Chapter 61 Care of the Eye in Facial Paralysis
Rehabilitation of a patient with facial paralysis depends on restoration of optimal lid position and function.1–3 This chapter summarizes techniques that I have found to be most helpful in achieving that goal, based on more than 5000 patients with facial paralysis on whom I have operated during the past 3 decades.
CRITERIA FOR SURGERY
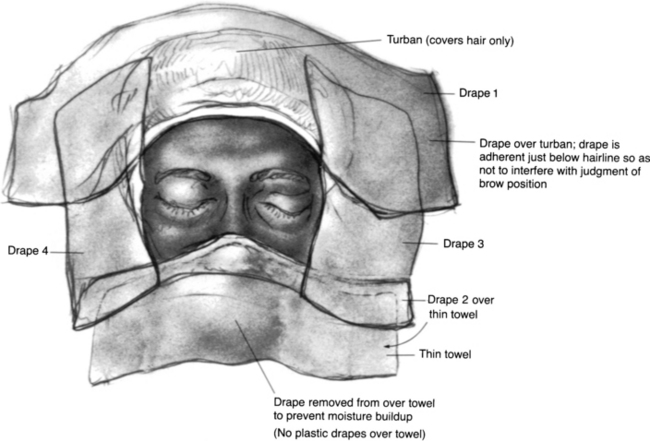
DRAPING
The hair is covered with a small drape formed into a turban and secured with a clamp. A second small sheet is incorporated with that drape to cover the superior end of the table. A body sheet is also placed. The eyelids and brow are isolated by means of two No. 1000 Steri-Drapes cut in half (Fig. 61-1). Each of the four drapes forms a border of the surgical field, which includes both eyes and the forehead area. Before the Steri-Drape is placed over the nose, a thin cloth towel is placed over the nose to avoid the suffocating feeling resulting from plastic over the nose. In addition, the plastic drape over the towel inferior to the adhesive area is excised to prevent moisture accumulation. Care is taken to avoid distorting the lower lid anatomy or brow areas by undue traction from the drapes.
GENERAL CONSIDERATIONS
Palpebral Spring Implantation
The palpebral spring4–14 is built preoperatively either in the office or at the bedside. Building the spring is time-consuming, and the surgeon and the patient should be comfortable during the procedure. Good light must be available, and if possible, the patient should be seated so that lid movement can be best evaluated.
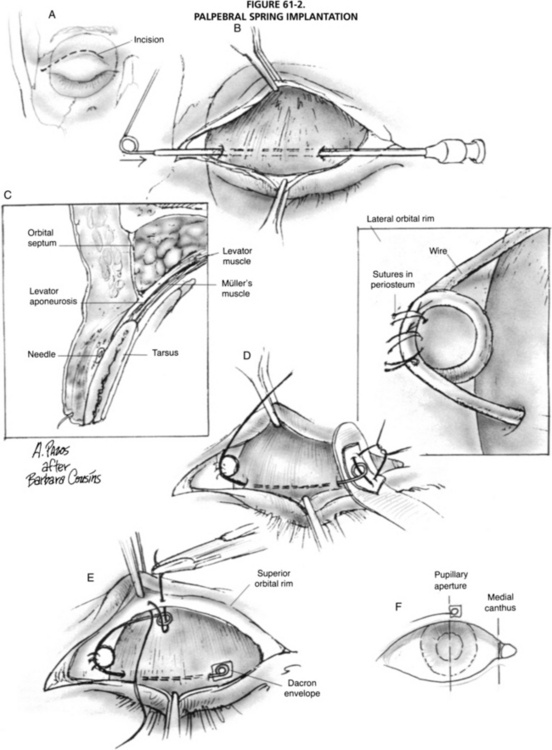
Surgical Technique
The eye is protected with a scleral shell. An incision is made along the lid fold at the junction of the medial one third and lateral two thirds of the palpebral aperture and is carried across the orbital rim (Fig. 61-2). Dissection is carried superolaterally, in the plane between the septum and orbicularis, to expose the orbital rim. Dissection is carried downward at the medial aspect of the incision to expose the tarsus.