to aid epithelial healing is associated with sterile infiltrates, which may occur more frequently in patients using topical NSAIDs for longer than 24 hours without concomitant topical corticosteroids. The infiltrates, which have been reported in approximately 1 in 300 cases, are secondary to an immune reaction (Fig 6-7). They are treated with institution of topical steroids, tapering and discontinuation of topical NSAIDs, and close follow-up. It must be kept in mind that any infiltrate may be infectious and should be managed appropriately. If infectious keratitis is suspected, the cornea should be scraped and cultured for suspected organisms.
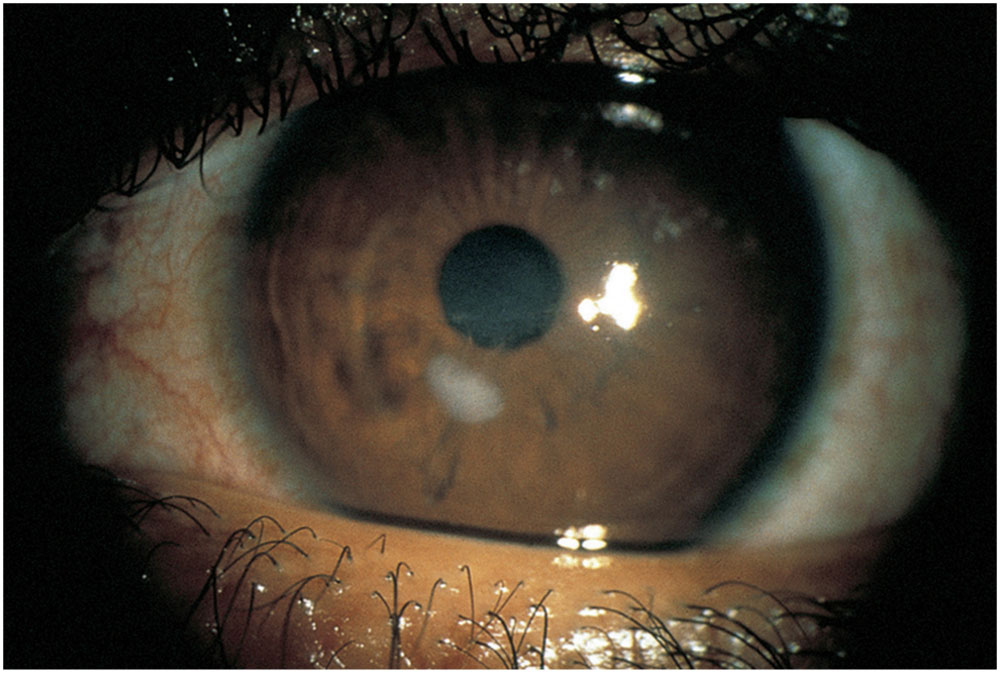
Figure 6-7 Stromal infiltrates after use of a bandage soft contact lens following PRK. (Courtesy of Jayne S. Weiss, MD.)
Corneal Haze
The manner of wound healing after surface ablation is important in determining postoperative topical corticosteroid management. Eyes that have haze and are undercorrected may benefit from increased corticosteroid use. Eyes with clear corneas following surface ablation and that are overcorrected may benefit from a reduction in topical corticosteroids, which may lead to regression of the overcorrection.
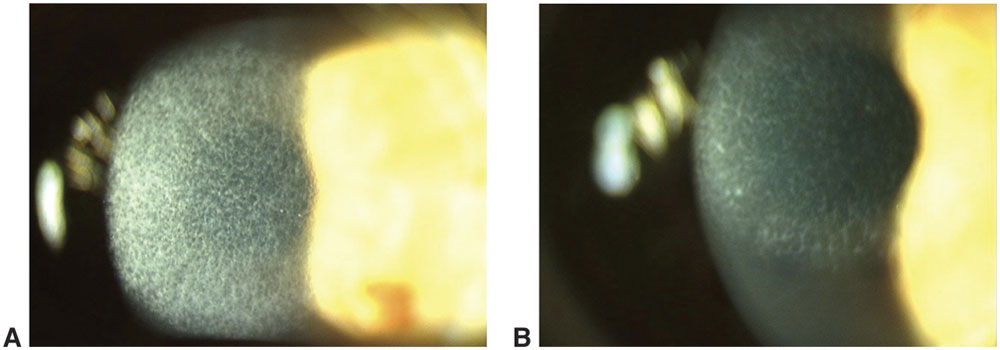
When present, subepithelial corneal haze typically appears several weeks after surface ablation, peaks in intensity at 1–2 months, and gradually diminishes or disappears over the following 6–12 months (Fig 6-8). Late-onset corneal haze may occur several months or even a year or more postoperatively after a period in which the patient had a relatively clear cornea. Histologic studies in animals with corneal haze after PRK demonstrate abnormal glycosaminoglycans and/or nonlamellar collagen deposited in the anterior stroma as a consequence of epithelial–stromal wound healing. Most histologic studies from animals and humans show an increase in the number and activity of stromal keratocytes, which suggests that increased keratocyte activity may be the source of the extracellular deposits.
Persistent severe haze is usually associated with greater amounts of correction or smaller ablation zones. Animal studies have demonstrated that ultraviolet (UV) B exposure after PRK prolongs the stromal healing process, with an increase in subepithelial haze. Clinical cases of haze after high UV exposure (such as at high altitude) corroborate these studies.
If clinically unacceptable haze persists, a superficial keratectomy or phototherapeutic keratectomy (PTK) may be performed. In addition, topical mitomycin C (0.02%), with PTK or debridement, may be used to prevent recurrence of subepithelial fibrosis. Because haze is known to resolve spontaneously with normal wound remodeling, re-ablation should be delayed for at least 6–12 months. The clinician should be aware that, in the presence of haze, refraction is often inaccurate, typically with an overestimation of the amount of myopia.
Ayres BD, Hammersmith KM, Laibson PR, Rapuano CJ. Phototherapeutic keratectomy with intraoperative mitocmycin C to prevent recurrent anterior corneal pathology. Am J Ophthalmol. 2006;142:490–492.
Donnenfeld ED, O’Brien TP, Solomon R, Perry HD, Speaker MG, Wittpenn J. Infectious keratitis after photorefractive keratectomy. Ophthalmology. 2003;110(4):743–747.
Hofmeister EM, Bishop FM, Kaupp SE, Schallborn SC. Randomized dose-response analysis of mitomycin-C to prevent haze after photorefractive keratectomy for high myopia [published online ahead of print July 3, 2013]. J Cataract Refract Surg. doi:10.1016/j.jcrs.2013.03.029.
Krueger RR, Saedy NF, McDonnell PJ. Clinical analysis of steep central islands after excimer laser photorefractive keratectomy. Arch Ophthalmol. 1996;114(4):377–381.
Moller-Pedersen T, Cavanagh HD, Petroll WM, Jester JV. Stromal wound healing explains refractive instability and haze development after photorefractive keratectomy: a 1-year confocal microscopic study. Ophthalmology. 2000;107(7):1235–1245.
The complications associated with LASIK are primarily related to flap creation, postoperative flap positioning, or interface problems.
Microkeratome Complications
In the past, the more severe complications associated with LASIK were related to problems with the microkeratome, which caused the planned LASIK procedure to be abandoned in 0.6%–1.6% of cases. In current practice, advances in microkeratome technology and the advent of femtosecond laser use for creating the LASIK flap have substantially reduced the incidence of severe, sight-threatening complications.
When using the microkeratome, meticulous care must still be taken in the cleaning and assembly of the microkeratome to ensure a smooth, uninterrupted keratectomy. Defects in the blade, poor suction, or uneven progression of the microkeratome across the cornea can produce an irregular, thin, or buttonhole flap (Fig 6-9), which can result in irregular astigmatism with loss of CDVA. Steep corneal curvature is a risk factor for the development of some intraoperative flap complications. If a thin or buttonhole flap is created, or if an incomplete flap does not provide a sufficiently large corneal stromal surface to perform the laser ablation, the flap should be replaced and the ablation should not be performed. Substantial loss of vision can be prevented if, under such circumstances, the ablation is not performed and the flap is allowed to heal before another refractive procedure is attempted months later. In such cases, a bandage soft contact lens is applied to stabilize the flap, typically for several days to a week. Although a new flap can usually be cut safely using a deeper cut after at least 3 months of healing, most surgeons prefer to use a surface ablation technique.