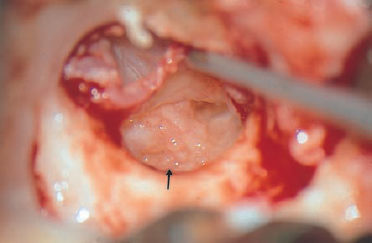
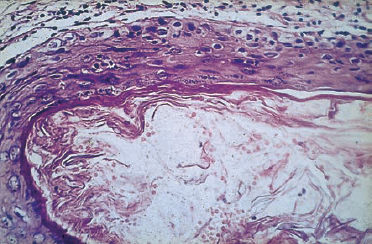
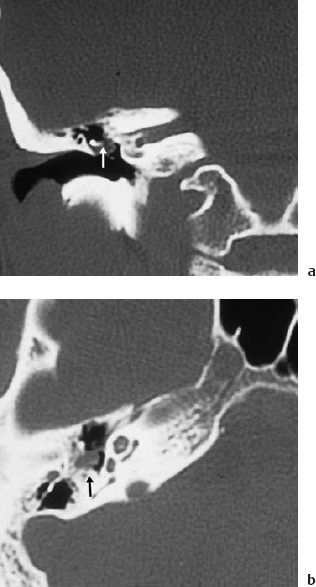
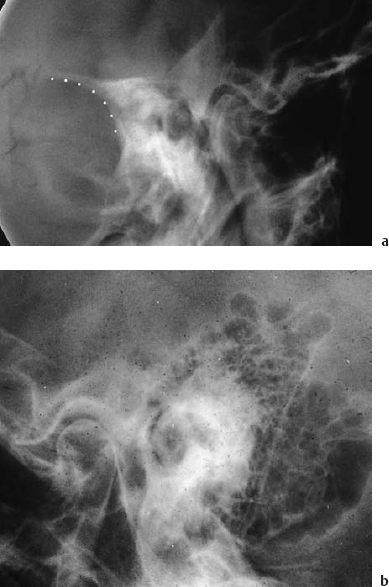
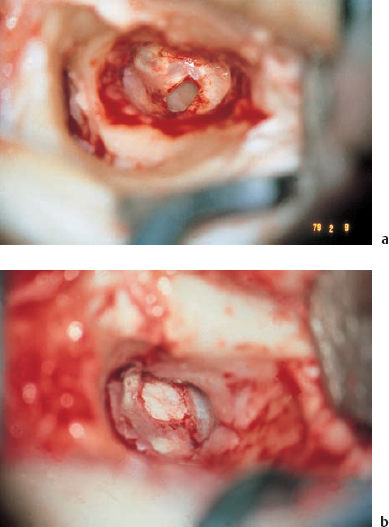
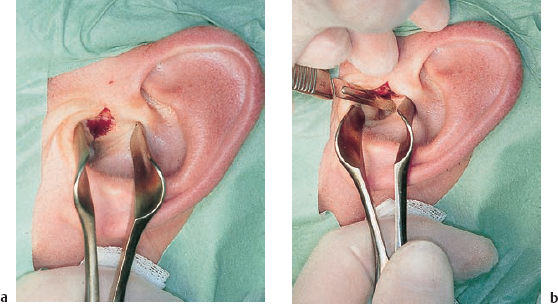
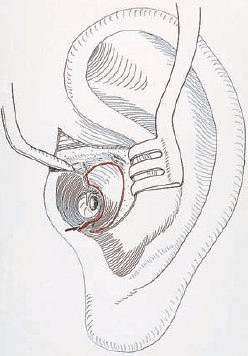
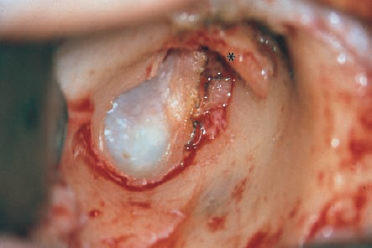
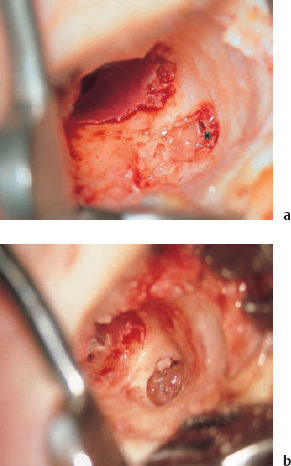
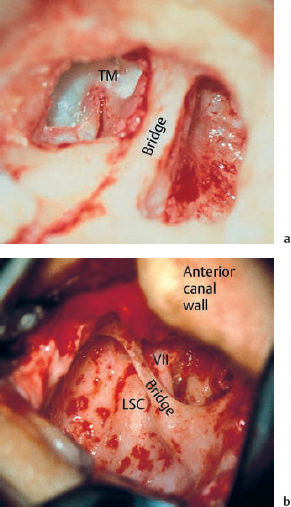
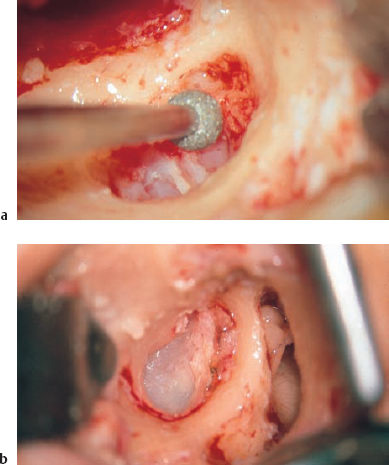
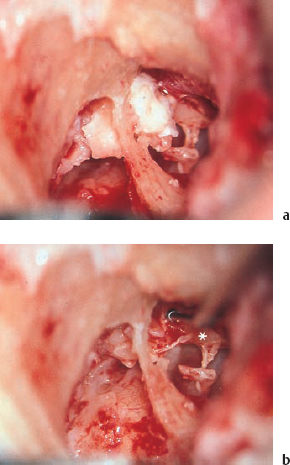
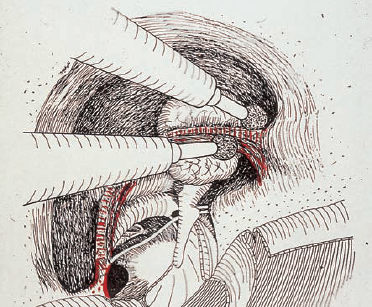
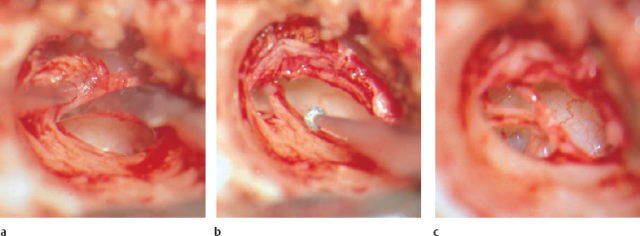
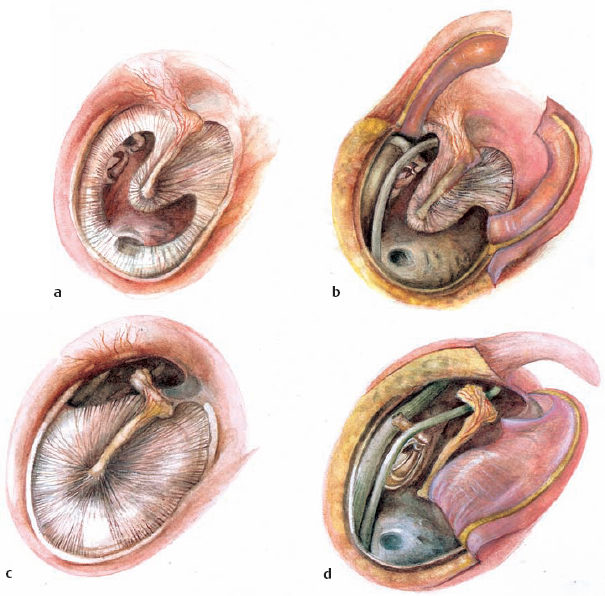
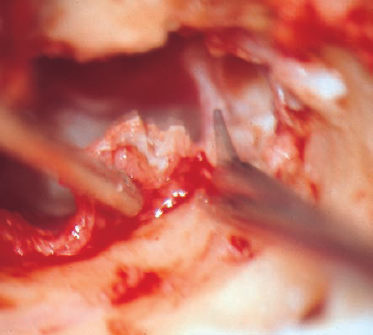
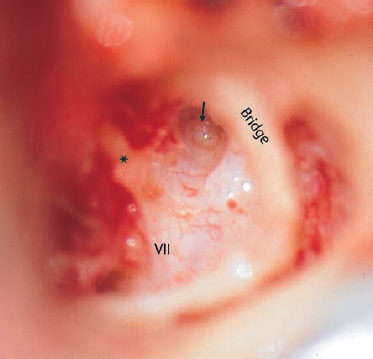
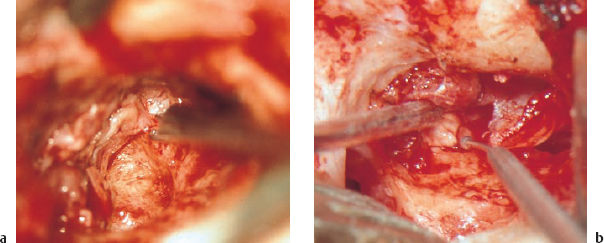
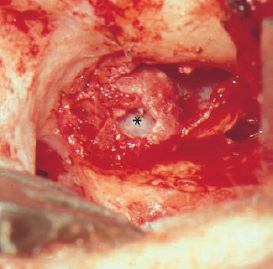
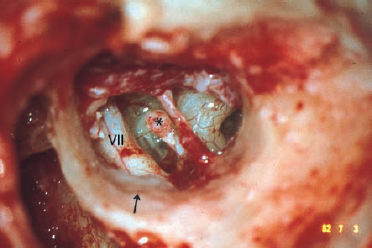
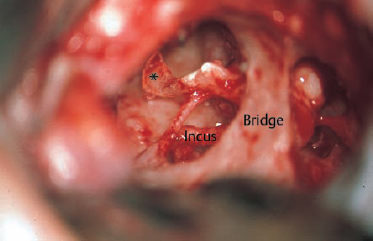
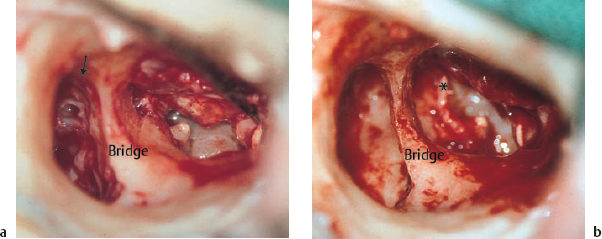
10 Chronic Otitis Media and Complications of Otitis Media The largest and most widely varied field within otology is the treatment of chronic otitis media—ranging from limited foci in the tympanic cavity to extensive involvement of the temporal bone. The criteria for chronic otitis media are: Complications include all forms of proliferation of the mucositis into neighboring structures such as bone (osteitis), endocranium (meningitis, cerebral abscess), nerves (neuritis), larger vessels (thrombophlebitis of the sinuses), and the inner ear (labyrinthitis). Tos et al. (1999) provide a valuable overview of contemporary knowledge and techniques for managing chronic otitis media. Chronic otitis media is most often accompanied by secretion into the external ear canal, but “dry ears” are also common. The latter are not free of the risk of reactivated infection, with complications developing. The traditional distinctions between different forms of chronic otitis media are of limited value, as they frequently overlap with mixed forms. However, classifying the condition prior to surgery may be helpful for reaching a treatment decision, deciding on a recommendation for staged interventions, and informing the patient. With these reservations in mind, distinctions can be drawn between: Inflammatory changes in the mucoperiosteum (chronic mucositis) are basically reversible after the pathogenetic factors have been eliminated in both the simplex form and the granulating form even in osteitis. However, deposits of chalk (tympanosclerosis) or keratinizing epithelium (cholesteatoma) have to be removed mechanically before healing is possible. Adhesive processes, in which the respiratory mucosa of the middle ear is replaced by fibrous scar tissue, are particularly problematic. This type of process can start in one area and may remain local, limited to the formation of some fibrous adhesions, but it may also proliferate across large surfaces, ending up with complete atresia of the middle ear spaces. One should be aware that any contact between two mucosal surfaces (atelectasis) can quickly result in a loss of lining epithelium and production of fibrosing granulations (Fig. 10.1). But the two mucosal layers can also persist for many years, and may remain separable surgically. Chronic otitis media basically starts during childhood, but it is often first detected in adults. Unilateral involvement is seen in about 50% of cases, with no prevalence between the two sides. The pathogenesis is not totally clear. There is consensus regarding the causative role of a malfunctioning eustachian tube during early childhood, due to disturbed nasal respiration or propagation of sinusitis (Bluestone 1995). In 100 cases of unilateral chronic otitis media, 19 ipsilateral, seven contralateral, and 17 bilateral foci of sinusitis were found (Wigand 1965). In adulthood, chronic otitis media can also be triggered by such events, as well as by nasopharyngeal malignancy. Any otosurgeon who is planning functional reconstruction needs to be aware of these associated conditions. Differentiating between central and marginal perforations is of little value here. More important is the difference between real perforations—with the mucosa visible on the promontory (Fig. 10.2)—and pseudoperforations, which are herniations of the drum membrane into the tympanic cavity or attic (with squamous epithelium on the promontory). Genuine marginal perforations, with the fibrous annulus absent, do notinfact exist. Microsurgery has shown that a thin fibrous rim can always be found below apparently marginal perforations with adjacent cholesteatoma growth. The traditional distinction between central and marginal perforation therefore needs to be replaced by a distinction between perforation and invagination. Limited invagination of the drum membrane, induced by retraction, creates the appearance of an epithelialized defect (Fig. 10.3), with further progress of the invagination into an epidermized tympanic cavity. True perforations only exceptionally lead to cholesteatoma. This can happen in traumatic perforations, or after rupture of a retraction pocket. The pathogenesis of cholesteatoma has fascinated otologists for many decades. In addition to the mechanism of cholesteatoma growth from dispersed islands of ectodermal skin matrix, without connection to the drum membrane or to the external auditory meatus (congenital genuine cholesteatoma), two other etiological mechanisms have been generally accepted: acquired primary cholesteatoma, caused by the invasion of epithelium from Shrapnell’s membrane; and acquired primary or mesotympanic cholesteatoma, which is thought to originate from epidermal growth through perforations in the drum membrane. Important reviews of the various classical explanations were presented by Rüedi (1978) and Escher (1979). They underlined the causative role of the underlying inflammatory tissue (“perimatrix”) in inducing epidermal invasion of the bone, and logically proposed that this should be treated with surgical removal of the underlying soft tissue (“perimatrix”), together with the epithelium. However, microscopic examination of epitympanic and mesotympanic cholesteatomas (Fig. 10.4) does not confirm these hypotheses. Secondary epithelialization through tympanic defects is practically never encountered, but one can almost always identify configurations involving retraction of a continuous epidermal surface. This may perforate secondarily, but true perforation of a cholesteatoma retraction sac is rarely seen in this way. Retraction can be induced by hypotension in the middle ear, with tubal insufficiency (more precisely termed “impression pocket”), or by shrinking and scarification of the inflamed underlying mucosa (“retraction pocket”). From a certain point onward, the retention of squamous debris exerts destructive pressure on the underlying bone. Cholesteatomas in infants consequently grow faster, as the bone is less resistant. Implantation of epidermis can, of course, be caused by middle ear trauma. Fig. 10.1 Initial stage of chronic otitis media. The first granulations have developed on the promontory (arrow), within a slightly swollen mucosa, coming into contact with the drum membrane (right ear). Fig. 10.2 Central perforation. The mucosa is visible on the promontory (*). Fig. 10.3 Pseudoperforation of the tympanic membrane. A retraction pocket has formed due to an adhesive process in the tympanic cavity. The head of the stapes (*) is prominent, in the absence of the long process of the incus. Fig. 10.4 Histological appearance of a cholesteatoma matrix. The surface is covered with keratinizing masses, pressure from which has flattened the squamous epithelium. The basal cells are also distorted, but they are well demarcated against the underlying connective-tissue perimatrix, which has replaced the respiratory epithelium (hematoxylin-eosin, original magnification 250 ×). A metaplastic cause for tympanic cholesteatomas (Sadé et al. 1983) is a hypothetical consideration for which there is little evidence in middle ear surgery. Support for our denial of the existence of “secondary” mesotympanic cholesteatomas is provided by interesting photographic follow-up studies of epidermal migration processes around tympanic membrane perforations, in which ingrowth of epithelium was never observed (Litton 1963, Franz 1966). The presenting symptoms of chronic otitis media are: These are frequent, but not obligatory. They may occur temporarily, with acute phases of rhinosinusitis, and they may also be absent over long periods of time. Other symptoms suggest incipient or advanced complications: Ear microscopy or endoscopy will show a pathological appearance in the drum membrane, with thickening, calcification, or perforation. If squamous epithelium can be recognized behind the defect, it is usually a pseudoperforation—i.e., invasion of the epithelium by retraction into the tympanic cavity or into the attic. A deep pouch may lead into the epitympanum, signalizing a cholesteatoma. The full extension of this cannot be assessed by direct inspection, unless there is destruction of the bony meatal wall. Short endoscopes with an angled view have proved valuable for exploring these pockets and recesses. Secretion from the middle ear indicates an exudative phase of the mucosal inflammation, but can also be caused by a simple granulation polyp. Although the consistency of the secretion is not informative, taking a swab for microbiological investigation provides a basis for targeted antibiotic treatment. Administration of systemic antibiotics perioperatively can improve the chances of successful tympanoplasty. Discharge from the ear—particularly if it is intermittent—must raise a suspicion of nasal pathology, and sinusitis in particular. Radiological examination of the sinuses is then mandatory. A check-up on nasal respiration is also recommended, but tubal function tests are no longer important, as they are not predictive of the outcome of surgery. Pure tone audiometry provides objective evidence of mechanical disturbance (based on the air–bone gap) and of sensorineural deficits (based on abnormal bone conduction). A perforation causes air–bone gaps of up to 25 dB; larger conduction losses indicate interruption or fixation of the ossicular chain. This diagnosis can be supported by measuring the middle ear reflexes, which are absent with stapes fixation. Tympanometry allows conclusions to be drawn regarding the middle ear pressure, and indirectly regarding tubal function. However, more or less normal hearing may persist even with large attic cholesteatomas if there is good sound transmission through the lesion to the stapes footplate. Speech audiometry is valuable for evaluating the overall outcome of surgery, but does not provide any informations regarding the diagnosis. Precise vestibular testing is necessary in all patients with vestibular symptoms and with positive-pressure nystagmus (a symptom of fistula). An electrophysiological examination (preferably electromyography; electroneuronography is less precise) of the facial nerve can be recommended whenever there are complications, and in cases in which revision is required. It is also prudent to test lacrimal and gustatory function before temporal bone surgery. Taking a general neurological status is imperative in every patient in whom there is a suspicion of sinus thrombosis or endocranial complications. For imaging of the temporal bone, high-resolution computed tomography (CT) on the axial and coronal planes is preferable today for detecting the extent of cholesteatoma (Fig. 10.5), labyrinthine fistulas, or ventilation passages, particularly when investigating complications. The classic Schüller projection (Fig. 10.6) is valuable for evaluating the current type and status of the pneumatization. It is therefore helpful for choosing the approach in cholesteatoma surgery; many authors prefer to use the combined approach, with preservation of the posterior bony canal wall, only in well-pneumatized mastoids. The classic Stenvers projection and its variants (providing information on the inner ear and internal auditory canal) are no longer indicated, since the related questions are now much better answered using high-resolution CT scanning. Fig. 10.6 Schüller-projection radiograph of a right mastoid with chronic otitis media. a The reduced pneumatization and translucency of the semicircular canals indicates a cholesteatoma. There is sharp delineation of the sigmoid sinus (…). b The contralateral ear has a normal appearance. The differential diagnosis of chronic otitis media is not extensive. The presenting symptoms of specific conditions (tuberculosis, acquired immune deficiency syndrome, Wegener’s granulomatosis, etc.) are only occasionally observed in the middle ear. Resistance to therapy or an abnormal course will raise suspicions and lead to a serological examination (antineutrophil cytoplasm antibody, ANCA) and a histological examination. The same applies to tumor-like lesions and neoplasia. Carcinoma of the external ear canal or middle ear may occasionally imitate chronic otitis media. The curative treatment for chronic otitis media is surgery, not conservative antimicrobial therapy. A functional reconstructive operation is therefore always indicated as a matter of principle. Irrespective of the patient’s age, there are absolute indications for surgery in all cases of progressive inflammation, threatening complications, and cholesteatoma. Concomitant rhinological treatment—e.g., adenoidectomy in early childhood, or sinus surgery in adults—can often convert the active phase of chronic otitis media into a mild, nonprogressive form, reducing the absolute indication to a relative one and meaning that surgery can be canceled or postponed in patients who are in poor health, or in infants below three years of age. In our department, we have individual restrictions on ear surgery in relation to older and younger patients, but no general restrictions based on principle. Relative indications also include dry, symptomfree ears without cholesteatoma. In these cases, advice in favor of carrying out functional microsurgery is based on the chances for hearing improvement and relief of tinnitus, reestablishment of watertight closure, and on the potential reduction in the relevant risk of complications. There is a consensus in the literature that ear surgery produces superior results in the treatment of chronic otitis in dry ears. Reconstruction of middle ears with discharge is associated with higher failure rates, in relation to both definitive healing and hearing function. However, I do not hesitate to operate on a draining ear, since recovery without surgery is often impossible. Concomitant rhinological surgery, if indicated, will also reduce harmful influences. However, the patient should be informed about the possible limitations of reconstructive elements—e.g., the problems of installing a columella into an oval niche with swollen mucosa or an adhesive process. The possibility of carrying out a second operation after improvement in the condition should be discussed. Planning a second intervention has proved successful when there is: It should be emphasized that in our department, defects in the tympanic membrane caused by chronic otitis media are not simply closed using a myringoplasty carried out through a speculum. Experience has shown us that hidden pathology in the attic or mastoid is not infrequent with dry central perforations—for instance, there is often an occult fibrous aditus blockade. Myringoplasty is therefore combined with antrum control, requiring the standard endaural approach. Tympanoplastic operations through a speculum are reserved for other indications—e.g., failed myringoplasty, trauma, or exploration of the tympanic cavity. The simple procedure involved in plastic microsurgical closure of a perforated tympanic membrane is the most widely used element in reconstructive ear surgery, and one that has had a significant impact on public awareness of the fact that a perforated drum is the main feature of otitic deafness. It should not be forgotten that Wullstein’s, Zöllner’s and Plester’s initial reports on the use of free skin onlay grafts for this purpose gave rise to protests from plastic surgeons—the implantation of living tissue on a narrow recipient bed over an infected cavity was regarded as hazardous and counterproductive. However, it soon became evident that tissues such as skin, fascia, periosteum, perichondrium, and even homologous membranes such as prefabricated dura, fascia, or even allogenic vessels are incorporated and revitalized from the periphery through the ingrowth of marginal vessels, or can serve as splints for replacement with new autogenous fibrous tissue. The first important step is therefore to prepare the implantation bed. A circular incision is made around the perforation, to remove any overhanging epithelium that may be present (Fig. 10.7). A sickle knife and a double-cup forceps are useful for this maneuver. The adjacent undersurface of the drum membrane is scratched with a hook over a distance of 1–2 mm in order to stimulate capillary regrowth. It may be difficult to create this circular wound around the perforation if the defect has reached the handle of the malleus. Using a sharp sickle knife or round knife, the residual drum and underlying mucosa have to be scratched from the manubrium as far as necessary to prepare an overhanging flap 1–2 mm wide, below which the graft can be placed over the umbo. Due to concern regarding the possibility that these manipulations may cause inner ear trauma in an intact ossicular chain, many schools recommend leaving the remnants on the manubrium and placing the graft below the umbo. However, in my view there is a potential risk that adhesions might arise due to the short distance involved here, or that there might be direct contact with the promontory, and I prefer to carry out very gentle, sharp skeletonizing of the handle of the malleus to provide an onlay on the umbo with an underlay below the perforation margins. Large or subtotal perforations are closed in the same way. If there is only a small strip of the fibrous annulus left, a circular incision is similarly made to allow safe removal of the marginal epithelium, but the internal surface is now freshened down to the osseous annulus. In this way, the graft is inserted below the scratched bone, in order to stimulate capillary invasion from the annulus. However, this design facilitates adhesive propulsion of the graft into the hypotympanum. Particularly if the fascia has to be anchored over the tubal orifice, it may narrow or even occlude the tube. An incision that is not too deep, and fixation to the annulus with the help of tissue adhesive, are therefore recommended. Repositioning the fibrous annulus and the residual drumhead itself has an additional stabilizing effect. Although I abandoned the insertion of Gelfoam into the tympanic cavity many years ago in order to prevent adhesions, we always use loose packing of Gelfoam on the outer surface over the margins of the graft to promote graft cohesion. Myringoplastic closure of a defect as described above is rarely carried out as a single measure—e.g., in cases of traumatic perforation. It can be performed through a small speculum, or else using an endaural approach with an auxiliary skin incision (see the next section, on endaural tympanomeatoplasty)—which at the same time opens up an access route to the inferior edge of the temporalis muscle, from which a suitable piece of fascia can be harvested. If there is no endaural incision, the fascia can be obtained from a small post-auricular skin incision. In most instances, however, myringoplasty is one of the final steps in any tympanoplastic procedure. In my opinion, the indication for a simple myringoplasty is confined to traumatic perforation and to secondary closure when tympanoplasty has failed. Even in dry central perforations with excellent sound conduction, if they are caused by chronic otitis media, I prefer to use a systematic endaural approach—with a brief look into the aditus via the antrum control hole in order to exclude blockage of the aditus by adhesion or granulation, which is often the cause of recurrent mucositis. Fig. 10.7 Closure of a small central perforation with an underlay graft of free temporalis fascia. a A circular incision has been made around the tympanic membrane defect to revitalize its margins. b The graft has been placed under the perforation, extending 1–2 mm beyond the margins. The standard procedure in our department is endaural tympanomeatoplasty. This operation is indicated for all forms of chronic otitis media, including cholesteatoma surgery. It can be divided into four phases: Since the retroauricular skin and mastoid cortex are not compromised by this access route, ear closure is confined to the external ear canal, and any harvesting of free grafts that may be necessary can be carried out using the endaural exposure. The surgery needed may be either minimal or extensive, depending on the individual abnormalities. Even revision operations in ears with previous radical operations can be managed using the standard endaural approach. One exception to this rule may need to be made: if the auricle was displaced during a previous operation with postauricular access, and there is now stenosis of the external canal, deep postauricular retraction, or fistula, the revision should be carried out using a postauricular route in order to renormalize the mentioned alterations. Step 1: skin incisions. A typical Botey endaural auxiliary skin incision (Botey 1898), using a no. 15 scalpel or the electric needle, is brought down to the bone at the meatal entrance (Fig. 10.8). It can start in the tragohelicine incisure at the level of the lower antihelical fold and reach into the roof of the external auditory canal at the squamotympanic fissure. The adjacent skin and periosteum are mobilized using a sharp dissector. A second vertical incision is added at the entrance of the external auditory canal, reaching from the first incision down to the floor of the canal. The posterior circumference of the bony external auditory canal is then uncovered, exposing the suprameatal spine (Henle’s spine). A special retractor designed for endaural surgery is now inserted to retract the auricle posteriorly. A second special retractor is inserted in a perpendicular position, retracting the skin in a craniocaudal direction and pressing the antitragus gently downward. Fig. 10.8 The Botey auxiliary skin incision at the tragohelicine incisure. a The upper extension of the incision varies, depending on how broad the distension needs to be. b An external vertical counterincision from the 6-o’clock to 12-o’clock positions along the bony entrance of the external auditory canal. The above manipulations are carried out under normal vision. At this point, the otomicroscope is positioned for use in the subsequent phases. A third skin incision is now made down into the external auditory canal. It starts at the 12-o’clock position in the first auxiliary incision and runs down to the 6-o’clock position, parallel to the fibrous annulus and at a distance of 2 mm from it, but it is drawn from there over the anterior meatal wall in an oblique direction (Fig. 10.9). This incision requires the use of sharp round knives of adequate sizes and angulations. I prefer an electric needle. All the posterior canal skin can now be mobilized and retracted outward, exposing the posterior bony canal wall from Henle’s spine to the annulus. The caudally based skin flap (in a modification of the Stacke II plasty) can be fixed under the retractor for the period of the subsequent surgery. I prefer to glue it in a suitable position with one drop of fibrin adhesive, which I have ready on the instrument table for every tympanomeatoplasty procedure. Step 2: widening the external auditory canal. The natural shape of the external auditory canal is often inconvenient for direct inspection of the lateral attic wall. An overhanging bony ridge or a hyperplastic squamotympanic suture (Fig. 10.10) may severely impede the exposure of Shrapnell’s membrane initially and of the anterior compartments of the epitympanum later on. Removing this bony crest—which sometimes compromises the accompanying nerve (a branch of the auriculotemporal nerve) and vessels—has therefore become routine. It has also proved valuable to enlarge the diameter of the external auditory canal by milling back its posterior and posteroinferior wall, including the tympanomastoid suture, using a cutting burr (Fig. 10.11). Care is taken to shape the inferior and posterior walls in such a way that flat transitions without overhanging margins are created, resulting in a conical, almost tunnel-like shape of the external auditory canal. This sculpturing, which may open the periantral pneumatization, is particularly important for subsequent clear exposure of the middle ear spaces. The anterior meatal wall, with its marked curvature, may also obstruct visualization of both the anterior quadrants of the drum membrane. It is therefore sometimes necessary to flatten the anterior wall (Fig. 10.12) in order to expose the anterior margin of a perforation or to reach the tubal orifice. For this purpose, one can drill away the overhanging bone, after having pulled outward the anterior canal skin as an externally pedicled flap. The use of a diamond burr is recommended for better protection of the drumhead and of the mandibular joint or parotid gland. Step 3: checking the aditus and antrum. Since it is obligatory, as mentioned before, to check the aditus and antrum in cases of chronic otitis media, enlargement of the external auditory meatus is followed by the establishment of an antrum control hole. The location of this hole, just posterosuperior to the posterior process of the incus (Fig. 10.13), should allow broad inspection of the antrum and of the aditus. Injury to the ossicle, to the lateral semicircular canal and to the tegmen antri can be avoided by using landmarks for guidance. If the periantral pneumatization has already been opened in step 2, it is safe and easy to follow the largest cells into the antrum. The solid bone of the labyrinth would provide a warning if the direction was false. If guidance using cells is not available, orientation may be provided by the inferior border of Shrapnell’s membrane, which is visible in most cases, and this line can be virtually extended backward to a point lying 4–6 mm behind the osseous annulus. Very careful drilling, using a diamond drill if there is any uncertainty, will prevent collision with the incus and ensure that the labyrinth remains untouched. Fig. 10.10 An overhanging bony crest (*) of the squamotympanic suture conceals the lateral attic wall. Fig. 10.11 There is free visualization of the lateral attic wall after the overhanging bony crest of the squamotympanic suture has been drilled away and the vertical diameter of the external auditory canal has been enlarged by milling the roof of the canal. The posterior canal wall is also excavated. Fig. 10.12 The overhanging anterior bony canal wall conceals the anterior tympanomeatal angle. a The anterior margin of a perforation (*) is not visible (right ear). b After correction of the anterior wall, the perforation and anterior tympanic angle are visualized. Fig. 10.13 Checking the aditus ad antrum. a The periantral pneumatization (*) is just opened by widening the external auditory canal. b The hole for checking the antrum in the upper half of the posterior canal wall. The antral mucosa is exposed. Step 4: mastoid control, endaural mastoidectomy. Depending on the actual pathology found in the antrum and on the preoperative imaging findings, the initial interest may be in exposing the tympanic cavity first and checking the mastoid later on. However, I have found it more rational and time-saving to deal with the mastoid first, immediately after exploring it, and to clean the tympanum after that. If a polypoid process or cholesteatoma has been identified during checking of the antrum, the small hole is enlarged in all four directions, depending on individual requirements (Fig. 10.14a). The pathological abnormality has to be visualized completely, although its mastoidal extension may be extremely large—even as far as the mastoid tip and the deep infralabyrinthine or retrosigmoid cells (Fig. 10.14b). However, bone removal is even then confined to what is necessary to obtain good exposure of all pathological abnormalities. One has to learn how to work in a conical surgical field in which the entrance is narrow but the internal space widens. Flexible, frequent rotation of the patient’s head is a prerequisite for this technique. It allows cholesteatoma matrix, cysts, and granulations to be gently lifted under direct visualization from the underlying mucosa, which is preserved. A ball-tipped dissector is ideal for this maneuver. The cells and their lining epithelium are not drilled away. For definitive recovery, it is sufficient to open the cells and niches sufficiently to ensure reventilation and drainage into the central mastoid pathways. Step 5: posterior atticotomy. One of the most important and critical stages in endaural tympanoplasty is the checking of the epitympanic recess via a posterior atticotomy. The attic, and particularly the anterior part of it, is the compartment of the middle ear that is most difficult to reach. Not surprisingly, therefore, the majority of authors prefer broad resection of the lateral attic wall whenever pathological abnormalities such as cholesteatoma have to be removed from this area. This attitude has been a traditional one ever since Zaufal (1890) and Stacke (1893), and since Wullstein (1956b) recommended this type of ablation in his classic type III and type IV tympanoplasties. This technique is among the crucial elements in endaural tympanomeatoplasty with preservation of the “bony bridge,” as it allows management of the epitympanum without removing the bony shield (scutum) of the lateral attic wall in practically all cases, with or without cholesteatoma growth. Starting from the exposure of the aditus via the control hole (see step 3), very careful bone removal is carried out using a diamond burr with a diameter of about 2 mm, in an anterosuperior direction (Fig. 10.15a). This makes it possible in vivo to drill away the bone over the underlying mucosal membrane. The mucosa should not be torn away, but should be transected with sharp scissors. The resulting mucosal flaps can later be replaced onto the bone, which helps avoid granulation. Under microscopic vision, it must be ensured that any injury to an incus that is still in situ, or to the lateral semicircular canal, is avoided. Superiorly, the exposure may extend to the tegmen epitympani, if necessary, to allow a wider survey of the attic. The lateral attic wall (which in fact is a solid three-dimensional block of bone, not literally a wall), is thinned out from inside using smaller diamonds, until the body of the incus and the head of the malleus, with their superior ligaments, are completely visualized (Fig. 10.15b). Depending on the actual pathology, the posterior atticotomy can be extended into the preepitympanic space (Figs. 10.16 and 10.17). If proliferations, membranes, matrix, etc., need to be removed from this space, it may be prudent either to resect the body of the incus or the head of the malleus, or both. If this appears necessary, the posterior atticotomy should be interrupted and continued only after exposure of the mesotympanum and after a possible anterior atticotomy. One should never manipulate the body of the incus and head of the malleus before checking the long process and manubrium. If there is continuity, one must beware of causing mechanical trauma to the inner ear with abrupt manipulations. If epitympanic removal of both of these ossicles is indicated, the long process and the neck of the malleus are gently transected (with a punch or laser) above the oval niche. A little bone removal from the osseous annulus is necessary for this maneuver. The posterior atticotomy can then be continued with retraction of both ossicles using 90° hooks and a double-cup forceps. Fig. 10.15 Posterior atticotomy. a Anterocranial bone resection from the antral hole. b The epitympanic recess is exposed behind the bony bridge. The head of the malleus and body of the incus are visualized (left ear). Fig. 10.16 Anterior atticotomy (right ear). a The lateral bony attic wall has been partly milled in front of the bony bridge in order to allow removal of an attic cholesteatoma under direct microscopy. b Complete dissection of the matrix using the ball-tipped probe. The long process of the incus has been transected. The body of incus had to be removed. (* = malleus handle) Dissection of the epitympanum can now be extended along its tegmen into the most anterior recess. An epitympanic sinus, if present, can be opened by additional bone removal in front of the superior semicircular canal. Often, meticulous removal of the last piece of cholesteatoma matrix is not possible without an additional anterior atticotomy, preserving a thinned bony bridge between the two approaches (Figs. 10.16 and 10.17). Looking alternately through each exposure with a quick change of the visual axis, behind and in front of the bridge, it is always possible to visualize every point in the anterior epitympanum. It should be emphasized again that exposure of the attic spaces is adapted to the individual extent of pathology. If the mucosa is healthy, no matrix present, and free communication between the tympanic cavity and the antrum can be demonstrated by easy suctioning of saline in both directions, then an atticotomy can be reduced to a very small opening, allowing just an inspection. Fig. 10.17 Combination of anterior and posterior atticotomy, with preservation of a thin bony bridge, for removal of an attic cholesteatoma (reproduced with permission from Tos 1995). Step 6: lateral tympanotomy. Inspection and management of the tympanic cavity are carried out by means of lateral tympanotomy—i.e., lifting up the fibrous annulus together with an adjacent ring of canal skin from the osseous annulus, together with the superior and inferior posterior quadrants of the drumhead. This maneuver can also be kept very small if there are no major pathological changes. However, it can be extended to complete excision of the tympanic ring if controlling the pathology requires it. It may be reasonable to make a circular incision round a perforation before lifting the annulus, if necessary. In my own experience, excision of the margins of the perforation to facilitate free grafting is also possible after it has been mobilized. Fig. 10.18 Lateral tympanotomy. a A curved sickle knife lifts the fibrous annulus from the osseous annulus along with a strip of adjacent canal skin. b Posterior resection of the osseous annulus using a diamond burr. c The chorda tympani has been dissected from its channel (right ear). Fig. 10.19 Lateral tympanotomy. After Shrapnell’s membrane has been lifted, exposure of the tympanic cavity can be extended in an anterosuperior direction by lifting the fibrous annulus from the bone, allowing visualization of the protympanum and tubal orifice (arrow). In this case, the residual drumhead remained fixed to the umbo (right ear). *: Antrum. The tympanotomy begins with the circumcision of the canal skin between 12 and 6 o’clock, parallel to and at a distance of 1–2 mm from the fibrous annulus. The skin and annulus are then lifted in continuity (Fig. 10.18). The adjacent tympanic mucosa is incised close to and in parallel with the annulus, opening the hypotympanum and mesotympanum. Particular care is taken to identify and mobilize the chorda tympani, which may be hidden by overhanging bone. Many otosurgeons prefer to use a sharp curette to remove this bone and to expose the chorda and oval niche. I use a small diamond burr (0.2–0.5 mm) for this delicate maneuver, to avoid tearing the small nerve (Fig. 10.18b). The annulus can now be lifted up to Shrapnell’s membrane. In all cases in which manipulations within the mesotympanum become necessary, I extend the superior skin circumcision around Shrapnell’s membrane and lift this girdle of skin together with the membrane from the neck of the malleus beyond the tuberculum anterius process, including the anterosuperior attachment of the fibrous annulus. From here, the annulus can easily be lifted further, and after a parallel incision of the mucosa, the tubal orifice and protympanum can be inspected in front of the malleus (Fig. 10.19). If necessary, the osseous annulus can be fraised back to obtain deeper exposure of the Eustachian tube. The same can be done at its inferior circumference if broad exposure of the hypotympanum is required. Most tympanotomies in this context are carried out in the presence of small or large perforations. Since the remnants of the drumhead are of great value for restitutional closure of the drum at more or less normal size, mobilization of the remnants should be carried out in such a way as to allow them to be used as flaps. Single anterosuperior or anteroinferior defects are rare. They can be handled as described above for myringoplasty, after the tympanic cavity has been inspected via a marginal tympanotomy. More frequent are posterior and posterosuperior defects or pseudoperforations, which are deep mesotympanic or epitympanic retractions. Since I have no concerns regarding any aggressive properties of the invaginated epithelium, this material is also scrutinized for possible use as a final epithelial covering for the fibrous or cartilaginous tympanic graft. An ideal, but rarely used, solution is en-bloc lifting of a tympanomeatal flap with a central perforation in its center. This flap can later be replaced over a fascial or cartilaginous graft that has been introduced. With large perforations, however, it is easier to split the tympanomeatal flap into a superior and inferior flap by transecting it posteriorly at its thinnest portion (Fig. 10.20). Large and deep retraction pockets—either mesotympanic or epitympanic—in fact need to be isolated by a circular incision round their entrances. Theoretically, they represent epidermal hernias, the orifice of which needs to be separated from the tympanic membrane. The remnants of the tympanic membrane can now be handled as superior and inferior flaps, as described above. In the presence of a Shrapnell’s membrane defect, which is an epitympanic hernia, the circular incision needs to follow the inferior margin of the retraction over the posterior malleolar ligament, in parallel with the chorda tympani, up to the anterior tubercle (Fig. 10.21). A superior transection along the superior margin of the retraction pocket follows the edge of the lateral bony attic wall (or what remains of it), also anteriorly to the anterior tubercle. This point—the anterosuperior end of the osseous annulus—will then become the bifurcation of a small superior flap and a larger inferior tympanic one. It is not always easy, irrespective of the approach, to separate these flaps in continuity from the epidermal layer in the attic, to preserve the chorda tympani in front of the malleus, and not to bury some matrix below the flaps. Provided one does not become confused by the three-dimensional confluence of internal surfaces, it is possible to achieve a logical exposure of all the tympanic and epitympanic compartments. Fig. 10.20 Formation of tympanic flaps. a, b Radial posteroanterior transection of the tympanomeatal flap into a central perforation develops two equally large subflaps. c, d Excising an epithelialized attic defect, and lifting the tympanic membrane below the defect and the superior meatal skin above it, produce a larger inferior and a smaller superior skin flap. (green: facial nerve and chorda tympani) Step 7: anterior atticotomy. In cases of anterior attic cholesteatomas or abnormal pneumatization, it may become necessary to visualize more of the protympanum and anterior epitympanum than is possible with the tympanotomy. Additional bone removal from the lateral attic wall in front of the bony bridge is then indicated. As little destructive removal of this important structure, the scutum, should be carried out as possible, and only as much as is necessary to allow free inspection of the proepitympanum, extending as far as and beyond the geniculate ganglion. If there is a deep sinus epitympani, exposure of it may also require removal of the coronoid process with the adjacent bone along the roof of the epitympanum (Fig. 10.22). In such cases, this exposure becomes the most difficult part of the endaural tympanomeatoplasty, and the procedure needs to be studied in intense detail in the laboratory. Removal of the malleus head and neck has to be accepted in such cases (the manubrium being preserved, with its attachment to the tensor tympani tendon), and the chorda tympani also has to be sacrificed. It should be emphasized that I have always found it possible to clean these remote areas—except with large cholesteatomas extending to the petrous apex and internal auditory canal, which require a second approach through the middle cranial fossa. Fig. 10.21 Circular incision of a Shrapnell’s defect using scissors. The inferior transection of the marginal skin follows the posterior malleolar ligament and the chorda tympani by opening a dermal fold (left ear). Fig. 10.22 Exposure of an emptied epitympanum after posterior and anterior atticotomy. Below the bridge lie the fallopian canal, tensor crest (*), and the sinus epitympani (arrow) at the rear. Above the bridge, the tegmen and anterior epitympanic wall are exposed (left ear). Step 8: dissection of the tympanic cavity. In contrast to the exercise on temporal bones without pathology, dissection of a tympanic cavity that has been altered by chronic otitis media presents particular problems. The following tasks are involved: Removal of thick mucus, debris, or cholesterol masses must be complete, but need not injure the mucosa. Gentle suction and soft dissection are usually sufficient. Careful irrigation with saline under moderate pressure is also helpful. Humped areas of edema are left in place; removing them would lacerate the epithelium, inducing granulations and adhesions. I have found that applying topical epinephrine (1 : 1000) is successful—it keeps diffuse hemorrhage under control and considerably reduces edema. It must not be left in place, as it can induce severe ischemia, with subsequent necrosis. However, if one or two drops from a syringe are introduced for a few seconds and then washed out with saline, it is a very helpful tool for testing the reactivity of edematous mucosa. If marked swelling is found, an immediate intraoperative intravenous injection of 250 mg of prednisolone sodium succinate (Solu-Decortin-H) is indicated. Subsequent administration of corticoids for one week appears reasonable. It has been found that corticoids do not compromise the ability of free connective-tissue grafts to take root. With the aim being to preserve as much of the mucous membrane as possible, any crude extraction of adhesions, polyps, or granulations is avoided, and sharp cutting scissors and forceps are used to transect or excise these (Fig. 10.23). This is often necessary in order to liberate the drumhead from the promontory. Mucosal injury here must be minimal. A cholesteatoma matrix is always lifted in continuity, using hooks or (preferably) the ball-tipped dissector. Removal with the double-cup forceps is no longer practiced; this instrument can be used to empty a cholesteatoma sac with intracapsular debulking (Fig. 10.24). This maneuver makes the sac mobile, improving the ability to remove it radically in continuity. Only after the sac has been mobilized and the integrity of its undersurface has been checked one can tear the free edges of it to reduce its size, and this also improves visualization of the next separation border. It is only rarely that it is not possible to dissect a cholesteatoma matrix from the mucosa along a cleavage plane. This may be encountered when there is a very thin matrix in a well-pneumatized mastoid, and it may then be reasonable to drill away some underlying bone. However, carrying out radical avulsion of the matrix together with mucosa and bone as a matter of principle is regarded in our department as being unjustified and detrimental. In particular, prophylactic drilling out of the underlying bone appears to be obsolete. Fig. 10.23 Dissectiolnig of pathological tissues. a Sharp transection of adhesions between the promontory and the drum membrane (left ear). b Blunt lifting of a cholesteatoma matrix using a ball-tipped probe (right ear). Cleaning the oval and round niches of debris, blood clots (blood on respiratory epithelium may induce persistent edema), adhesions, and granulations, is particularly important for restoring sound conduction. Removing blocking adhesions from the niche to the round window is usually unproblematic. These should not be misinterpreted as the round window membrane itself, which is usually hidden by overhanging bone from the promontory. Freeing the stapes superstructure and its footplate from pathological masses, however, is the second critical phase in the whole operation. The amount of mechanical resistance presented by the annular ligament varies from individual to individual, as does the stability of the delicate bone. Extensive personal experience is needed to be able to remove adhesions or fibrous scars gently, without injuring the stapes or the inner ear. I myself do not hesitate to scratch fibrous tissue off the footplate, when the stapes superstructure is absent, but I prefer to leave some residual adhesions if there is an existing stapes blocking free access. It is difficult to judge its mobility with a needle. In the postoperative audiogram, there is often no functional equivalent to what was thought intraoperatively to represent fixation. There is some limited value to the observation of a countermovement of the round window after gentle pressure on the stapes. This can be seen as a slight reflextoasmall drop of saline in the round niche (Wullstein’s counterpressure test). If there is no doubt that there is marked fixation of the footplate, one should not apply force, but should plan a second-stage stapes replacement in a healed, uninfected ear. Cleaning the facial recess, sinus tympani and hypotympanum is usually easy. Exposure of these is achieved by adequate mobilization of the fibrous annulus, possibly extending to the tubal orifice. With the exception of adhesive processes, avulsion of pathological content can be achieved without mucosal injury. Cholesteatomatous pockets can practically always be mobilized in continuity using balltipped hooks, after adequate resection of the overhanging bone. Consistent exposure of the facial recess is mandatory (Fig. 10.25). I have never found it necessary to use the transmastoid extended facial recess approach, which is a last resort. Fig. 10.24 Cholesteatoma sac after intracapsular debulking (*). The matrix can now be handled in continuity (right ear). Fig. 10.25 The oval niche and facial recess (arrow) after partial resection of the osseous annulus (right ear). *: Head of the stapes. Management of the ossicular chain is the key to good functional results in tympanomeatoplasty. A posterior atticotomy and lateral tympanotomy, with additional bone removal from the posterosuperior part of the osseous annulus, allow precise checking. If continuity of the ossicular chain is confirmed, only minor manipulations are necessary—such as transection of adhesions to the promontory or to the facial canal. If the long process of the incus is defective, I prefer to remove the incus and subsequently elevate a mobile stapes using an autograft (see step 9, ossiculoplasty). This technique may also become necessary after optional transection of the long process and removal of the incus in order to empty the attic. Fig. 10.26 The handle and umbo (*) of the malleus have been skeletonized in a patient with a subtotal defect in the tympanic membrane. The ossicular chain is intact (left ear). The malleus is highly resistant to chronic otitis, including cholesteatoma. The manubrium, in particular, persists in most cases. When decapitation of the malleus appears appropriate in order to remove cholesteatoma from the epitympanum, or simply to widen the epitympanic isthmus in cases of stenosing mucositis, the neck of the malleus should be transected superior to its attachment to the tensor muscle tendon. With central perforations, I skeletonize the manubrium in most cases with sharp dissection of the drum membrane, in order to allow onlay of a membranous graft. In this way, the umbo below it can prevent adhesion of the graft to the promontory. When there is an intact pars tensa with an epitympanic defect, this separation of the drum from the malleus handle is only carried out over 2 mm, leaving the umbo in its connection with the drum. On the other hand, if the umbo stays close to the promontory (Fig. 10.26), I do not hesitate to resect 1–2 mm of the peripheral end of the handle, in order to prevent central fixation of the reconstructed drum. With partial defects of the stapes, all remnants of both crura should be preserved, as they may stabilize an inserted columella (see step 9, ossiculoplasty). When there is complete destruction, interposition of a columella is indicated, and this is preferably carried out at a second operation if the first intervention identifies advanced pathology or a total defect and requires extensive grafting of the lateral tympanic and posterior canal walls. Dissection of the tympanic cavity should always be executed in such a way as to allow subsequent implantation of free grafts. Bone removal is reduced to what is absolutely necessary to visualize diseased areas. For this purpose, some bone can be removed very cautiously when it presents an obstacle, but every possible millimeter should be preserved to provide support for grafts subsequently. Finally, the remaining parts of the osseous annulus, lateral attic wall, and meatal roof should be sculptured flat, in order to avoid excessively concave infolding of a graft, which would result in a shrinking process with lateral displacement from the manubrium. Particular attention is also given to creating a flat transition between the planes of the new drumhead, the attic, and the new posterior canal wall. However, the interior of the middle ear should be redesigned in such a way as to restore natural ventilation and drainage. This can be achieved through prudent enlargement of normally narrow areas such as the isthmus between the tensor tympani ridge and the anterior epitympanic roof. The facial isthmus between the facial nerve and the lateral attic wall can also be widened by carefully adjusted thinning of the bony lateral attic wall. Finally, the aditus ad antrum—often narrowed by a Körner’s septum or by a low tegmen epitympani—should be overcorrected with limited resection of its roof. The optional resection of the malleus and incus mentioned above (Fig. 10.27) is consistent with these strategies, and can contribute substantially to the definitive cure of chronic mastoiditis. Step 9: ossiculoplasty. Complete reconstruction of a defective ossicular chain is of supreme importance for the audiological results in tympanoplasty. In my opinion, however, the technology involved in ossiculoplasty—e.g., the shapes and materials used for the implanted material—has been overemphasized in the literature in comparison with the fundamental biological parameters that are relevant in tympanoplasty. The quality of steps 4 to 8, therefore (management of the middle ear spaces) may have a greater impact on the functional outcome than any detail of step 9 (ossiculoplasty). Looking at the tables for audiological figures from different centers and comparing the various materials used, one may be disappointed by the unconvincing results, despite the promising technical properties of the implanted prostheses. In our department, the options for ossicular chain reconstruction have basically been reduced to the following six. These are based on a new classification of the different types of ossicular chain reconstruction that preserves Wullstein’s classification, with its worldwide acceptance, but includes contemporary techniques in a more realistic order (Table 10.1).
 Clinical Entities
Clinical Entities


 Symptoms, Signs, and Diagnosis
Symptoms, Signs, and Diagnosis
 Differential Diagnosis
Differential Diagnosis
 Indications for Surgery
Indications for Surgery
 Surgical Techniques
Surgical Techniques
Myringoplasty using the Underlay Technique
Endaural Tympanomeatoplasty (Bridge Technique)
Exposure of the Middle Ear


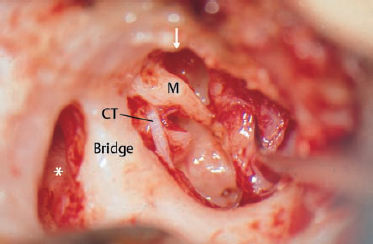
CT Chorda tympani
M Malleus
VII Facial nerve
Removal of Pathology
VII Facial nerve
Reconstruction of the Sound Transformer
| I | Ossicular chain intact | Mobile stapes-incus-malleus chain |
| I r | Reconstructed ossicular chain with lever function | Defect of ossicular chain bridged |
| II | Ossicular chain without malleolar lever function | Malleus defect. TM contacts incus. |
| III | Extended tympano-stapedo-pexy | Mobile stapes with extension to tympanic membrane in normal tympanic cavity, various interposition models |
| III l | Low ossicular chain | Classic connection between mobile stapes and tympanic membrane without extension, shallow tympanic cavity |
| III c | Columella-type chain | Absence of stapes. Stapes prosthesis on mobile footplate, normal or shallow tympanic cavity |
| III i | Columella–inner ear-pexy | Interposition of stapes prosthesis between tympanic membrane or malleolar handle and vestibule (malleovestibulopexy) or cochlea (cochleostomy) |
| IV | Chainless cochlear stimulation | Open oval niche, round window shielded with shallow tympanic cavity |
| X | No sound conduction | No contact between tympanic membrane and oval window |
- Intact ossicular chain: care is taken to ensure undisturbed mobility.
- After transection of the long process and removal of the body of the incus: fixation of the long process to the drum membrane (natural elevation of the stapes).
- Defect in the long process, stapes functioning: interposition of an autograft or alloplastic material between the head of the stapes and the drum membrane (stapes elevation) or, if possible, reconnection of the defective incus with the stapes using an interposed prosthesis.
- Absence of the stapes: insertion of auto- or homograft or alloplastic material between a mobile footplate and the drum membrane (columella).
- Problem-free radical cavity, open oval niche with mobile footplate, good spontaneous hearing: type IV tympanoplasty (oval window unshielded against the external auditory canal, round window sound-protected in a narrow hypotympanic cavity). This is a very rare indication.
- Fenestration of the oval window or fenestration of the promontory for rare cases of inaccessibility of the oval window (cochlear fenestration). Interposition of a prosthesis between this new window and the malleus handle (malleovestibulopexy or malleocochleopexy), or a comparable principle. If the malleus handle is absent, a piece of bone can be implanted into the drum membrane, to which a wire prosthesis can be fixed during a second procedure (dumbbell principle).
Some facts should be noted here. The original Wullstein type II was a theoretical notion, since without a malleus the incus cannot work as a transducer with a lever function. Instead, the sound waves are directly conducted to its long process, which serves as an elevation of the stapes. In our option no. 2 (natural stapes elevation), this principle is easily achieved by gluing the mobile end of the long process to the new drum membrane. One can also support it using the chorda tympani underneath (Fig. 10.28). However, if there are mucosal defects, or if there is a tendency for adhesions to develop, the chorda should not be placed under the stapes elevation. Its vicinity to the facial canal could result in progressive formation of adhesions, pulling the tympanic membrane down into the facial isthmus. In these problematic ears, the formation used in option no. 3 (the stapes rider) is preferable.
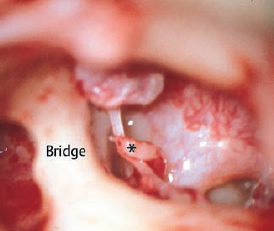
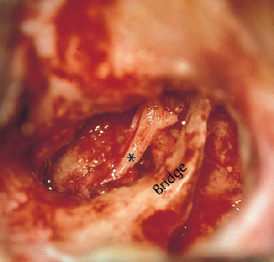
Fig. 10.29 Type III ossiculoplasty with elevation of a mobile stapes using a rotated umbo (*): malleostapedopexy. The neck and head of the malleus are resected and the incus is removed.
Wullstein’s original type III consisted of a bare stapes in contact with a limited drum membrane, reaching only to the facial canal, since Wullstein removed the lateral attic and the posterior canal walls and established a meatomastoid cavity. Our type III, by contrast, takes advantage of a drum membrane with a normal or slightly enlarged diameter at a normal distance from the oval window, since the natural support for the drumhead provided by an osseous annulus is preserved or reconstructed. Our type III therefore always implies that the stapes is elevated by interposing a piece of bone or other material (the stapes rider). The principle is to establish direct acoustic contact between the drum membrane and a mobile, elevated stapes, without a lever effect.
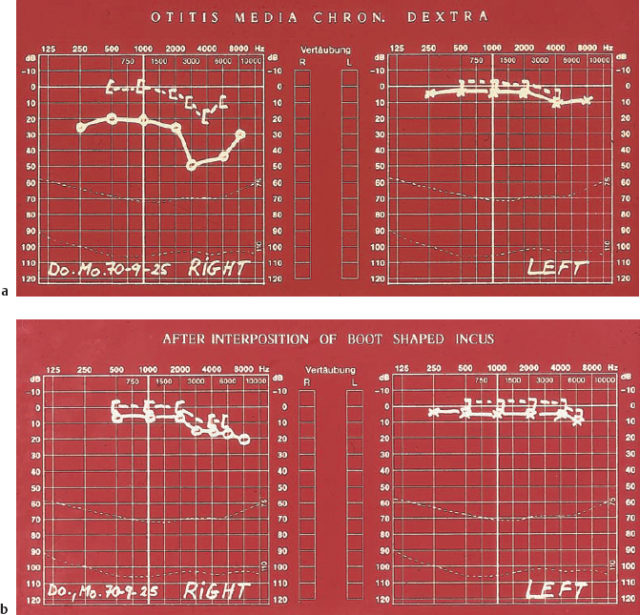
Various modifications have been tried and evaluated for achieving stable elevation of a mobile stapes (Moretz 1998). This is an area that challenges the surgeon’s imagination. Since autografts are basically preferred to alloplastic material in our department, advantage is taken of the actual situation observed in each individual case. An intact ossicular chain (type I) is respected as the best acoustical solution. One of the most frequent problems is interruption of the long process of the incus in the presence of a mobile stapes. Prostheses are available to bridge this defect. Earlier attempts to establish sound conduction by simply interposing a piece of bone or cartilage have not proved satisfactory. The manubrium of the malleus can also be rotated on top of the stapes head, either with its umbo after mobilization of the tensor tendon (Fig. 10.29), or with its neck, if the umbo has been left integrated into the drum. A free piece of bone from the head of the malleus can be shaped into an appropriate form and pierced by the malleus handle, so that it functions as a well-fixed stapes rider. The body of the incus, sculptured into the shape of a ski boot, has proved particularly convenient. It is placed with its upper, hollowed end over the stapes head, and with its sole facing the drum membrane (Fig. 10.30). It can stand free, or can be leant against the malleolar handle for stabilization. It is important that the sole should provide a comparatively large area of contact, transmitting more acoustic energy than the point-like contact with a simple rod-like stapes rider (Fig. 10.31). Whatever kind of stapes rider is chosen, it should be slim, not fat, in order to enhance conduction at higher frequencies and avoid contact with the facial nerve canal.
When the body of the incus or the head of the malleus are not available for carving a rider, one must resort either to prefabricated homografts (Messerli et al. 1994) or alloplastic materials. We have tried a wide variety of substitute materials, with variable results. Neither Micropore, nor ceramics, nor glass have produced consistent results without disappointment. At present, there is a trend in the literature toward resuming the use of metals—with gold and titanium being the favorites at the end of the 1990s. In our department, gold has been found extremely useful. It is flexible to a certain extent, but at the same time rigid enough to provide stable contact. If an alloplastic prosthesis is needed to elevate the stapes in the absence of a malleus head or incudal body, a partial ossicular replacement prosthesis (PORP) (Hütten-brink 1997) can be successfully used (Fig. 10.32). Other authors use autogenous material such as cortical bone, or prefer to use homologous teeth.
If the stapes superstructure is missing as well as the incus and malleus, a total ossicular replacement prosthesis (TORP) has to be interposed to transmit sound energy from the drumhead to the inner ear. This type of direct contact with the mobile footplate is created by a columella. Homografts such as a homologous malleus or incus are good for interposition (Fig. 10.33), but these are now less widely used, for virological reasons. Metallic prostheses made of gold or titanium compete with ceramic prostheses, which have to be carved into an appropriate shape. In our department, the gold TORP is preferred for audiological reasons, as well as cost considerations. No matter which alloplastic substitute is chosen—both for the stapes rider and the columella option—the peripheral end of the prosthesis has to be covered with a piece of cartilage, which is interposed between the drum and the prosthesis (Fig. 10.34). Unshielded contact between the membrane and the metal would result in gradual extrusion of the metal.
The classic type IV tympanoplasty (open cavity with a reduced drum membrane reaching to the promontory) is not consistent with the natural configuration of a tympanic cavity. It is therefore not an option for endaural tympanomeatoplasty. Exceptionally, it may be created if it is intended that a radical cavity should persist, and if the oval window has spontaneously epithelialized and audiometry has shown evidence of favorable sound conduction.
All types of columella have the disadvantage that the contact with the footplate is initially loose if they are not anchored in it. Fixation can be achieved using a columella with a spike on its base that can be inserted into a small groove drilled into the center of the footplate—the “spandrel” proposed by Fisch. I would not risk drilling into a footplate in the presence of manifest middle ear infection. The patient should therefore be prepared to undergo a second minor tympanotomy for readjustment. A second intervention also reduces the risk of inner ear infection, which is always present when there is extensive dissection of the footplate at the initial session.
In rare cases of footplate fixation due to chronic otitis media, a second operation with platinectomy and establishment of a stapes prosthesis is indicated. The peripheral end of the prosthesis is fixed to a persistent manubrium of the malleus, or to a small bone graft (Fig. 10.35) interposed into the tympanic membrane graft (dumbbell type). Another rare option is fenestration of the promontory, when there is insurmountable occlusion of the oval window. This is exceptional in chronic otitis media, but it may be indicated in middle ear malformations.
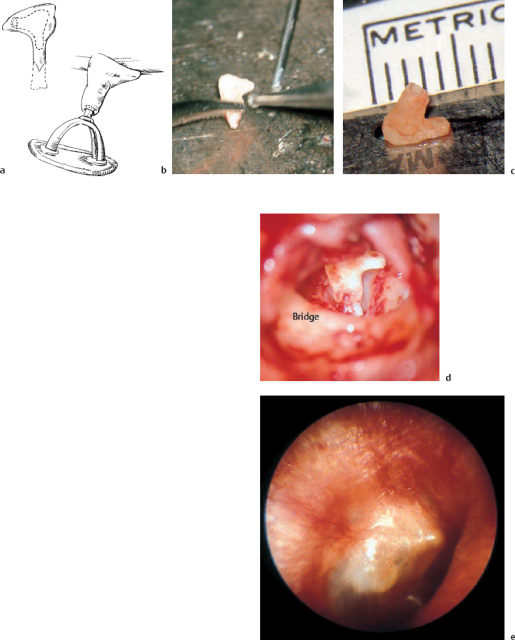
Fig. 10.30 Sculpturing a boot-shaped autograft from a defective incus. a The dotted line marks the outline of the new incus. b Carving with a diamond drill. c The new ossicle, with a hollow shaft. d The ossicle in place. e Incorporation after one year.
Reconstructing the Walls
Step 10: harvesting grafts. The endaural skin incision is sufficient to expose the temporalis muscle and harvest appropriately sized pieces of fascia (see Fig. 1.6, p. 9). If this was already removed during previous surgery, the periosteum below the muscle provides adequate material. Large amounts of mastoid periosteum can also be accessed and obtained using the endaural approach. If more soft tissue is required, an additional postauricular skin incision can provide almost unlimited areas of fascia or periosteum. Cartilage can be taken from the tragus or from the ipsilateral auricle, or both. Short skin incisions on the tragal edge, or on the back of the auricle, allow excision of appropriate pieces. The resulting pouches are glued together, and a few monofilament skin sutures close the procedure.
Step 11: closure of the tympanic and epitympanic cavities. The placement of free grafts to close the middle ear follows the principles required for reconstruction in an approximately natural form. Both the lateral attic wall and the tympanic cavity are closed simultaneously. If the lateral attic wall has been removed or reduced by about 50%, a triangular piece of cartilage is put in its place and fixed to the bony bridge by laying its partly stripped perichondrium over the bone—imitating the scutum and providing support for the tympanic membrane.
All three outer walls of the middle ear, tympanic membrane, lateral attic wall, and posterior meatal wall, are basically reconstructed with soft tissues such as fascia, perichondrium, or cartilage. These are covered as far as possible with local mobilized canal skin and the remnants of the tympanic membrane, but are left uncovered to a certain extent to allow secondary, spontaneous epithelialization. This principle has advantages over the implantation of split-thickness or full-thickness skin grafts, which can lead to complications due to hairs and sebaceous glands. On the other hand, it also has disadvantages such as intermediate transudation and the need for prolonged postoperative treatment.
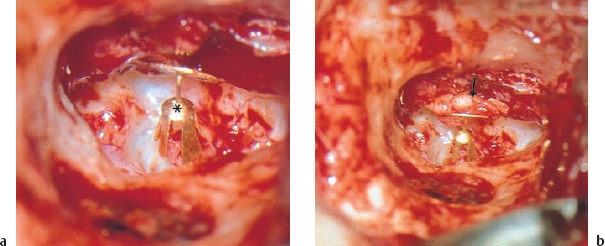
Fig. 10.32 A patial ossiciular replacement prosthesis (PORP) in situ. a Fixation on the stapes head (*). b Protection of the tympanic membrane with underlaid cartilage (arrow).
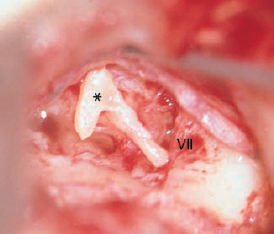
Fig. 10.33 A homologous columella (*) in position, carved from an intact incus (left ear).
VII Facial nerve

Fig. 10.34 A total ossicular replacement prosthesis (TORP) made of gold. a The outer surface of the round plate is covered with a piece of cartilage, which is fixed to the metal by using tissue adhesive to attach it to a small amount of fascia on the inner surface of the metallic frame. The cartilage is glued to the tympanic membrane. b Incorporation after one year.
The tympanic membrane is usually repaired with temporalis fascia, using the underlay technique. Small defects are plugged from inside with a piece of fascia, underlapping by about 1–2 mm (Fig. 10.7). With large central perforations, it is reasonable to transect the ring of the residual tympanic membrane posteriorly, forming superior and inferior tympanic flaps (Fig. 10.20), which are placed over the fascia that has been inserted anteriorly below the annulus and laid posteriorly over the osseous annulus and bony bridge. Larger defects are closed using a free graft of temporalis fascia, which is placed over the skeletonized manubrium and pushed under the margins of the defect (Fig. 10.36). It should also cover the full extent of a newly created lateral attic wall, reconstructed with cartilage. If sufficient perichondrium is available, this has also proved valuable (Goodhill 1967, Goodhill et al. 1964). Many authors consider that there is a risk of lateral displacement of the newly grafted tympanic membrane due to scar retraction if the fascia is placed over the malleolar handle, and they consequently prefer to place the fascia below the manubrium. I have found that this technique encourages tight synechia between the reconstructed tympanic membrane and the promontory. For this reason, I always lay the fascia over the manubrium, and have not often observed lateral displacement. The important factor for incorporation of the graft on the exact plane of the drumhead is to introduce it precisely below the margins of the defect. Broad contact between the graft and the skeletonized handle provides good chances of a close junction down to the umbo. The umbo itself has to be resected if it is positioned within 1 mm of the promontory. Otherwise, broad adhesion can be expected.

Fig. 10.35 Dumbbell prostheses for tympanovestibulopexy. A wired piece of autogenous bone shaped for interposition between the tympanic membrane and the oval window and serving as a total ossicular replacement prosthesis. The bone is fixed during an initial intervention, and platinectomy follows at a second session.
Gentle tightening of the fascia is recommended to prevent it from folding and sagging into the cavity. One drop of tissue adhesive will normally be sufficient to fix the inserted graft firmly to the overlying canal skin and bony frame. It should be emphasized once again that this osseous ring must remain in flat continuity with the posterior canal wall in order to reduce the lateral surface tension and minimize the danger of lateral displacement of the new drumhead.
When there are subtotal defects in the drum, and particularly when there is manifest ulceration of the tympanic mucosa—with a risk of broad contact between the graft and the medial wall—it is recommended to establish a new drumhead consisting of cartilage (Jansen 1963, Heermann J 1967) (Fig. 10.36b). The inner surface of the cartilage should be denuded to reduce the chance of new adhesions developing. The outer surface of the cartilage should support the perichondrium, as this promotes incorporation and spontaneous epithelialization. The cartilage should not overlap the bony annulus, but should fit snugly into the framework of bone. If the cartilage is not too thin and heavy, using it as a new drum provides satisfactory audiological results after a period of a few months, during which it is apparently remodeled internally, becoming more flexible.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


