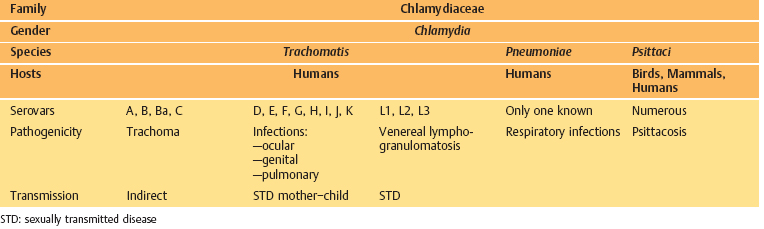
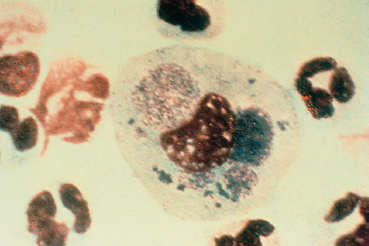
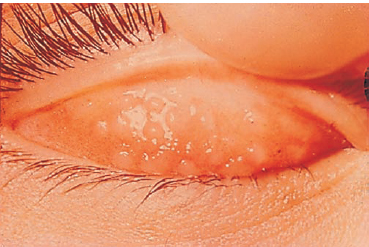
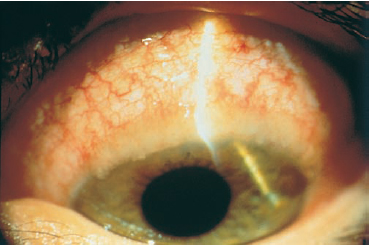
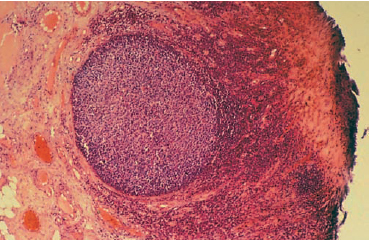
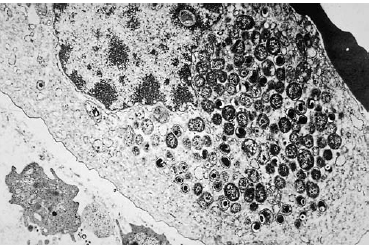
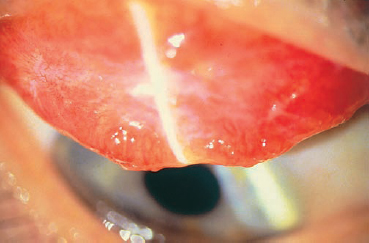
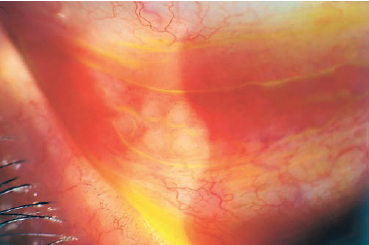
Chapter 7 Chlamydial Conjunctivitis Fig. 7.1 Florid-stage trachomatous conjunctivitis: follicles and papillae (courtesy of Dr. Chauvin, Montpellier) Fig. 7.2 Superior limbal follicles in florid trachoma Fig. 7.3 Conjunctival trachomatous follicle in early-stage florid trachoma: it consists mostly of small lymphocytes (Courtesy of Professor Nguyen Duy Tän, Hanoi) Fig. 7.4 Electron microscopic micrograph of a reticulate body: note the abundant elementary bodies (Courtesy of Dr. A. Péchinot, Dijon) Fig. 7.5 Cicatricial-stage trachoma: fibrous conjunctival scars It is disturbing that trachoma should still be associated with such a high morbidity rate: highly effective antibiotics are available and prevention is simple (in theory, at least), being based on elementary hygiene. Unfortunately, epidemiological data show that this infection, which is an excellent worldwide indicator of poverty, is still widespread at the beginning of this new millennium. Those who feel unconcerned by the ocular manifestations of chlamydial infection are mistaken. Population movements and immigration mean that all specialists will encounter trachoma sooner or later, perhaps not in its florid form, but certainly the chronic or cicatricial form. Travel to endemic regions (trachoma is still present in some countries from which it has officially been eradicated) and participation in humanitarian missions provide abundant opportunities to apply knowledge of this disease in practice. Inclusion conjunctivitis in adults, which was often suspected but rarely proved in patients with isolated chronic follicular conjunctivitis, is more problematic in industrialized countries. This chapter will provide an update on progress in the biological diagnosis of this contagious disease. Trachoma has been known since antiquity. Chinese texts dating back to the 22nd century BC describe the treatment of trichiasis. In 1907, Halberstaedter and Von Prowasek were the first to notice, on Giemsa-stained smears of conjunctival scrapings from patients with trachoma, intracytoplasmic granulations that they named inclusions.1 They inoculated the disease by the subconjunctival route to baboons, which developed conjunctivitis characterized by follicles containing cells bearing inclusions. In 1909 similar inclusions were found on a conjunctival smear from a newborn with conjunctivitis, and also in the mother’s cervical smear. A few years previously there had been reports of outbreaks of conjunctivitis in adults that resembled attenuated forms of trachoma and were contracted in swimming pools (hence the name “endemic swimming pool conjunctivitis”).2 Chlamydial inclusions (TRIC agent, for trachoma inclusion conjunctivitis) were detected and the venereal mode of transmission was demonstrated.3 In 1924, Favre described inclusions in lymph node cells from patients with lymphogranuloma venereum.4 During a pandemic of psittacosis (from the Latin psittacus, meaning parrot), Bedson observed inclusions similar to those associated with trachoma in macrophages of mice inoculated by the intraperitoneal route with sputum from patients with severe pulmonary diseases.5 He thus succeeded in identifying the agent responsible for psittacosis as an obligate intracellular filtrable parasite, and also isolated it. Thygeson, in 1934, was the first to establish a link between the psittacosis agent and the intracellular inclusions associated with trachoma. All infections characterized by these intracellular inclusions are due to members of the chlamydiae. The technique recommended by Tang in 1957 of isolating the agents of trachoma in chick embryo6 has been superseded by culture on irradiated MacCoy cells, a method first described by Gordon and Quann in 1965.4 General Considerations Nomenclature The family Chlamydiae contains a single genus, Chlamydia, and four species: C. trachomatis, C. pneumoniae, C. psittaci, and C. pecorum (Table 7.1). Chlamydia trachomatis is responsible for trachoma (serovars A, B, Ba, and C), inclusion conjunctivitis, urethritis, epididy-mitis, cervicitis, salpingitis, otitis and pneumonia (serovars D-K), and lymphogranuloma venereum (serovars L1, L2, and L3). Chlamydia pneumoniae, responsible for respiratory infections, has only one known serotype. Chlamydia psittaci, the psittacosis agent, has many serovars, which have not yet been characterized but appear to fall into three groups.4 Little is known about Chlamydia pecorum7 Bacteriology Chlamydiae are Gram-negative bacteria equipped with both RNA and DNA. Strictly intracellular, they can only develop by parasitizing a living cell. They occur in different forms: —Elementary bodies measure 0.1-0.3 mm in diameter; they have no metabolic activity but are capable of infecting host cells. Their wall contains a polysaccharide rich in α2-keto-3 deoxyoctanoic acid, the antigen characteristic of the family Chlamydiae8; —Reticulate bodies measure about 1 mm in diameter; they have their own metabolic activity and are incapable of infecting host cells; —Inclusions consist of colonies of various sizes and shapes. Their variability is due to the different stages of the chlamydial life cycle. The Chlamydial Life Cycle The life cycle takes about 70 hours from infection to host cell lysis9 and is strictly intracellular. The Elementary Body Phagocytosis of the elementary body is the first step in the infectious process. The host cell provides the necessary energy for phagocytosis, via its mitochondria. Once inside the cell the elementary body surrounds itself with a vesicle, forming a phagosome that protects it from attack by lysosomes. Table 7.1 Classification of the Chlamydiaceae The Reticulate Body Once inside a phagosome, the elementary body transforms within a few hours into reticulate bodies, which are themselves grouped into morulae. Reticulate bodies are the reproductive form of chlamydiae inside the host cell. As they divide they form “inclusions,” which eventually occupy the entire cytoplasm. At this stage of their development, chlamydiae are visible by light microscopy.8 Finally, the host cell bursts, and the released elementary bodies infect new cells4 (Fig. 7.4). The Intermediate Body The intermediate body, a transition form between the elementary body and the reticulate body, possesses a central DNA pseudonucleus surrounded by ribosomes. Immunity Many animal models have been used to study chlamydiae. Mice seem to be most suitable experimental animals,10 although the primate species Macaca nemestrina is particularly useful for studying chlamydial infection in children.11 The immunological phenomena triggered by chlamydial infection have been partly elucidated. Cell-mediated immunity seems to play an important role in the pathogenesis of the conjunctival scars seen in trachoma.12–14 Humoral immunity does not prevent reinfection,15 and the severity of the lesions could be related to repeated infection.16 Attempts at vaccination have failed.17,18 Clinical Aspects Chlamydia trachomatis Trachoma Epidemiology Trachoma is the most serious form of ocular involvement by C. trachomatis. It is the leading cause of blindness in developing countries, accounting for 6-9 million cases of blindness worldwide. Nearly 80 million children are also at risk of visual impairment because of inflammatory trachoma.19 Trachoma is a public health problem in Africa, southern Asia and some parts of South America, Australia, and the Pacific islands. A study in Tanzania, an endemic region, showed that 54% of children and 9% of women had inflammatory trachoma.20 In another study conducted in the same country, Bobo detected C. trachomatis by means of polymerase chain reaction (PCR) in the conjunctiva of one quarter of 234 children with no signs of ocular infection.21 Trachoma is associated with poverty. Its transmission occurs through direct or indirect contact with infected materials (hands, clothes, towels), or through flies landing on the face and inoculating the eyes directly.22,23 The presence of young children and a lack of toilets in the home are supplementary risk factors.24 There is no gender difference in prevalence.25 Clinical Aspects Trachoma, formerly known as granular conjunctivitis, is a contagious disease that is rarely encountered in industrialized countries, except among occasional infected immigrants arriving from endemic regions. It is nonetheless crucial to know how to diagnose this condition, which is still the leading cause of blindness worldwide. Its spontaneous course is chronic, lasting many years. The diagnostic criteria for trachoma are a corneal pannus, conjunctival follicles, characteristic conjunctival scars, and Herbert pits. The diagnosis of trachoma is established when two of the four criteria are found. The traditional classification of McCallan, introduced in 190826 and modified in 1952, comprises four stages of progression based on the external aspect of the superior palpebral conjunctiva. However, it does not take into account the severity of inflammation, and does not distinguish between sight-threatening lesions and others. Stage I: trachoma incipiens The initial symptoms are those of mild conjunctivitis characterized by conjunctival follicles and papillae at the upper edge of the superior tarsus. Onset can be very insidious, with mild tearing and a sensation of heavy lids. The diagnosis is often made during routine examinations as part of screening campaigns in endemic regions. In children less than two years old the papillary reaction and inflammatory thickening of the conjunctiva can predominate.27 The pannus tenuis is also an early sign of trachoma, with limbal infiltrates attracting conjunctival vessels that form relatively characteristic fine arcades. Stage II: florid trachoma Marked symptoms are present, with a foreign-body sensation, discomfort beneath the lids, photophobia, and marked tearing. Pseudoptosis frequently occurs, giving the patient a sleepy appearance. Stage IIA is characterized by an increase in the number and size of follicles, not only on the superior tarsal conjunctiva, but also on the lower tarsal conjunctiva, and in the two fornices. They carpet the tarsal conjunctivas with a frog-spawn appearance (Fig. 7.1). They can necrotize and burst under the pressure, exuding a yellowish material. Although they have a characteristic (but nonspecific) histological aspect (Fig. 7.3), conjunctival biopsy has been supplanted by less invasive and more sensitive diagnostic techniques (see p. 127 ff), and the diagnosis is based on clinical signs at this stage anyway. Stage IIB: papillary hypertrophy accompanies the follicles. The papillae take on various forms, from small red spots at the surface of the conjunctiva to dilated and congestive capillary tufts. At this stage the chlamydiae have invaded the corneal epithelium and attracted lymphocytes and mast cells; these stimulate the proliferation of limbal vessels toward the cornea, under the Bowman’s layer, forming a vascular pannus.28,29 This translucent pannus is qualified as vasculogranular because of the infiltrates and follicles that can accompany the vessels. The trachomatous pannus extends from the superior limbus to the center of the cornea, its long vascular arcades appearing to fall vertically, “like rain.” In the limbus, the follicles juxtapose to form a gelatinous infiltration of yellow-greenish color (“limbal sago,” “pearl diadem,” “trachoma rosettes”) that sometimes become highly exuberant (Fig. 7.2). Nodules or follicles present in the pannus (especially at its base) can break to the surface, where they leave, on healing, characteristic small depressions called “Herbert peripheral pits.” Stage III: precicatricial trachoma This stage marks the beginning of the cicatrization process, which accounts for the gravity of trachoma. It occurs at a variable interval after the initial infection. Areas of follicular necrosis heal, causing sclerosis of the conjunctiva and underlying tissues.30 These conjunctival scars may be linear, stellar (scars of retracted follicles), but can also be deep and widespread. Calcifications (concretions) sometimes replace the follicles. At this stage the pannus has reached its maximal size. The degree of conjunctival scarring is directly proportional to the intensity and duration of inflammation.31 Stage IV: cicatricial trachoma Occurring very late, cicatricial trachoma consists of multiple fibrous scars that converge toward a white horizontal line on the superior palpebral conjunctiva, parallel to the eyelid margin (Arlt’s line). The underlying conjunctiva is smooth and pale (Fig. 7.5). This stage is also characterized by an entropion-trichiasis of variable degree. Inflammatory signs have disappeared and the disease is no longer contagious. A simplified description of trachoma for primary health-care workers was introduced by the World Health Organization (WHO) in 1987. It includes corneal, conjunctival, and palpebral signs that are identified with the assistance of a loupe and handlight32: —TF (trachoma follicles): five or more follicles on the upper tar-sal conjunctiva; —TI (trachomatous inflammation): diffuse inflammation of the upper tarsal conjunctiva obscuring at least 50% of normal deep tarsal vessels; —TS (trachomatous scarring): trachomatous conjunctival scarring; —TT (trichiasis): at least one deviated eyelash touching the eyeball; —CO (corneal opacity): corneal opacity or scarring. A new, more detailed classification has also been developed by the WHO. It takes into account the severity of the inflammation in terms of the tarsal papillary response (P) and the tarsal follicular reaction (F). This more detailed description is useful for field studies.33 —Papillary response (P): papillary hypertrophy and diffuse infiltration of the superior tarsal conjunctiva —Follicular reaction (F): follicles on the superior tarsal conjunctiva The intensity of inflammation can thus be scored as follows: —Severe: P3 and F —Moderate: P2 and F3 —Mild: P and F2 —Insignificant: P, and F0 or F1 Complications —Palpebral complications: the entropion-trichiasis results from cicatricial retraction of the tarsus. The lashes are turned in toward the cornea and cause complications such as ulceration and vascular infiltration, which can affect the entire corneal surface. Interindividual variations in orbicular function would explain why not all patients develop trichiasis.34 —Corneal complications: at the stage of cicatricial trachoma, the cornea remains vascularized but the vessels are thinner. The surface is highly irregular, with a facetted appearance due to the scars left by follicle resorption and various infiltrates. Patients may then develop superficial punctate ker-atitis (generally on the upper part of the cornea), anterior stromal inflammatory infiltrates, reactivation of superficial neovascularization, and ulceration worsening the opaque, astigmatogenic scars. These complications are mainly due to dryness and entropion-trichiasis. The most severe complications are perforation and xerosis. —Conjunctival complications: fornix foreshortening and severe dry eye syndrome associated with destruction of goblet cells.35 The terminal stage consists of xerosis, with an opaque and keratinized cornea and conjunctiva. —Lacrimal complications: atresia of the tear duct orifices, dacryocystitis, and dacryoadenitis. —Infectious complications: bacterial infections are extremely frequent and cause corneal ulcers associated with vascular ingrowth. —Eyelash changes: hypertrophy or, on the contrary, atrophy or rarity of lashes (madarosis).36 Adult Inclusion Conjunctivitis Epidemiology While trachoma is due to C. trachomatis serovars A, B, and C, adult inclusion conjunctivitis is due to serovars D, E, F, G, H, I, J, and K.37 Both are oculogenital conditions. The bacterial reservoir is the genital tract of a sexually active adult. Transmission to the eye occurs by direct contact with infected genital secretions,38 or by indirect contact in an inadequately disinfected swimming pool, hence the term “swimming pool conjunctivitis.”2,3 Direct eye-to-eye transmission is possible but very rare,39 and indirect infection can also occur by contact with contaminated inert surfaces.40 Adult inclusion conjunctivitis represents 6-19% of all cases of chronic bacterial conjunctivitis.39,41,42 It mainly occurs between the ages of 15 and 30 years.27 More than 90% of women with positive ocular cultures for Chlamydia also have positive genital cultures.43 Improvements in detection techniques may explain the apparent increase in the number of cases of ocular chlamydiosis. Extraocular Manifestations Urogenital chlamydiosis Sexual liberation in industrialized countries led to a rise in the frequency of sexually transmitted diseases (STD), and especially genital infections by Chlamydia. Genital chlamydiosis is the most frequent STD. Chlamydia trachomatis is found in 5-20% of asymptomatic women. The patients most at risk are between 20 and 30 years of age.44 In women, the infection can cause urethritis, cervicitis, endometritis, salpingitis (responsible for a large proportion of cases of infertility), and perihepatitis (Fitz-Hugh-Curtis syndrome). In men, it causes epididymitis, balanitis, prostatitis, and urethritis. Other sites of involvement include the pharynx and anus, while oral, neurological, and cardiac involvement is rare. Ocular Signs The incubation period ranges from 2-19 days. The first symptoms of conjunctivitis may occur abruptly or more slowly, with ocular hyperemia, often associated with blepharitis, mu-copurulent secretions, a foreign-body sensation, and photophobia. Itching and burning sensations are rarely mentioned. In most cases the conjunctivitis is initially unilateral, papillary, and accompanied by ipsilateral preauricular ade-nopathies. Spread to the other eye generally occurs later.45 On day 15 follicles develop on the inferior and superior tarsal conjunctivas46 (Fig. 7.6). The papillary response is more pronounced on the superior tarsal conjunctiva, while the follicular reaction is identical on the inferior and superior tarsal conjunctivas. There is also infiltration and thickening of the conjunctiva, but no pseudomembrane (although this can occur in infected newborns).30 In 30-85% of cases the course is complicated by corneal involvement, with a micropannus of 1-2 mm, epithelial punctate keratitis, or fine limbal subepithelial infiltrates.47 The combined presence of these latter two signs can mimic ade-noviral infection. Corneal neovascularization and conjunctival scarring are rare19 Unless treated, the condition becomes chronic, with disappearance of the conjunctival hyperemia but persistence of the subepithelial follicles, papillae, and nodules for many months. Fig. 7.6 Follicles on the lower palpebral conjunctiva in a case of adult inclusion conjunctivitis Table 7.2 Causes of chronic follicular conjunctivitis
P0 (absent): normal conjunctiva;
P1 (minimal): subconjunctival vessels visible;
P2 (moderate): conjunctival infiltration obscuring the subconjunctival vessels;
P3 (severe): thickened, opaque conjunctiva hiding the subconjunctival vessels over more than 50% of the tarsal conjunctival surface.
F0: no follicles;
F1: follicles present, but less than 5 on the central tarsal conjunctiva;
F2: 5 or more follicles on the central tarsal conjunctiva;
F3: 10 or more follicles on the central tarsal conjunctiva.
—Trachoma —Adult inclusion conjunctivitis —Molluscum contagiosum —Some causes of Parinaud’s oculoglandular syndrome: —Adenoviral keratoconjunctivitis —Toxic conjunctivitis (eyedrops, ointments, etc.) —(Allergic conjunctivitis) —(Lyme disease) |
Differential Diagnosis
Adult inclusion conjunctivitis is often missed because it mimics many other follicular infections (Table 7.2). Follicles are slightly elevated hemispheric, translucent, pale nodules about 1 mm in diameter. Fine vessels circumscribe the base, usually sparing the center. Clinically, follicles are distinguished from papillae, which are smaller and pinkish, and have a central vascular tuft and a vaguely hammerhead shape. In practice, however, the distinction is not always so clear: the two types of conjunctivitis are often confused, particularly as follicles are often accompanied by a papillary reaction. Histopathologi-cally, both lesions are characterized by subepithelial lymphoid hyperplasia, but the predominance of one or other form in a patient with conjunctivitis can contribute to the diagnosis. It is noteworthy that children can have asymptomatic folliculosis of the lower fornix, in the absence of inflammation; it is simply due to hypertrophy of adenoid tissue, which can be normally present in children.
Epidemic adenoviral keratoconjunctivitis is very similar to inclusion conjunctivitis, but its onset is more acute and the conjunctival hyperemia is more pronounced; in addition, the secretions are less thick and the corneal involvement occurs earlier. It should be noted that the two infections can coexist.48 There are many other forms of conjunctivitis mimicking chlamydial disease (allergy, herpes, rosacea, chronic blepharitis, Newcastle disease, etc.), which means that Chlamydia should be sought in patients with chronic or atypical forms.49 This can lead to the discovery of genital infection and cut the chain of infection,50 particularly in case of latent ocular chlamydiosis.51
Neonatal Inclusion Conjunctivitis
Epidemiology
Neonatal inclusion conjunctivitis is due to infection of the neonate during passage through the birth canal. It is the most frequent neonatal ocular infection.52 It affects 5-60/1000 newborns in the United States and 80/1000 newborns in Kenya.53 The risk of transmission by a genitally infected mother is 25-50%, but C. trachomatis, being difficult to detect, is found in only half these mothers.54
Clinical Aspects
Neonatal inclusion conjunctivitis usually occurs between days 5 and 15 of life, and, rarely, after 2 months. Initially unilateral, it becomes bilateral in half the cases.54 The conjunctival involvement takes the form of congestive, hyperemic, mucopurulent conjunctivitis without follicles (the adenoid layer is absent before the third month of life). The conjunctiva may bleed readily on contact. The lids are swollen. Inflammatory membranes can appear during the second week after onset. There is generally no corneal involvement, but complicated forms of superficial keratitis with a pannus, leaving corneal scars, have been described.55 Extraocular manifestations are also possible, such as otitis media and pulmonary involvement, the latter representing the main risk.56 Treatment leads to recovery within 1-4 weeks, with no visual sequelae.
Reiter’s Syndrome (see Chapter 9)
Reiter’s syndrome mainly affects young men with the HLA-B27 antigen. The latter appears to be an even stronger precipitating factor in patients already sensitized to C. trachomatis. 57 C. trachomatis is not the only cause of the syndrome, because only 70% of patients are seropositive for this species. Other pathogens such as Shigella, Salmonella, Yersinia, and Campy-lobacter spp have been implicated.58
The classic symptom triad, consisting of urethritis, arthritis, and conjunctivitis, is often incomplete, making the diagnosis more difficult. The arthritis is often asymmetric, and the urethritis moderate or asymptomatic.59 Mucocutaneous manifestations are possible, such as keratodermia (psori-asiform rash on the palms and soles) and circinate balanitis of the glans penis.
Conjunctivitis, the least present feature of the symptom triad, appears a few days after the urethritis. It is usually unilateral, moderate, and transient, and may go unnoticed.59 The conjunctivitis is papillary and follicles are rare. Uveitis and, more rarely, keratitis can occur.60
Lymphogranuloma Venereum
Lymphogranuloma venereum occurs in three phases:
—The inoculation chancre, which is usually genital (or rectal in homosexual men) and sometimes goes unnoticed;
—The bubonic stage: crural and especially inguinal lymph nodes progressing to suppuration and possibly fistulization, associated with systemic signs;
—The tertiary stage, which is chronic and accompanied by very rare late complications (fistulae, rectal stenosis, genital elephantiasis, meningitis, and pneumonia).
Chlamydia trachomatis serovars L1, L2, and L3 are responsible for the ocular involvement, which is very rare. Transmission to the eye occurs by sexual contact, but accidental inoculation has been reported among laboratory personnel. The incubation period is variable, sometimes as long as 30 days. The ocular involvement is known as “Parinaud’s oculoglandular syndrome” (see Table 9.6), which consists of generally unilateral conjunctivitis, with macrofollicles and papillary hyperplasia. It usually only affects the superior palpebral conjunctiva and for-nices and is associated with often mucopurulent secretions and voluminous inflammatory preauricular and submaxillary lymph nodes. The associated keratitis is characterized by the presence of a thick and large vascularized pannus of the superior limbus. Iridocyclitis is frequent.
Systemic therapy prevents fistulization of the lymph nodes and accelerates recovery of the conjunctivitis, which otherwise disappears spontaneously after a few months.
Miscellaneous
Some authors have suggested that vernal conjunctivitis could be related to chlamydial infection.37,61 The persistence of Chlamydia in the conjunctiva after birth would be responsible for sensitization to specific antigens. This would explain why allergic investigations are negative in 50 % of children with vernal conjunctivitis, but this needs to be confirmed.
Chlamydia Psittaci
Psittacosis is caused by C. psittaci, which infects a large variety of bird species (particularly parrots) and ruminants. Humans are occasional hosts, and are infected by inhalation of dust contaminated by the feces of infected animals. Chlamydia psittaci then lodges in the reticuloendothelial system and provokes acute or subacute symptoms such as fever, headache, and myalgia.62 The respiratory form causes atypical pneumonia, and the systemic form is septicemia. The diagnosis is based on the clinical course, and especially the patient’s lifestyle.
Ocular infections in humans63 mainly consist of abrupt onset follicular conjunctivitis, with preauricular adenopathies and epithelial and subepithelial corneal infiltrates.64 The conjunctivitis disappears after 1-3 months. A case of bilateral ker-atouveitis associated with cardiovascular and ear involvement has been described.65 Tetracycline therapy leads to recovery without sequelae.
Chlamydia Pneumoniae
Chlamydia pneumoniae infection is air-borne. It is responsible for mild respiratory disease that can be severe in fragile or im-munocompromised patients. Outbreaks can occur in institutions. The pulmonary infection generally has a subacute course and is difficult to cure, even with appropriate antibiotic therapy.66
Chlamydia pneumoniae can cause conjunctivitis in humans. A case of papillary and follicular conjunctivitis associated with rhinitis, without corneal involvement, has been described.67 Local and systemic therapy led to recovery without sequelae.
Laboratory Investigations
The diagnosis of trachoma is mainly based on clinical findings. Biological tests are rarely contributory, except for early forms in nonendemic areas and some chronic forms, when there is doubt as to the eradication of the infection.
In contrast, the diagnosis of chronic nontrachomatous chlamydial conjunctivitis is difficult, and any diagnostic delay can lead to aggravation of the lesions and/or dissemination of the infection. Biological tests are particularly useful in these settings, by identifying chlamydiae in the conjunctiva.
Chlamydiae possess three types of antigen:
—Group-specific antigen: lipopolysaccharide (LPS) or lipopoly-oside common to all members of the genus Chlamydia;
—Species-specific antigens, which are used to distinguish among the three species of Chlamydia. The most important is the major outer membrane protein (MOMP);
—Type-specific antigens, which identify the 15 serovars of C. trachomatis, the numerous serovars of C. psittaci, and the single serovar of C. pneumoniae.
Direct Diagnosis
Older direct diagnostic techniques such as staining with iodine, Lugol, and Giemsa (Fig. 7.7), which have poor specificity and sensitivity, have been superseded by cell culture, im-munolabeling with monoclonal antibodies, and molecular biology-based techniques.
Fig. 7.7 Cytological examination of conjunctival scraping: juxta-nuclear body, or Halberstaedter-Prowazek inclusion body (Giemsa staining)
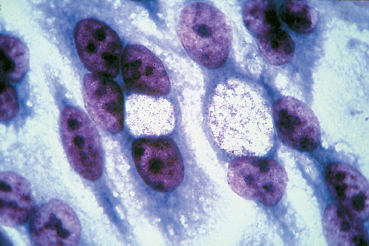
Fig. 7.8 Chlamydia trachomatis: large, negatively stained juxtanuclear inclusion (reticulate body) (cell culture, cresyl violet staining) (Courtesy of Dr. A. Pechinot, Dijon)
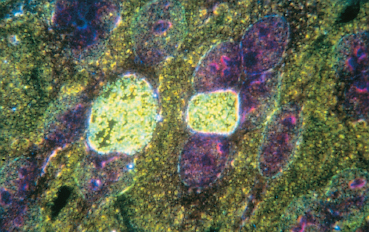
Fig. 7.9 Same inclusion as in Fig. 7.8, but on a dark background: the inclusion contains a multitude of points corresponding to elementary bodies ready to be released (Courtesy of Dr. A. Pechinot, Dijon)
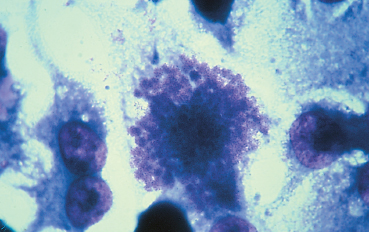
Fig. 7.10 Chlamydia psittaci: inclusion on the point of bursting (cresyl violet staining) (Courtesy of Dr. A. Pechinot, Dijon)
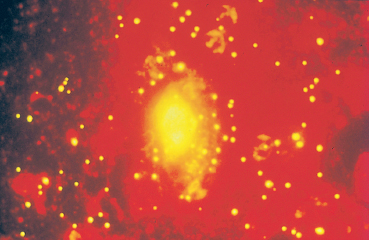
Fig. 7.11 Inclusion (reticulate body) revealed by direct immuno-fluorescence
Cell Culture
As chlamydiae are obligate intracellular parasites, viable cells must be used for culture:
—MacCoy cells are mouse fibroblasts,
—HeLa 229 cells are derived from a human cervical epithelial carcinoma.
The cells are irradiated or treated with a cytostatic agent (cy-cloheximide) to inhibit their division. The inoculum is centrifuged to increase bacterial adherence to the target cells.68
Under topical anesthesia, samples are obtained by swabbing or scraping the lower and upper tarsal conjunctivas with a dacron instrument, and are rapidly placed in culture or stored at -70°C.69 Cells infected by chlamydiae can be detected by means of direct or indirect immunofluorescence, or im-munoenzymatic techniques.
Cell culture is the reference method for detecting chlamydiae. Detection of a single inclusion is sufficient for diagnostic purposes. Specificity is 100%, but sensitivity ranges from 65-85%.70 Temperature variations during sample storage, transport and manipulation, and delays before inoculation are responsible for the numerous false-negative results.71,72 This is a difficult, complex and costly technique available in few laboratories (Figs. 7.8-6.10).
Direct Immunofluorescence (Fig. 7.11)
Monoclonal antibodies coupled to fluorescein are used to detect the MOMP of chlamydiae.73 The sample is fixed on the slide and considered positive if at least 10 elementary bodies are observed.74 Direct immunofluorescence has a specificity of 81-99% and a sensitivity of 80-99% according to the study.75,76 It can reveal residual elementary bodies persisting in the conjunctiva after the end of the phase of active infection.77 It is a simple, rapid and reproducible technique,78 but necessitates an experienced examiner: the difficulty in reading the slides may explain many false-positive results.79
Immunoenzymatic Techniques (ELISA)
The antigens are detected on the slide with monoclonal an-tipolysaccharide antibodies conjugated with an enzyme (alkaline phosphatase or horseradish peroxidase) and a revelation system based on enzymatic amplification. The intensity of the final staining reaction is measured by absorption spectropho-tometry at 450 nm. A sample is considered positive if its optical density is above the cutoff.
The specificity of this technique is 97-98% and its sensitivity 85-97% according to the study.76 Samples containing too few cells can give false-negative results.
Polymerase Chain Reaction
Polymerase chain reaction (PCR) amplifies a specific gene in three successive reactions: DNA denaturation, pairing of short fragments (primers of the target molecule) and synthesis of a new DNA molecule between the two primers by elongation (mediated by DNA polymerase). The three reactions are repeated at least 30 times, thereby amplifying the target fragment millions of times. Hybridization to a specific probe confirms the specificity of the amplification.80
The sequences chosen for amplification correspond to the MOMP gene, the endogenous plasmid, or 16S ribosomal RNA.81 Amplification of sequences corresponding to the endogenous plasmid rather than the MOMP gene increases the sensitivity of the technique by a factor of four.82 PCR can be coupled to an immunoenzymatic technique.21 Haller et al. obtained 100% specificity and sensitivity in a study of 558 conjunctival specimens from patients with chronic follicular conjunctivitis.83
Hybridization Probes
Radioisotopes and nonradioactive techniques (sulfonation, bi-otin, etc.) can be used to detect the C. trachomatis genome.84 The two DNA strands are separated and a labeled probe specific for the target sequence is bound to them.85 This very specific but poorly sensitive technique is not commonly used.
Indirect Diagnosis
Indirect diagnostic techniques are used to detect antibodies directed against chlamydial antigenic motifs in serum or tears.
Anti-LPS antibodies appear in the serum early after infection, while anti-MOMP antibodies reflect the later immune response. Simultaneous detection of these two antibodies is possible.83 In fact, serological tests are often of little use because circulating antibodies are already present in many patients.
Complement Fixation
The complement fixation reaction reveals antibodies directed against the common chlamydial antigen. It is an old technique with good specificity but poor sensitivity, and has virtually been abandoned.
Microimmunofluorescence
Microimmunofluorescence is used to distinguish among the three species of chlamydiae and the 15 serovars of C. trachomatis. This is a sensitive method, which consists of reacting a known antigen with a drop of serum or tears and revealing the complex with fluorescein-labeled anti-human immuno-globulin antibodies.
Immunoenzymatic Techniques (ELISA)
The detection of circulating antibodies by ELISA is simpler and less subjective than by microimmunofluorescence, and many samples can be tested simultaneously.
Guidelines
Rapid laboratory diagnosis is crucial for effective management of adult and neonatal chlamydial conjunctivitis.50 Many studies have been conducted to assess the sensitivity and specificity of the different techniques (Table 7.3).
The complexity of cell culture, together with its high cost and susceptibility to false-negative results,86,87 mean that this method cannot be used routinely.
In contrast, direct immunofluorescence has many advantages, including good sensitivity and specificity, low cost, and rapid diagnosis. However, it necessitates experienced personnel and can only be used to test a small number of samples at the same time.
Immunoenzymatic techniques (ELISA) are inexpensive and observer-independent, and can be used to test a large number of samples simultaneously. However, they are less sensitive than direct immunofluorescence and can give false-positive results.88
Polymerase chain reaction is highly specific and exquisitely sensitive. It is superior to direct immunofluorescence, ELISA, and cell culture89 but requires a well-equipped laboratory.
Serological tests are of little value in the diagnosis of localized chlamydial infection. The significance of anti-Chlamydia antibody detection in tears is not clear, mainly because of the possibility of antibody transudation from serum, especially in patients with genital chlamydial infection.89 As anti-Chlamydia IgA, but not IgG, antibodies have been detected in the tears of patients with genital chlamydiosis,90 detection of specific IGA may be useful in case of suspected chlamydial conjunctivitis when the antigens cannot be detected in the conjunctiva.91 This technique requires further evaluation.
Table 7.3 Laboratory diagnosis of ocular chlamydiosis
| Specificity | Sensitivity | |
|---|---|---|
| Cell culture | 100% | 65-85% |
| Direct immunofluorescence | 81-99% | 80-99% |
| Immunoenzymatic techniques (ELISA) | 97-98% | 85-97% |
| Poylmerase chain reaction (PCR) | 95-100% | 88-100% |
Trachoma
Medical Therapy
Trachoma being endemic in some regions of the world, curative or preventive therapy is crucial to avoid blindness. Treatment must be simple, effective, inexpensive, and safe.
Prevention
Key factors in the prevention of trachoma are improved living conditions and the teaching of basic hygiene rules such as hand washing. However, health education programs alone cannot improve the performance of mass treatment programs.92 One per cent ophthalmic tetracycline ointment twice a day or eye drops four times a day on at least five consecutive days each month for 6 months a year, or twice a day for 2 months, is the treatment of choice. This intermittent treatment schedule offers substantial advantages in terms of cost and personnel.18 There is no vaccine.
Curative Therapy
Curative large-scale treatment of trachoma consists of the mass topical application of 1 % tetracycline ophthalmic ointment or erythromycin twice a day for 2 months, combined with systemic therapy in patients with severe or moderate forms, as ocular samples again become positive one month after cessation of topical therapy alone.93 Systemic therapy for adults consists of 100mg of doxycycline, morning and evening for 3 weeks (or 4 weeks in case of marked inflammation). Pregnant women should be treated orally with 500 mg of erythromycin three times a day for 3-4 weeks, and children with 50 mg/kg per day erythromycin for 3 weeks. Chlamydia tracho-matis is very sensitive to sulfonamides.
Studies have shown the efficacy and safety of a new long-acting macrolide antibiotic, azithromycin, in the treatment of adults and children with trachoma. The dose regimens are 1 g and 20 mg/kg, respectively, as a single dose. With this treatment, 78% of patients no longer had active trachoma after 6 months, compared with 72% of patients who received conventional intermittent topical therapy (tetracycline or erythromycin eyedrops).94
One problem is that the systemic route is reserved for only certain indications because of the adverse effects encountered with most drugs, and that topical therapy, owing to its long duration, carries major problems of compliance.
The persistence of follicles 2-3 months after the beginning of treatment must not be interpreted as reflecting treatment failure. Nevertheless, the presence of chlamydiae has been demonstrated in the cornea and conjunctiva of patients apparently cured of trachoma for many years.37
Surgical Therapy
Surgical correction of cicatricial entropion and trichiasis is difficult, but is essential to eradicate trachomatous blindness. Electroepilation or cryotherapy can be performed to eliminate a few ectopic eyelashes irritating the cornea, but surgery is necessary in more advanced lid deformities. In poor regions, simple procedures must be used so that they can be performed by nonspecialized medical personnel or mobile teams. Indeed, in many regions of Africa patients do not even have access to hospitals, let alone ophthalmologists.95 The most effective techniques are lid rotation procedures. Simple tarsal advancement is ineffective when lid closure is incomplete.96 When feasible, more sophisticated techniques are preferable, such as marginoplasty with oral mucosal grafting and other forms of surgical palpebral reconstruction.
Surgery of the lacrimal excretory system is also part of the surgical therapy of trachoma (dacryocystorhinostomy, dacryo-cystectomy, canalicular surgery, etc.).
Adult Inclusion Conjunctivitis
Local therapy consists of 1 % tetracycline ointment, twice a day, for 1 month. Ofloxacin ophthalmic ointment has also proved effective in chlamydial conjunctivitis.97 Thrice daily use of 0.1 % dexamethasone eyedrops has a synergistic action with the antibiotic therapy.98
Topical antibiotic therapy alone is inadequate, because extraocular reservoirs of chlamydiae (genital, nasopharyngeal) are not sterilized and can lead to ocular reinfection on topical treatment withdrawal.99 Systemic therapy of adult inclusion conjunctivitis is classically based on oral doxycycline, 100 mg twice a day for 3 weeks. Erythromycin 500 mg, four times a day for 3 weeks is prescribed to pregnant women. Other oral medications include a single dose of 1 g of azithromycin, which is as effective but costly,100 and norfloxacin.101 It is of course necessary to treat all the sexual partners of infected patients. Safer sex is the best way of preventing dissemination, and of avoiding mother-child transmission.
Chlamydia should be tested for at least 3 weeks after treatment cessation, to identify patients who are still infected and require a further course of treatment.102 The ideal test is RNA detection with a molecular probe, because direct immuno-fluorescence can be negative after treatment.103
Neonatal Inclusion Conjunctivitis
Treatment of children born to mothers who carry chlamydiae is based on 1 % tetracycline or erythromycin ophthalmic ointment, twice a day for the first week of life. In case of documented conjunctivitis, oral erythromycin should be added at a dose of 50 mg/kg per day in four divided doses for 2 weeks. The parents must also be treated.
Other Conditions
The conjunctivitis of lymphogranuloma venereum, Reiter’s syndrome, and C.pneumoniae infection are treated in the same way as adult inclusion conjunctivitis. In contrast, conjunctivitis due to C. psittaci is not sensitive to erythromycin.
Chlamydial infection is highly prevalent and is an important cause of systemic and ocular morbidity. Ocular chlamydiosis must be diagnosed rapidly. Appropriate therapy will limit dissemination of the infection and avoid the sight-threatening complications of trachoma.
References
26. Mac Callan AF. Ophthalmoscope, 1908, 6: 856.
36. Diallo JS. Les lésions dégénératives du trachome. Bull Soc Panafr Ophtalmol, 1989; 1: 61-2.
38. Thygeson P. Historical review of oculogenital disease. Am J Ophthalmol, 1971; 71: 975-81.
53. Fransen L, Volker K. Neonatal ophthalmia in the developing world. Int Ophthalmol, 1988; 11: 189-96.
56. Saint-Blancat P, Risse JF. Les ophtalmies néo-natales. Bull Soc Oph-talmol Fr, 1995; 95: 367-71.
59. Catterall RD. Clinical aspects of Reiter’s disease. Br J Rheumatol, 1983; 22: 151-5.
60. Mark DB, Mc Culley JB. Reiter’s keratitis. Arch Ophthalmol, 1982; 100: 781-4.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree