Chapter 145 Brachytherapy for Choroidal Melanoma
Treatment of choroidal melanoma with brachytherapy – suturing a radiation source to the eye – was first reported by Moore in 1930.1 These early studies by Moore with radon seeds paved the way for the use of other forms of radiation at clinical centers around the world, including cobalt-60,2–5 ruthenium-106,6–8 gold-198,9 iodine-125,10–18 and palladium-103.19–21 Iodine-125 is currently the most commonly used isotope in brachytherapy for choroidal melanoma in the USA, whereas ruthenium-106 and palladium-103 continue to be popular at some centers. Brachytherapy offers an alternative to enucleation in the treatment of choroidal melanoma, allowing globe-salvaging with the possibility of maintaining useful vision. The Collaborative Ocular Melanoma Study (COMS) was a prospective, randomized study that provided clinicians with statistically sound evidence supporting the use of radiation in the treatment of choroidal melanoma. The study investigated more than 1300 patients with medium-sized melanoma and randomized to iodine-125 brachytherapy or enucleation.22 After 12 years of follow-up, there was no statistically significant difference between these two modalities of treatment with regard to mortality.22,23 Although treatment protocols and selection of tumors for plaque treatment must be individualized and differ among clinical centers, generally acceptable indications for plaque brachytherapy include: (1) selected small choroidal melanomas exhibiting growth or malignant transformation; (2) medium-sized choroidal and ciliary body melanomas in eyes with visual potential; (3) large melanomas with dimensions up to 16 mm in diameter and 8–10 mm in thickness; (4) larger melanomas, especially in monocular patients. However, despite success in sparing enucleation, radiation has profound effects on the surrounding retina and optic nerve, with vision limited by the resulting radiation retinopathy and optic neuropathy.24–28 These complications can have profound effects on quality of life with 209 patients from the COMS reporting no significant difference in visual function 3–5 years post-treatment for plaque brachytherapy versus enucleation.29 Continued research and investigation are needed to identify efficacious supplemental therapies for these universally common radiation-related complications.
Dosimetry
The optimal tumoricidal radiation dose for uveal melanoma remains unclear,30,31 but doses range between 50 and 100 Gy, with doses less than 50 Gy being associated with significant treatment failures.30 Kindy-Degnan et al.32 used helium ion radiation and reported on tumor apex dosages ranging between 50 and 80 Gy, showing that regardless of whether 50, 60, 70, or 80 Gy was used, there were no differences in tumor regression, survival, complications, or visual outcomes. Initially, the COMS decided to deliver 100 Gy to the tumor apex with a delivery rate of 50–125 cGy/h (tumors <5 mm in height are managed as if they were 5 mm thick).33 However, in 1996, based on newer dosimetric measurements and the recommendations of the American Association of Physicists in Medicine (AAPM), the COMS modified the prescription dose to deliver 85 Gy to the tumor apex with a delivery rate of 43–105 cGy/hour.34 Based on these modifications, with the AAPM-recommended calculation and revised prescription dose, the actual dose delivered to the tumor is the same. As a result, when analyzing studies prior to 1986 that utilized iodine-125, the actual dose to the tumor is 85% of the stated dose. Furthermore, the American Brachytherapy Society has presented the COMS dose recommendation as the guideline for the treatment of choroidal melanoma.35 As more accurate estimates for some of the assumptions used and better calculation algorithms have become available, dosimetry has been further refined and recalculated incorporating anisotropy, line source approximation, and Silastic and gold shield attenuation. Tables of dose to the tumor apex and various other ocular structures have been presented for the various size plaques.36 On average, the dose to the apex of the tumor appears to be 0.89 of the 85 Gy that has been assumed using the AAPM formalism.36 The physics of brachytherapy has been reviewed in several publications.36–38
Isotope selection
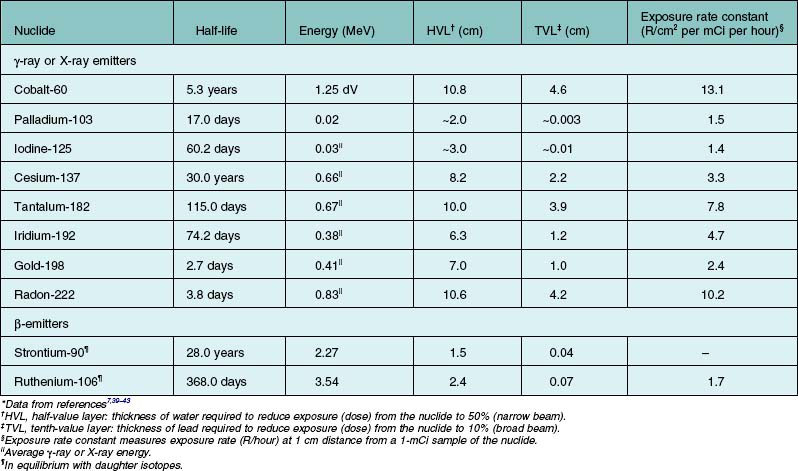
Brachytherapy is the application of radiation from isotopes over very short distances in contact with a surface. The radiation is distributed over a short distance from a surface or within the target tissue. Table 145.1 presents physical characteristics for the commonly used isotopes in brachytherapy. The table breaks isotopes into two broad categories: (1) those that emit γ-rays or X-rays; (2) those that emit β-particles (electrons). Table 145.1 footnotes explain some of the simplifications. The half-value (HVL) in water for a narrow beam is useful in comparing isotopes for the penetration of their radiations in tissue. The tenth-value layer (TVL) in lead for a broad beam is useful in evaluating penetration in shielding materials.
The energy of γ-rays or X-rays relates to their penetration in matter in a complex way. The more energetic rays penetrate to a greater extent and are more difficult to shield; these two factors are dealt with in the last two columns of Table 145.1.
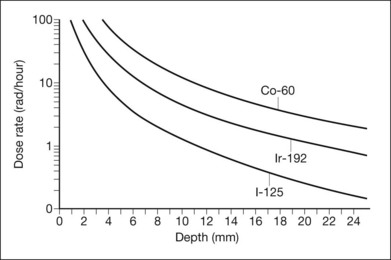
The HVL in water is an index of the extent to which the energy of the radiation is absorbed in water (or tissue). At short distances, important for application in localized tumors of the eye, the inverse-square law largely governs the radiation penetration in tissue. Figure 145.1 displays the depth–dose curves for iodine-125, iridium-192, and cobalt-60. Because of the small height (up to approximately 1 cm) of the tumors treated, this inverse-square law is far more important in determining scleral (or choroidal blood vessel) dose for a given dose to the tumor apex. The dose rate falls more rapidly near the source than further away. Thus, the scleral dose relative to the dose at the apex of the tumor may be reduced by simply introducing a space between the source and the sclera. In the orbit, only size constraints limit the magnitude of the space, with 1 mm being the maximum in plaques used for ocular brachytherapy. With greater distances and less energetic rays, tissue absorption begins to play a more important role. For the β-emitters, absorption in tissues, which is complex and related to the energy of the β-particle, must be measured.
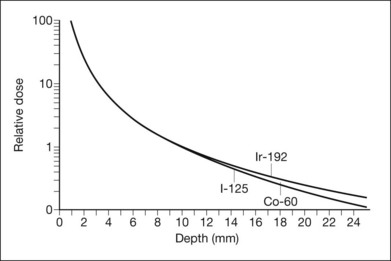
The exposure rate constant is an expression of dose rate at a standard distance from a specified amount of isotope. More atoms of an isotope with a low constant can achieve the same dose rate as one with a higher constant, the other characteristics being equal. The curves of dose rate versus depth in tissue for different isotopes can nearly be superimposed by adjusting the amount of each isotope in inverse ratio to the ratio of the exposure rate constants (Fig. 145.2).44
Beta-emitters, such as ruthenium-106, have been shown to be successful in tumor control for small to medium tumors, potentially up to 16 mm in diameter and up to 8 mm in thickness when used alone with calculated apex doses, or combined with transpupillary thermotherapy (TTT) when apex doses are insufficient.45 The presumed advantages of these lower-dose radiation sources are a decrease in the potential risk to adjacent structures as well as decrease the risk of radiation retinopathy.46 However, studies have not shown a reduction in treatment-related visual decline,45 as doses are thought to still be above those maximally tolerated by the retina, vasculature, and optic nerve.
Plaque design
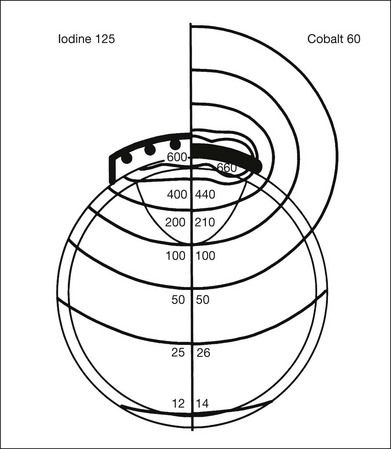
The iodine-125 plaque design used in the COMS evolved from that used by Rotman et al.47 and Robertson et al.,18 and consists of a gold plaque that is approximately 0.4 mm thick with a lip around its perimeter that resembles a smooth bottle cap (Fig. 145.3).44 The shielding device decreases lateral spread of radiation and results in a collimated beam of radiation. Plaques may be customized with notches or indentations of the gold rim to allow placement adjacent to the optic nerve sheath for juxtapapillary tumors. Notched plaques attempt to minimize the likelihood of plaque tilting secondary to placement next to the optic nerve sheath, as this tilt may result in excess radiation to the optic nerve, while decreasing the dose to the tumor apex. Other unique plaque designs and concepts include slotted plaques,48 which may aid in the treatment of juxtapapillary tumors, including circumpapillary tumors, which prove difficult to treat. Within the gold plaque is a soft, pliable plastic (Silastic) seed carrier insert with evenly spaced troughs that accept the iodine-125 seeds. The carrier is designed so that the seeds are adjacent to the gold. The thickness of the seed carrier separates the seeds from the sclera surface by 1 mm. The prepared loops facilitate anchoring of the plaque to the sclera with sutures. Eyelet placement proves important to minimize the potential for plaque tilt, with those with circumferential eyelets posing decreased likelihood of tilting. The relative dose distribution associated with a particular radioactive plaque is basically determined by the arrangement (distribution) of the seeds in the plaque. The dose distribution from seeds within a plaque, such as shown in Figure 145.3, is demonstrated by the schematic in Figure 145.4. By distributing iodine seeds over the area of the plaque and having a 1 mm spacer between the seeds and the sclera, the scleral dose delivered by an iodine-125 plaque is approximately the same as that delivered by a cobalt-60 plaque. Monte Carlo calculations by Chiu-Tsao et al.49 demonstrate a lower scleral dose for iodine-125 compared to cobalt-60, for a point source model.
Indications for treatment
Medium tumors
The Collaborative Ocular Melanoma Study (COMS), a prospective, randomized study funded by the National Eye Institute, compared survival in patients with medium-sized tumors randomized to brachytherapy or enucleation.33 The rationale for this study was outlined by Robertson in 1989.50 Results of the COMS medium-size tumor trial became available in 2001.22 Medium tumors were defined as tumors with a thickness between 2.5 and 10 mm, as well as a maximal basal diameter <16 mm. Stringent inclusion and exclusion criteria were used, including patient-related factors, such as a history of any prior cancer, comorbidities that may influence survival, and immunosuppressive therapy, as well as tumor characteristics such as juxtapapillary tumors (tumors within 1 mm of the optic nerve), diffuse (ring) melanomas, and melanomas with a primary ciliary body location. With 1317 patients enrolled and randomized between enucleation and iodine-125 brachytherapy in the medium-size COMS study, mortality rates were not statistically different up to 12 years after treatment. The trial had >80% power to conclude that neither treatment altered the mortality by as much as 25% from each other. The COMS study group refined survival rates to include 12-year data.23 Overall, cumulative all-cause mortality at 12 years for patients treated with either enucleation or plaque radiotherapy was 41% and 43%, respectively. For melanoma-specific mortality, or death confirmed histopathologically with melanoma metastasis, rates for iodine-125 were 10%, 18%, and 21% at 5, 10, and 12 years, respectively. For patients that received primary enucleation, melanoma-specific death rates were 11%, 17%, and 17%. These most recently updated statistics emphasize that even at longer follow-up, there were no statistically significant differences in survival between iodine-125 plaque brachytherapy and enucleation.
Long-term studies utilizing plaques other than iodine-125 have demonstrated success in the treatment of choroidal melanoma. For palladium-103, Finger et al.51 reported on 400 patients treated with plaque brachytherapy and a mean follow-up of 51 months. Metastatic rates were found to be 6%, with estimated 5- and 10-year risks of metastasis of 7.3% and 13.4%, respectively. For ruthenium-106 plaques, Verschueren et al.45 reported on 425 patients treated with plaque brachytherapy, with and without TTT, and a median follow-up of 50 months. Failure of local tumor control was 3.9%, with estimated metastasis rates of 24.5% and 30.9% at 5 and 10 years, respectively, and overall survival of 79.6% and 68.2%. Investigators utilizing ruthenium-106 plaques have shown that tumors >5 mm had increased risk of local recurrence.52 As a result, for tumors >5 mm or those tumors with insufficient doses to the tumor apex, adjuvant TTT is suggested;45,52 therefore, tumors up to 8 mm in thickness and 16 mm in diameter may potentially be treated with ruthenium-106.45
The extended COMS report that included 12-year mortality rates also assessed prognostic factors for metastasis and death, reporting a correlation with advanced age at baseline, as well as larger maximum basal tumor diameter. Shields et al.53 conducted an in-depth analysis of tumor size and risk for metastasis, reporting on the millimeter-by-millimeter risk for metastasis. In a series of 8033 patients with ciliochoroidal melanoma, tumor size was significantly associated with rates of metastasis. For small melanomas, rates of metastasis were 6%, 12%, and 20% at 5, 10, and 20 years, respectively. These rates were shown to increase based on tumor thickness, with large tumors metastasizing in 25%, 49%, and 67% of patients at 5, 10, and 20 years. Of note, advanced baseline age and tumor size were confirmed as risk factors for metastatic disease, as well as ciliary body location and clinical findings such as a brown tumor, subretinal fluid, and extraocular extension.
Small tumors
Curtin et al.54 reported on the observation of small choroidal melanomas in an era of enucleation as the gold standard. In a series of 46 patients observed over 14 years, melanoma-specific mortality was 6.5%, with no patients that were observed dying of melanoma-related causes. Other authors have reported on similar rates of melanoma-related mortalities for tumors that received either prompt treatment or delayed treatment.55,56 The COMS classified small melanomas as tumors with an apical height of 1–3 mm, and a maximal basal diameter between 5 and 16 mm.57,58 The COMS included 204 patients that did not fit the inclusion criteria for the medium-sized tumor trial. Upon study enrollment, 16 patients (8%) had treatment, while 67 patients (33%) required treatment at follow-up. Estimates of the need for treatment of small melanomas were 21%, 33%, and 38% at 2, 5, and 7 years, respectively. Overall, there were 27 deaths, with six melanoma-related. Five- and 8-year melanoma-specific mortality was 1% and 3.7%, respectively. Importantly, the study identified risk factors that were found to be predictive of tumor growth, including initial tumor thickness, the presence of orange pigment, the absence of drusen, and the absence of RPE changes surrounding the tumor (absence of halo). Other risk factors for the malignant transformation of small melanomas include subretinal fluid, patient symptoms, margins close to the optic nerve, and ultrasound hollowness.53,59
The COMS small tumor trial was not designed with mortality as a primary outcome, and initially was designed to be the framework for a larger, randomized trial to determine significant differences between observation, with deferred treatment upon documented growth compared with immediate treatment of small melanomas. Singh et al.60 reported on the proposed inclusion criteria for the aforementioned trial. Based on subgroup analysis from the COMS with identification of risk factors for tumor growth, the authors determined criteria to be: (1) apical height between 1 and 3 mm, and maximum basal diameter between 5 and 16 mm; (2) presence of any of three risk factors, including basal diameter >12 and <16 mm; tumor thickness between 2 and 3 mm, and the presence of orange pigment. To date, a randomized, controlled trial investigating these treatment strategies for small melanomas has not been undertaken. A more recent series by Sobrin et al.,61 reported on 154 patients with small choroidal melanomas who were observed for signs of malignant transformation (tumor growth or presence of orange pigment). A total of 45 patients (29%) who were observed needed treatment, with a mean interval to treatment of 4.1 years. All patients with observed transformation were treated with iodine-125 plaque brachytherapy utilizing intraoperative ultrasound for plaque localization. Of those treated, 4.5% developed metastasis, with only one death during the follow-up period. Additionally, one patient (2%) had local tumor recurrence necessitating enucleation. Notably, for those patients with small melanomas that continued to be observed for a mean of 8.1 years, no patient developed metastasis or died secondary to melanoma. Vision at baseline was 20/25, with final visual acuities of 20/30 for patients who were observed, and 20/50 at 2 years for patients that were treated with plaque brachytherapy. Radiation retinopathy and optic neuropathy were observed in 56% and 31% of patients, respectively.
Finally, transpupillary thermotherapy (TTT) has been proposed for the treatment of small choroidal melanomas that have a tumor height <4 mm. Numerous authors have reported on TTT in these lesions, with rates of tumor recurrence ranging from 8% to 56%, without standard inclusion criteria.39,62–69 A systematic review of the literature by Singh et al.70 reported a mean local tumor recurrence rate of 17% including 7% with extrascleral extension at a mean follow-up of 37 months. Although TTT may cause less visual morbidity in the treatment of small choroidal melanomas, the sole use of this therapy has the potential for high recurrence rates, which have been shown to be associated with an increased risk of metastasis.71 As a result, the sole use of TTT in the treatment of small choroidal melanomas should be carefully considered.
Large tumors
With the COMS establishing the widespread use of plaque brachytherapy for medium-sized choroidal melanoma, most eyes are salvaged, but not without severe visual morbidity secondary to the effects of radiation on the eye. The maximum tumor size that can be effectively treated with radiation without causing severe radiation complications is not known with certainty. Gragoudas72 suggested that eyes harboring tumors that involve up to 30% of the eye can usually be treated and salvaged after radiation. Char et al.73 reported information that suggested an upper size limit for tumors treated with radiation. Nearly 50% of the eyes with tumor thickness >10 mm eventually required enucleations after treatment with helium ions. Castro et al.74 noted that the enucleation rate for complications from helium ions increased as the tumor thickness increased beyond 6 mm. Munzenrider et al.75 reported that the enucleation rate following proton beam irradiation was significantly higher if the tumor thickness was >8 mm and/or if the tumor basal diameter was >16 mm. The COMS reported that enucleations were more common for tumors with greater thicknesses and greater base dimensions, although percentages were not given.71 If one adheres to the guidelines suggested by the COMS that radioactive plaques should extend 2 mm beyond the tumor margin, the maximum basal dimension of a tumor treatable with brachytherapy is approximately 21 mm, since for practical purposes it becomes technically difficult to place an episcleral plaque of more than 25 mm in diameter on the eye surface.
By COMS definition, large melanomas are tumors that are >10 mm in thickness, or >2 mm in thickness with basal diameter >16 mm. The COMS investigated the use of radiation pre-enucleation versus primary enucleation for large choroidal melanomas. At 10 years, survival rates did not show statistically significant differences, with melanoma-specific death rates of 40% for enucleation, whereas rates were 45% for patients that received radiation prior to enucleation.76 Although the COMS only looked at brachytherapy for medium-sized tumors, several studies have investigated the use of brachytherapy for large melanomas as an alternative to enucleation.77–79 Wilson et al. reported on 124 patients with large tumors of the ciliary body and choroid treated with iodine-125 brachytherapy and concluded that tumor thickness >8 mm in height or 16 mm in maximal basal diameter can be effectively treated with a favorable expectation of globe salvage, but limited vision conservation. Puusaari et al.78 came to a similar conclusion based on 96 eyes with large choroidal melanomas meeting one of three possible criteria: (1) largest basal diameter >16 mm provided that thickness was >2 mm; (2) height >10 mm regardless of basal diameter; (3) peripapillary tumor >8 mm in height and located <2 mm from the optic disc. The authors found that they had a fair chance of globe conservation with acceptable cosmesis, as well as a reasonable chance of conserving useful vision for 1–2 years. Shields et al.79 reported on 354 large choroidal melanomas (>8 mm in thickness) that were treated with plaque brachytherapy. Failure in local tumor control was estimated in 9% and 13% of tumors at 5 and 10 years, respectively. Metastasis of melanoma was estimated in 30% and 55% at 5 and 10 years, respectively. Notably, estimates of poor visual acuity (20/200 or worse) were 97% at 15 years.
Ruthenium-106 has also been used to treat large choroidal melanomas. Despite the finding that ruthenium-106 was a risk factor for local tumor recurrence,79 Kaiserman et al.80 reported on 63 large tumors treated with ruthenium-106. With a mean follow-up of 69.6 months and mean tumor thickness of 9.29 mm, 23.8% failed local tumor control. Estimated rates of metastasis were 22.5% and 48.1% at 5 and 10 years, respectively, while melanoma-specific mortality was found to be 20.5% and 46.2%. Interestingly, 70.8% of patients maintained vision better than 20/200. Other investigators suggest the use of adjuvant TTT in cases of tumors treated with ruthenium-106.81,82 Large melanomas present a unique situation, and were not included in the COMS for treatment with plaque brachytherapy. Investigators have shown that large tumors can be effectively treated with brachytherapy, but visual morbidity is high secondary to the large amounts of radiation to obtain effective tumor control.
Juxtapapillary tumors
Notched plaques are designed with an indentation in the plaque rim to allow flush placement adjacent to the optic nerve sheath. In addition, novel designs incorporating a slot in the plaque may allow for the successful treatment of juxtapapillary, and even circumpapillary tumors.48 In 1994, De Potter et al.83 reported on 127 patients with juxtapapillary melanomas treated with either enucleation or plaque brachytherapy. Despite being a non-randomized, retrospective study with a small percentage of patients treated with plaque brachytherapy (28%), the authors found that the treatment modality did not affect risk for metastasis. The same group also reported success using iodine-125 notched plaques in patients with juxtapapillary tumors overhanging the disc with tumor recurrence rates of 10%, a rate of metastasis of 13%, and 3% mortality.84 As expected for radiation treatment in close proximity to the optic nerve and fovea, 77% of patients had a visual acuity of 20/200 or less. Sagoo et al.85 also reported on the use of notched iodine-125 plaques in the treatment of circumpapillary tumors (tumors encircling the optic nerve). Recurrence rates were shown to be 14%, while the metastatic rate was 4% with no melanoma-specific deaths observed with a mean of 52 months follow-up. Preservation of visual acuity was poor, with greater than 60% manifesting with vision less than 20/200. Emphasizing the importance of notched plaques with placement confirmation by intraoperative ultrasound, Hui et al.86 reported on control rates of 100% at 30 months using notched plaques, compared to 89% at 25 months for non-notched plaques. Despite the promising results of notched plaque brachytherapy for juxtapapillary choroidal melanomas, studies with long-term follow-up are lacking. However, a recently published study87 reported on 650 juxtapapillary tumors treated with notched plaque brachytherapy with or without TTT with a mean follow-up of 52 months. Overall incidence of tumor recurrence was 11%, while metastasis was 10% with a melanoma-specific death rate of 3%. Kaplan–Meier estimates of tumor recurrence at 10 years were shown to be 21%, with metastasis and death of 24% and 9%, respectively.
In addition to the use of notched plaques with placement aided by intraoperative ultrasound, some have advocated the use of TTT as an adjunctive treatment for juxtapapillary tumors that have historically had higher rates of tumor recurrence. In the prior study by Sagoo et al.,87 TTT was utilized as an adjunctive treatment in 56% of eyes. Overall, tumor recurrences with TTT were 9% (compared to 14% for no TTT), metastasis was 9% (compared to 10%), with a death rate of 2% (compared to 5%). However, differences in recurrences and metastasis were not statistically significant when TTT was used as an adjuvant treatment in juxtapapillary tumors.
In conclusion, juxtapapillary tumors may be treated with plaque brachytherapy, with notched plaques and intraoperative ultrasound contributing to successful treatment. Proton beam irradiation (PBI) has also been shown to be efficacious in the treatment of peripapillary and parapapillary melanomas,88 as compared to notched plaques for juxtapapillary tumors.89 Additionally, TTT may be used as an adjunctive therapy with uncertain benefits. However, as a result of the close proximity to the macula and optic nerve, rates of visual compromise are high, with the majority of patients being legally blind.
Plaque placement technique
With advancements in ophthalmic photography, including wide-angle photography and digital software measurements, tumors are more often captured in toto as montage images. Tumor dimensions can then be determined by approximating the basal tumor diameter with regards to disc diameters or use of calipers, with the horizontal diameter of the optic nerve approximated at 1.5 mm. Wide-angle photography has been shown to be more accurate than ultrasound in measuring the basal diameter, as it potentially captures those margins or pigmentation that are not determined on ultrasound secondary to lack of elevation.90,91 Using this estimate, basal tumor diameter can be determined, with ultrasound (quantitative A-scan) aiding in the measurement of the tumor thickness and presence or absence of extraocular extension. For tumors that are unable to be captured completely by photographs, tumors can be measured using a technique first described by Hilton,92 where a grid is placed over the 20-D lens with each square representing 1 disc diameter. The tumor is viewed monocularly through the grid, allowing an approximate calculation of the basal diameter. The pre-surgical tumor estimates are important to pre-select plaque sizes to ensure that the plaque covers the entire tumor base along with 2 mm or more of tumor-free perimeter. For example, a tumor with a base diameter of 12 mm is treated with a 16 mm in diameter plaque.
The choice of anesthesia is left to the discretion of the surgeon. After an adequate peritomy, the surface of the sclera corresponding to the tumor is exposed. If extraocular extension is observed within a pseudoencapsulated focus ≤2 mm in diameter, the plaque is placed over the tumor base and the extension. Because an extraocular extension of <2 mm may not worsen the prognosis for survival,93 proceeding with brachytherapy as intended is reasonable. If extraocular extension is in excess of that noted, enucleation with tenonectomy must be considered. As an alternative, an iodine-125 plaque without a gold shield could be placed over the extension to allow radiation of orbital tissues adjacent to the visible extension. Ultrasound frequently detects extensions >2 mm,94 with extensions of this size occurring infrequently.93 As a result, discovery of large extraocular extensions (>2 mm) at surgery should rarely occur. For example, there have been virtually no such instances for globes enucleated in COMS.
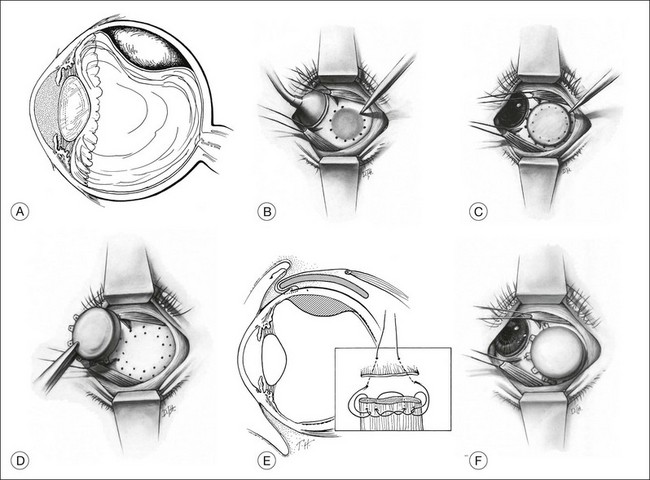
At surgery, the tumor base is localized with standard techniques used for retinal breaks or transillumination (or both). Sometimes the shadow of the tumor can be clearly outlined on the sclera while the globe is transilluminated through the cornea (Fig. 145.5A). The perimeter of the tumor base should be verified with indirect ophthalmoscopy. The MIRA diathermy-transillumination unit may assist in outlining the tumor base (MIRA 1 electrode handle with fiberoptic bundle and coaxial cable with scleral transilluminator). The intense light of the angled fiberoptic transilluminator allows the operator to visualize the tumor with indirect ophthalmoscopy while simultaneously visualizing the transsclerochoroidal retinal illumination from the fiberoptic light tip as it is moved to localize the perimeter of the tumor. Indirect ophthalmoscopy with scleral depression can also aid in identifying tumor margins. With the fiberoptic light at the perimeter of the tumor, a low-intensity diathermy mark can be made on the sclera. This mark can be made darker with a surgical marking pen (Fig. 145.5B). The tumor diameter can be measured and recorded using calipers, followed by estimation of 2 mm perimeter beyond the tumor borders. A transparent acrylic dummy plaque with a diameter equal to that of the therapeutic plaque is used to facilitate localization and later placement of the opaque therapeutic plaque. The dummy plaque is placed on the sclera, covering the scleral marks that identify the tumor perimeter. The dummy plaque must completely cover the base of the tumor as well as a tumor-free perimeter of 2 mm or more (Fig. 145.5C). After the perimeter of the dummy plaque has been marked on the sclera with pencil or diathermy, it is removed, and the opaque therapeutic plaque is placed within this ring of scleral marks and anchored with two or three intrascleral sutures (Fig. 145.5D,E). If the therapeutic plaque is the same size or smaller than the boundary of the tumor base as marked on the sclera, the procedure is terminated, and a larger plaque is prepared and placed on the eye later. If the plaque diameter is 3 mm or more greater than the diameter of the tumor base, it is sutured in place.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree