CHAPTER 67 Arytenoid Adduction
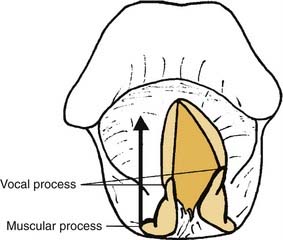
The arytenoid adduction procedure addresses laryngeal incompetence in patients with unilateral laryngeal paralysis.1 It mimics the action of the lateral cricoarytenoid muscle to close the glottis via rotation of the arytenoid cartilage rather than direct displacement of the membranous vocal fold.2 An adduction suture is placed in the muscular process of the arytenoid, which is the origin of the lateral cricoarytenoid muscle. This suture is passed forward through the paraglottic space and secured to the inferior thyroid ala (Fig. 67-1). This anterior traction pulls forward on the muscular process so that the arytenoid rotates. The vocal process, which is orthogonal to the muscular process, moves medially, dragging the membranous vocal fold with it. Arytenoid adduction can be performed in conjunction with type I thyroplasty. Research in animal models indicates that a combination of the two procedures is more effective than either alone.3
Arytenoid adduction is a more invasive procedure than type I thyroplasty and is technically more difficult. It has been reported to carry somewhat greater surgical risks, including airway obstruction, joint dislocation, fistula, and carotid injury.4,5 A 2001 study compared outcomes of type I thyroplasty alone or in combination with arytenoid adduction in 237 patients. The complication rate was 19% in patients undergoing arytenoid adduction versus 14% in those receiving thyroplasty alone. However, the difference in the complication rate was not statistically significant, and the 2 patients who required emergency tracheotomy for airway obstruction had thyroplasty alone.6 Arytenoid adduction does provide better closure of the posterior glottis, and research in animal models has objectively documented that acoustic and aerodynamic results for this procedure are better than for those of thyroplasty alone.7,8 Thus, arytenoid adduction is a valuable component of the therapeutic armamentarium for rehabilitation of patients with laryngeal paralysis, particularly those with significant glottal incompetence.
The clinical impact of laryngeal paralysis varies greatly.9 Some patients with unilateral paralysis are completely asymptomatic. At the other end of the spectrum, some patients are aphonic and have severe problems with aspiration during swallowing. Such severe symptoms result from laryngeal incompetence—the inability of the glottis to close completely. Two key factors that influence glottal closure in patients with laryngeal paralysis are the configuration of the paralyzed vocal fold and the compensatory function of the contralateral fold.
Several theories have been proposed to explain variations in symptoms and vocal fold positions in patients with laryngeal paralysis, ranging from selective damage to abductor fibers10 to adductor action of the cricothyroid muscle (Wagner-Grossman hypothesis).11,12 However, it has been demonstrated that the cricothyroid muscle does not exert an adductor force on the vocal fold.13–15 It is now generally accepted that a medial vocal fold position results from residual or regenerated innervation of laryngeal muscles.16–19 When there is significant innervation of adductor muscles, the paralyzed fold is located near the midline, and compensatory activity of the normal side of the larynx can often close the glottis during phonation. In such cases, aspiration is rare, and hoarseness or breathiness responds well to surgical medialization of the membranous vocal fold performed by injection or thyroplasty. On the other hand, complete flaccid paralysis results in a cadaveric position of the vocal fold with more severe glottal incompetence, often referred to as a posterior gap.
It has long been recognized that vocal fold injection, such as with polytetrafluoroethylene (Teflon), cannot restore glottal competence when there is a large glottal gap.20 There is some controversy regarding the efficacy of Isshiki type I thyroplasty in closing a posterior gap. It has been contended that a posterior extension of the thyroplasty implant can close a posterior gap, based on clinical observation.21 However, other clinical reports as well as experimental studies indicate that arytenoid adduction is much more effective than thyroplasty in closing the posterior glottis.7,8
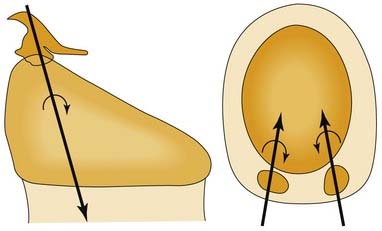
The concept of a “posterior gap” is not entirely accurate, in that the maximal glottic opening is between the vocal processes. The open glottis actually converges posterior to the vocal processes because lateral displacement of the vocal process involves external rotation of the arytenoid cartilage, not lateral displacement of the arytenoid.22,23 In other words, the angle between the membranous vocal fold and its posterior cartilaginous portion decreases as the vocal fold abducts (Fig. 67-2).24 Thus, the posterior portion of the cartilaginous vocal fold is medial to the vocal process in abduction, and it prevents glottic closure even with vigorous hyperadduction of the normal vocal fold (Fig. 67-3). Procedures that medialize the membranous vocal fold may achieve some medial displacement of the vocal process; however, the force vectors created by such procedures are inadequate to effect significant internal rotation of the arytenoid cartilage.
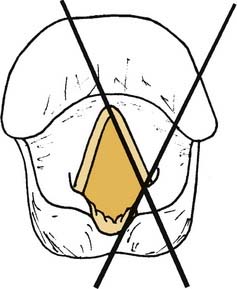
Figure 67-2. Vocal fold angle (X) formed by membranous and cartilaginous portions of the vocal fold.
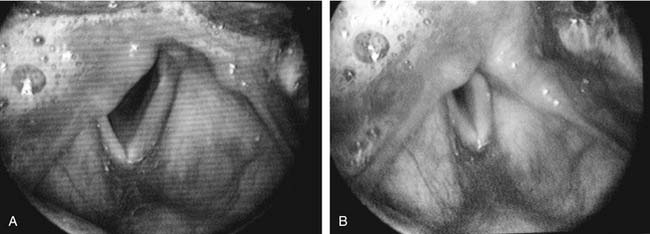
Figure 67-3. A, Apparent vocal fold shortening in laryngeal paralysis. B, Compensatory shortening of the mobile focal fold.
Vocal fold injection and type I thyroplasty do not address differences in the level of vocal folds. The paralyzed vocal fold often lies in a different plane from that of the mobile vocal fold. Although both folds are firmly attached to the anterior commissure, the vocal process may sag on the paralyzed side or lie above the glottic plane, as it does in physiologic abduction. Thus, there can be a significant vertical gap between the edges of the vocal folds, even when they appear to be touching when viewed from above in a two-dimensional image. The paralyzed fold can lie either above or below the glottal plane. In cadaver specimens from subjects who had chronic vocal fold paralysis, the vocal fold has been reported to be caudally displaced with a wide ventricle and shift of the conus elasticus to a horizontal plane.25,26 Other reports describe superior displacement of the paralyzed vocal fold, essentially the same position assumed by an actively abducted vocal fold.2,27
A difference in the level of the vocal folds can often be appreciated with indirect mirror laryngoscopy, which permits binocular vision. In 1932, noting observations with mirror laryngoscopy, New and Childrey28 stated, “In the absence of any innervation from the recurrent nerve fibers, the cord is somewhat relaxed or bowed; it is, therefore, shortened, somewhat narrowed and depressed, lying at a lower level than normal.” In a two-dimensional video image, a level difference is not apparent. What can be perceived is a difference in the apparent length of the vocal folds. Brewer and colleagues29 noted that a paralyzed vocal fold generally appears shorter than its mobile mate. In patients with significant glottal incompetence, the apparent length of a paralyzed vocal fold during inspiration is approximately two thirds that of the mobile side. During phonation, the mobile vocal fold appears to shorten to nearly the same length as its paralyzed mate (see Figure 67-3). Successful arytenoid adduction increases the apparent length of the paralyzed vocal fold.30
Three-dimensional motion analysis in cadaver larynges indicates that the arytenoid adduction procedure does not actually lengthen the vocal fold but instead moves the vocal process caudally. It is this vertical component of motion that is endoscopically perceived as a length change; the visual image shortens owing to rotation of the vocal fold out of the optical plane.31 In arytenoid adduction, the arytenoid rotates about an oblique helical axis. As the vocal process moves medially, it is displaced caudally as well (Fig. 67-4).32 Conversely, when the posterior cricoarytenoid muscle abducts the vocal fold, the vocal process moves laterally, rostrally, and caudally (Fig. 67-5).23 An abducted vocal fold appears shorter when viewed from above because the vocal process has moved rostrally; the vocal fold slopes upward, out of the plane of the image. In adduction and during arytenoid adduction, the vocal process moves caudally, toward the level of the anterior commissure, so that the vocal fold is parallel to the image plane, and the apparent length is longer.31
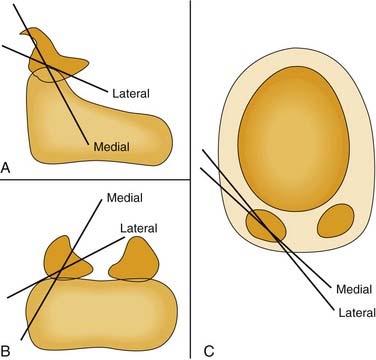
Figure 67-5. Axes of rotation (X) with simulated individual contraction of the two bellies of the posterior cricoarytenoid muscle in cadaver larynges. A, Sagittal view; B, posterior, coronal view; C, axial view. These data, as well as those from the study depicted in Figure 67-4, illustrate the multiaxial nature of the cricoarytenoid joint.
The cricoarytenoid joint is a shallow ball-and-socket, and therefore, it is multiaxial. That is to say, vocal folds do not open and close along a fixed “track,” and the rostrocaudal level of the vocal process is not completely dictated by internal and internal rotation. Cadaver studies of simulated muscle contraction demonstrate that the axis of rotation for the posterior cricoarytenoid is quite different from that for the lateral cricoarytenoid muscle (see Fig. 67-5).23
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree