OVERVIEW
The visual system takes a complex course in its path from the retina to the cortical visual processing areas, and the efferent control system has its own particular organization. These systems are subject to effects from vascular disease throughout their courses. Recognizing when a vascular lesion might underlie a visual complaint provides the ophthalmologist with an opportunity to pursue testing and to avert further damage.
After transduction and initial processing in the retina, neural signals exit the globe through axons of the retinal ganglion cells and travel to the optic chiasm through the optic nerve. In the chiasm, axons from the nasal retina decussate while axons from the temporal retina remain ipsilateral. Via the optic radiations, 90% of optic nerve axons then travel to the lateral geniculate nucleus of the thalamus where they synapse. Thalamic neurons then project via the optic radiations, which fan out through the temporal lobes with the axons carrying information from the superior visual field coursing most laterally. These axons synapse in layer IV of the primary visual cortex, whose neurons in turn project to higher cortical visual areas.
Similarly, the visual motor control pathways are subject to damage at multiple points. Three cranial nerves carry control information for the six extraocular muscles and lid muscles as well as the iris and ciliary body. The oculomotor nerve innervates the superior rectus, medial rectus, inferior rectus, and inferior oblique muscles as well as the levator palpebrae, superior tarsus, iris sphincter, and ciliary body. The bulk of its fibers arise from midbrain nuclei, and after exiting from the ventral midbrain, the nerve passes between the superior cerebellar and the posterior cerebral arteries. It exits the dura anterior and lateral to the posterior clinoid process. It runs along the lateral wall of the cavernous sinus in a relatively superior path. Sympathetic fibers running with the internal carotid artery then join it. It next divides into the inferior and superior branches that enter the orbit through the superior orbital fissure. The trochlear nerve innervates only the superior oblique muscle. Its nucleus lies in the rostral midbrain below the cerebral aqueduct. Unusual among the cranial nerves, the fibers decussate before the nerve emerges from the dorsal brainstem. It too passes between the superior cerebellar and the posterior cerebral arteries. It exits the dura beneath the tentorium cerebelli and travels through the lateral wall of the cavernous sinus, inferiorly to the oculomotor nerve, before entering the orbit through the superior orbital fissure. Finally, the abducens nerve innervates the lateral rectus. Its course is the longest of the three extraocular cranial nerves. Its nucleus is located in the pons at the floor of the fourth ventricle. Axons travel ventrally and caudally before exiting at the junction of the pons and medulla. It travels upward along the clivus and exits the dura via the Dorello canal before entering the cavernous sinus. Its path in the cavernous sinus is inferior and medial compared with the oculomotor and trochlear nerves. Then it also enters the orbit through the superior orbital fissure. Also of note, V1 and V2 run through the lateral wall of the cavernous sinus with V1 lateral to the abducens nerve and the maxillary nerve inferior to it.
Along these pathways, nerves are subject to compromise at multiple points via multiple mechanisms, including several notable vascular abnormalities. These pathways are intimately near the intracranial vessels. The ophthalmic artery runs with the optic nerve, usually inferolaterally, but rarely superiorly. The optic chiasm is surrounded by the circle of Willis with the anterior cerebral
artery coursing over the optic nerve, the bifurcation of the internal carotid just lateral to the chiasm and optic tract above the posterior communicating artery.
The efferent system is also closely apposed to multiple vessels. Before joining the nasociliary nerve (first division of the trigeminal nerve), the sympathetic fibers travel with the internal carotid artery. All the nerves controlling eye movements course through the cavernous sinus where they pass just lateral to the internal carotid artery with the abducens nerve abutting it in an inferior and lateral position. Before they enter the cavernous sinus, these nerves pass near multiple arteries in the circle of Willis. In particular, the oculomotor nerve is just lateral to the posterior communicating artery.
Vascular abnormalities can damage the visual system in multiple ways. Expansile lesions, such as aneurysms and arteriovenous malformations (AVMs), can directly compress nearby structures. Ischemia can cause damage anywhere along the visual system, whether large vessel strokes or microvascular damage affecting only a single cranial nerve. At times, these two possibilities can occur together. Vasospasm leading to ischemic stroke, even in vascular distributions distant from the primary bleed, is a major concern for comorbidity following subarachnoid hemorrhage. Elevated intracranial pressure, whether from blocking cerebrospinal fluid flow and reabsorption or from parenchymal swelling following brain injury, can compress cranial nerves with the abducens and oculomotor nerves as notable examples. It can lead to papilledema and to hemorrhage within the globe. Additionally, direct compression of the optic nerve can result in papilledema.
The ophthalmologist plays an important role in characterizing the patient’s deficits through history and examination, identifying potential vascular causes in the differential diagnosis and initiating proper evaluation. Identifying the deficits in the afferent visual pathway along with deficits in eye movements, pupillary abnormalities, and ptosis permits localization of the underlying lesion. While cerebrovascular disease can present in dramatic fashion, such as with major ischemic strokes or subarachnoid hemorrhages, aneurysms and other malformations can develop gradually with chiefly ophthalmic complaints. One classic example is an expanding posterior communicating artery aneurysm leading to oculomotor dysfunction typically involving the pupil. Recognition prompts vascular imaging, which can identify the aneurysm prior to rupture. In addition to formal catheter cerebral angiography, computed tomographic angiography (CTA) and magnetic resonance angiography (MRA) are increasingly utilized to evaluate possible vascular disease. MR angiography often can be combined into a single session with MRI. Identification of a cerebrovascular abnormality can permit treatment with the possibility of greater functional recovery and before more catastrophic damage takes place.
CRANIAL VASCULAR RADIOGRAPHY
Multiple modalities are available for assessing the cranial vessels. Digital subtraction angiography (DSA), also called conventional angiography or catheter angiography, remains the standard by which other modalities are judged. However, it carries small but significant risks related to its invasive nature, most notably the need for arterial access and the possibility of stroke and vascular damage, as well as risks from anesthesia. It also requires significant time of radiologists and supporting staff. MRA and CTA have increased in popularity. They avoid some of DSA’s drawbacks, but each modality has its own shortcomings. Additionally, duplex ultrasonography is a noninvasive modality with extremely small risk, but significant disadvantages in quality and applicability.
Computed Tomographic Angiography
CTA has a role in the detection of many cranial vascular abnormalities. Its sensitivity for aneurysm detection varies with the size of the aneurysm. One analysis found that sensitivity ranges from 2% for 2-mm aneurysms to 95% for 7-mm aneurysms.
1 A newer study using bone masking techniques found 99% sensitivity for aneurysms at least 3 mm, but only 38% for aneurysms less than 3 mm, and an even newer study, from China, found 91%, 94%, 98%, and 100% sensitivities for aneurysms in sizes less than 3 mm, 3 to 5 mm, 5 to 10 mm, and over 10 mm, respectively.
2,
3 In addition to screening, CTA can serve to confirm the absence of aneurysm. One study looking at CTA for subarachnoid hemorrhage that had been negative by DSA showed a 5.2% yield.
4CTA is useful for other vascular abnormalities. CTA appears to approach DSA for carotid-cavernous fistula (CCF) detection.
5 In the diagnosis of cervical artery dissection, one review found overall similar results for CTA and MRA.
6 For AVM detection, CTA sensitivity is 90%.
7CTA has its own drawbacks. CTA requires infusion of iodinated contrast, often in a volume of 1 L. This need limits its use in patients sensitive to iodinated contrast and in patients prone to volume overload, such as with chronic kidney disease and heart disease such as atrial fibrillation and congestive heart failure.
Magnetic Resonance Angiography
MRA allows for single-session imaging in combination with MRI. As an advantage over CTA, it does not use ionizing radiation. Most protocols are longer in time than CTA, but still only tens of minutes.
Its sensitivity in aneurysm detection is quite good under the right circumstances. Newer volume rendering MRA techniques offer greater than 95% accuracy, sensitivity, specificity, and negative and positive predictive values for aneurysm detection.
8,
9 Earlier data, however, indicate that 5 mm appeared to be a detection threshold.
10 Newer computer-aided techniques can offer up to 95% sensitivity with 91% sensitivity for aneurysms under 3 mm.
11MRA’s role in detection of other cranial vascular diseases is limited compared with CTA and DSA. MRA appears inferior to CTA and DSA for CCF detection.
5 MRA detection of cervical artery dissection, mentioned above, might be significantly better than reflected in older studies before the development of current techniques.
6 For AVM detection, MRI was 89% sensitive, whereas MRA was only 74% sensitive.
7
Ultrasonography
Duplex ultrasonography offers the attractive features of noninvasiveness, very low risk, speed, and lower cost. However, its overall usefulness is currently limited. It has been studied for dissection diagnosis. Its initial sensitivity for carotid dissections was only 74% in one study although follow-up scans showed a 91% sensitivity.
12 Another study, however, noted 100% sensitivity for carotid dissections and 94% sensitivity for vertebral dissections using flow techniques.
13 For aneurysm detection, transcranial ultrasonography in conjunction with CTA or MRA can improve results, but not significantly with the more difficult smaller aneurysms less than 5 mm.
14 Additionally, the interevaluator reliability of ultrasonography is a common concern. It can be useful for serial evaluation, but it does not appear as reliable as CTA or MRA for initial diagnosis.
ANEURYSMS
Epidemiology
Aneurysms within the circle of Willis account for perhaps some 80% to 90% of all aneurysms. The great majority present as sudden, nontraumatic subarachnoid hemorrhage, with high morbidity and mortality rates. Unruptured asymptomatic aneurysms are discovered in 5% of autopsied adults, and approximately 10% present with neurologic deficits related to mass effects, such as visual loss. The age- and gender-adjusted annual incidence rate is 9.0 per 100,000 (more frequent in women), and the incidence of rupture increases with age peaking in the two decades between 55 and 75 years. Risk of hemorrhage in unruptured aneurysms is 1% to 2% annually.
15 The annual incidence of subarachnoid hemorrhage from aneurysm is approximately 10 in 100,000, and multiple intracranial aneurysms are found in 20% to 30% of patients.
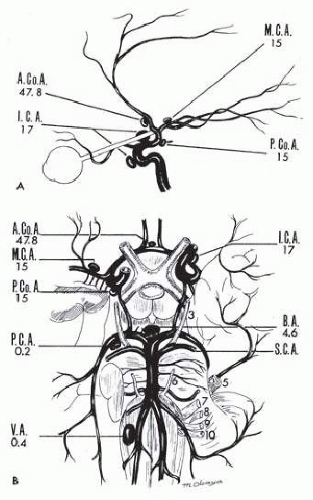
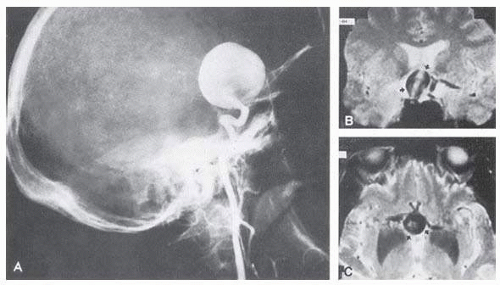
16Multiple saccular aneurysms of the carotid or vertebrobasilar system occur 20% to 30% of the time, frequently with identical or mirror sites found in the left-sided and right-sided circulations. Most aneurysms arise from the carotid system on the anterior communicating, middle cerebral, and internal carotid arteries, or they arise in the region of the origins of the posterior communicating arteries (
Fig. 17.1A). Only some 5% of saccular aneurysms arise on the vertebrobasilar system (
Fig. 17.1B).
Pathogenesis
The intracranial arteries have thin media and poorly developed or absent internal elastic lamina; they are particularly prone to developing small outpouchings at arterial branch junctions where developmental defects in the media exist. Histologic study of the saccular aneurysm often demonstrates a defect in the elastic and muscular coat, beginning at the point of origin (neck) from the parent artery. This finding has supported the concept of a developmental origin and created the term congenital aneurysm to designate saccular aneurysms, although these lesions are not present at birth.
Factors such as hypertension, degenerative changes in the arterial wall, and heritable connective tissue disorders as in the Ehlers-Danlos syndrome and neurofibromatosis-1, all play roles in the subsequent development of aneurysms. There is firm evidence of increased incidence of aneurysm in first- or second-degree relatives of patients who harbor aneurysms, and there is a distinct association with polycystic kidney disease and aortic coarctation.
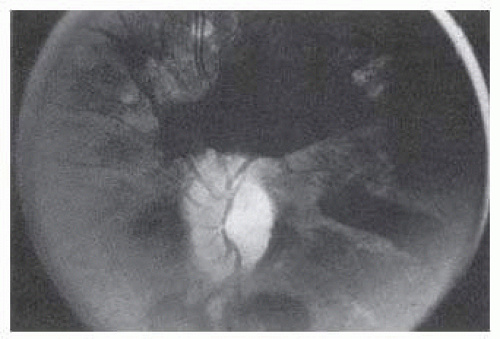
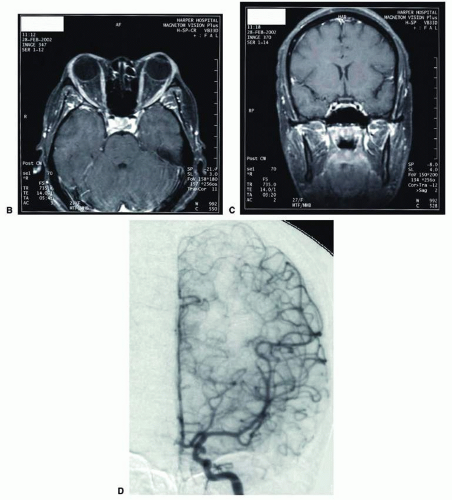
16The intraocular hemorrhage of Terson syndrome is thought to result from transmission of intracranial pressure through the subarachnoid communication between the optic nerve sheath and the intracranial cavity, with subsequent nerve sheath dilation and rupture of dural and bridging vessels (
Fig. 17.2). Intraocular hemorrhage is possibly the result of retinal venous hypertension brought on by the obstruction of both the central retinal vein and the retinochoroidal anastomoses. Kuhn et al.
17 have reviewed Terson syndrome, including the role of pars plana vitrectomy; these authors noted the high incidence of preceding coma, and the efficacy of surgical intervention in visual recovery.
Presentation
Clinical symptoms usually result from the rupture of an aneurysm with extravasation of blood under arterial pressure into the subarachnoid or intraventricular spaces or into the brain parenchyma with intracerebral hematoma formation. Subarachnoid and intraventricular blood causes depression of consciousness; intracerebral hematoma and vascular spasm produce focal neurologic signs and even cerebral herniation with compression of the third nerve. The subsequent sudden increase in the intracranial pressure may result in sixth-nerve palsies, in subretinal, intraretinal, or preretinal hemorrhage, and in conjunctival and, rarely, orbital hemorrhage.
Aneurysms, either saccular or fusiform, also cause neurologic deficits by progressive enlargement rather than by rupture—for example, visual loss caused by compression of the optic nerve from fusiform distortion of the supraclinoid carotid or ophthalmic artery, or saccular enlargement of the intracavernous carotid artery that produces chronic ocular motor palsies. The symptoms in patients with aneurysmal compression of the anterior visual pathway may include visual loss that can be acute, gradual, or fluctuating.
Management
In general, neurosurgical clipping and endovascular coiling are the two major options available for the treatment of aneurysms. A ruptured aneurysm leading to subarachnoid hemorrhage is a medical emergency requiring immediate intervention. Neurosurgeons and neurointerventional radiologists typically quickly decide on the safest intervention on a case-by-case basis.
The best timing and approach for unruptured aneurysms remain open questions. Some unruptured aneuryms pose relatively low risk when left untreated. In particular, smaller aneurysms and anterior circulation aneurysms have lower rupture rates.
18 The risks of intervention might outweigh the risks of monitoring in more cases than previously thought.
19 Many experts disagree with this approach, however.
20 In older individuals and others in whom the chance of significant morbidity is large, a conservative approach with serial examination and imaging may be prudent.
Saccular Aneurysms
Intracavernous Carotid
Epidemiology
Intracavernous carotid aneurysms constitute only 2% to 3% of all intracranial aneurysms and are unique because of their location.
Presentation
Owing to their location and proximity to multiple cranial nerves, these aneurysms produce a specific constellation of ocular and neurologic signs and symptoms. Rupture of such aneurysms, which are almost always saccular, may possibly result in carotid-cavernous sinus fistula, but subarachnoid hemorrhage is rare.
22 However, slowly progressive enlargement is the rule, usually occurring within the cavernous sinus, with compression of the third, fourth, and sixth cranial nerves and later involving the first and second divisions of the fifth nerve (see
Chapter 12).
23 Progressive enlargement of the aneurysm forms a mass in the floor of the middle cranial fossa, compromising motor as well as sensory functions of the trigeminal nerve. Anterior expansion of the aneurysm erodes the anterior clinoid, optic foramen, and superior orbital fissure, eventually producing unilateral visual loss and exophthalmos. Posterior expansion, which occurs later, can erode the petrous portion of the temporal bone, causing ipsilateral facial palsy and, rarely, deafness. The sphenoidal sinus and the nasopharynx may infrequently be involved by inferior expansion, and medial extension erodes into the sella and may simulate a pituitary tumor
24 or cause bilateral ophthalmoplegia.
25 Bilateral saccular intracavernous aneurysms occur uncommonly.
26The onset of signs and symptoms is usually insidious, at times accompanied by pain about the eye and frontal area on the involved side. The pattern of serial involvement of the cranial nerves within the cavernous sinus is usually as follows: VI, III, V, and IV. Occasionally, palsies evolve simultaneously and the ipsilateral optic nerve may eventually be encroached on by superior expansion of the aneurysm. The pupil is often not dilated maximally, as in the usual acute third-nerve palsy; it may be relatively small (rarely immobile) because of the simultaneous involvement of the oculosympathetic fibers.
23 Indeed, the combination of ipsilateral sixth-nerve palsy and ipsilateral Horner syndrome is a classic presentation for a cavernous aneurysm, given the anatomic relationships between the sixth nerve, ocular sympathetics, and the cavernous carotid artery. Barr and associates
21 believed that such aneurysms usually arise as a weakness in the lateral wall of the carotid artery within the cavernous sinus and that the aneurysm tends to expand laterally between the third and fourth nerves superiorly and the sixth nerve inferiorly, finally compressing the nerves on the medial wall of the aneurysmal sac rather than laterally. Late involvement of the fifth nerve is emphasized by the findings that, in the three studied cases, this nerve was not splayed over the lateral aspect of the aneurysm, but that it lay mainly inferior, lateral, and posterior in the region where late expansion of the aneurysm occurs. Although periocular pain has often been emphasized as a prominent symptom, it may not occur until ophthalmoplegia has been present for years.
Management
The management of these aneurysms differs significantly from that of other saccular aneurysms. Because of the location and configuration within the cavernous sinus, direct surgical approaches to cavernous carotid aneurysms are hazardous. In recent years, intravascular occlusion of the internal carotid by detachable balloon has evolved as a safe and successful procedure, often with relief of pain and improvement in ophthalmoplegia.
27 In many cases, symptomatic treatment of the double vision and/or ptosis (e.g., prisms, strabismus surgery, ptosis repair) and careful monitoring is the preferred management strategy.
Carotid-Ophthalmic Artery
Epidemiology
They are rare in reported series: Pool and Potts
28 cited only two examples in 157 cases, and there was a 5.4% incidence in 2,672 patients with single aneurysm in the Cooperative Study of Intracranial Aneurysms and Subarachnoid Hemorrhage.
29 Ferguson and Drake
30 reported 32 such aneurysms; Guidetti and LaTorre
31 reported 16 cases. A high incidence of concurrent cerebral aneurysms has been reported: 67% in one series
31 and 37.5% in another.
32
Presentation
These aneurysms may present with vision loss. There is a striking correlation between aneurysmal projection and visual impairment. With superior-medial projection, optic nerve compression with monocular visual loss is often present. Eight of 16 patients reported by Guidetti and
LaTorre
31 had prominent visual symptoms with reduced vision and optic atrophy. Larger aneurysms may involve both optic nerve and chiasm. However, Ferguson and Drake
30 reported 32 patients with preoperative visual deficits. While involvement of the anterior visual pathway is the most frequent neuroopthalmologic presentation, paralysis of the third cranial nerve was reported in a single case. Although deemed a rare event,
30 visual loss occurs in approximately one-third of patients with carotid-ophthalmic aneurysms.
32 Aneurysms in this location may traverse the adjacent optic nerve or chiasm by actually splitting it, the mechanism of which is still unknown. Presentation with visual disturbance is again variable.
33
Supraclinoid Carotid Artery
Epidemiology
Of 3,123 giant (larger than 25 mm) intracranial aneurysms in one series,
34 93 involved the internal carotid above the cavernous sinus, thus qualifying as supraclinoid. Sixty-five were carotid-ophthalmic, 16 were at the bifurcation of the middle cerebral artery, and 12 were carotid-posterior communicating-anterior choroidal in location. Bilateral carotid-ophthalmic aneurysms were found in 19 cases, with a female predominance and average age of 48 years. The visual system was compressed in all but 6 cases, and 14 aneurysms presented as subarachnoid bleeding. Most of these giant aneurysms occur in women in the fifth and sixth decades of life. These effects are primarily the result of compression of the optic nerves and chiasm.
34 For the most part, involvement of the visual system represents the only neurologic complication.
Presentation
These aneurysms rarely rupture. Most commonly, they present as insidious visual loss, or they are uncovered during angiography for other, sister aneurysms.
35 The pattern of visual field loss with supraclinoid aneurysm and its temporal profile tend to differ from that occurring with primary intrasellar or parasellar tumors. Vision is usually affected in a single eye, commonly with nasal field depression, and at times progressing to blindness before the second eye is involved.
36 These aneurysms arise below the optic nerve, which is stretched and flattened before subsequent involvement of the chiasm and the opposite nerve.
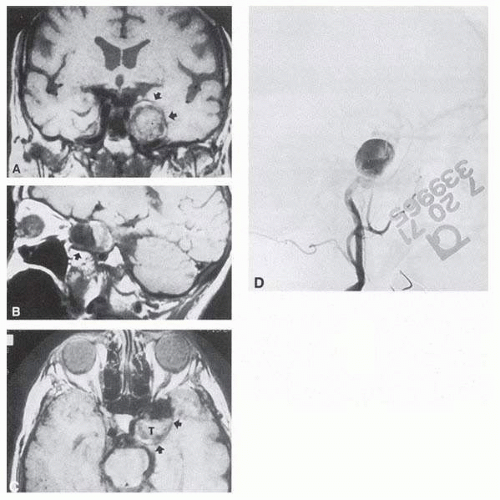
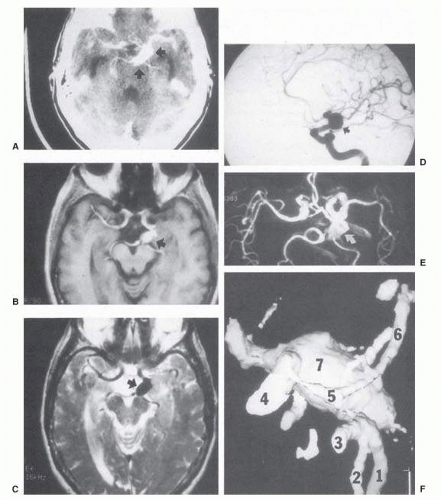
Most such aneurysms expand upward and forward, becoming located primarily anteriorly (
Fig. 17.4). The optic nerves rise upward from the optic canal and may be inclined at a 45° angle such that the chiasm is more superiorly, as well as posteriorly, placed. It may be expected that uniocular ipsilateral visual loss would occur and
progress before the contralateral field is involved because of chiasmal compression and before opposite nerve damage ensues. Although rapid visual loss has been reported, a longer duration (even years) is the rule. Rarely, the aneurysm may be more posteriorly placed or the chiasm more anteriorly fixed, resulting in initial involvement of the optic tract.
37Large aneurysms also arise from or involve the origins of the middle or anterior cerebral arteries, and they may precisely mimic a slowly growing suprasellar neoplasm. Similarly, large aneurysms of the supraclinoid carotid can simulate a pituitary tumor,
24 including prolactinemia via the compression of the pituitary stalk.
38 Aneurysms may mimic other masses, and this underscores the need for MRI or arteriography in the evaluation of some sellar or parasellar syndromes.
Ophthalmic Artery
Presentation
The symptoms are quite similar to the symptoms of supraclinoid aneurysms, consisting of monocular progressive visual loss due to vascular compression from beneath the optic nerve. The pattern of visual loss begins as a unilateral scotoma usually involving fixation and then depression of the nasal and upper field, progressing to blindness. Further expansion involves the lateral aspect of the chiasm, causing temporal field loss in the opposite eye. Rarely, such aneurysms extend to involve the more distal aspects of the ophthalmic artery, producing enlargement of the optic foramen and even erosion into the orbit.
36,
39 Jain
40 reported an unusual presentation of a true saccular aneurysm of the ophthalmic artery with projection into the optic foramen in a patient with monocular papilledema. Again, the intimate relationship of ophthalmic artery origin from the internal carotid and the size of the aneurysm may blur distinctions among ophthalmic, carotid-ophthalmic, and supraclinoid.
Intraorbital ophthalmic artery aneurysm was the clinical diagnosis given to the first cases of CCF described by Travers
41 in 1809. All such previous cases before modern angiography must be suspect, with the majority probably being misdiagnosed CCFs or arteriovenous communications involving the orbital circulation. However, cases proved arteriographically do exist. Rubinstein and associates
42 reported the case of a 36-year-old man who experienced monocular burning and lacrimation with progressive loss of vision fluctuating over weeks; angiography demonstrated a 7-mm aneurysm arising intraorbitally, 12 mm distal to the origin of the ophthalmic artery. Rarely, direct penetrating trauma may produce aneurysmal dilation of the intraorbital ophthalmic artery.
43
Posterior Communicating Artery
Presentation
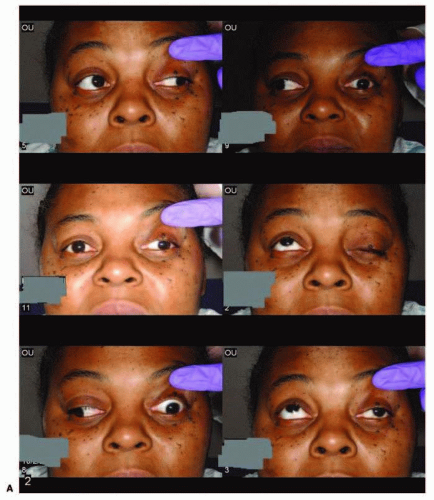
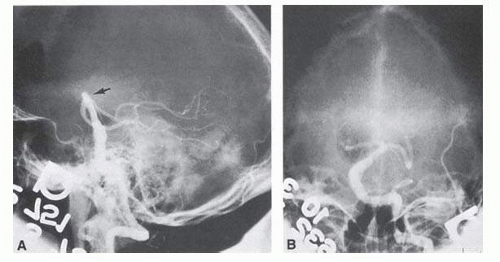
These aneurysms are of special interest to neurologists, neurosurgeons, and ophthalmologists because they tend to involve the oculomotor nerve, often in a neurologically isolated fashion. The classic presentation is sudden onset of severe unilateral frontal headache, ptosis, limitation adduction, depression and elevation of the eye, and dilated and fixed pupil. The cerebrospinal fluid is grossly bloody, and angiography is diagnostic (
Figs. 17.5 and
17.6). Pain in and around the eye in the trigeminal-ophthalmic distribution is a conspicuous symptom, but its presence is not sufficient to differentiate an aneurysmal third-nerve palsy from a microvascular etiology. Sensory defects are absent as only the oculomotor nerve is compromised. Clinical and pathologic evidence indicates that impairment of function by a contiguous aneurysm usually occurs in conjunction with hemorrhage into the oculomotor nerve that, along with sudden distortion, can produce referred pain.
44Oculomotor palsy caused by posterior communicating artery aneurysm typically shows maximal involvement of all third-nerve functions (
Fig. 17.5A). Although an individual extraocular muscle may be partially paretic, it is quite uncommon for any single extraocular muscle to be entirely spared (lateral rectus and superior oblique excluded), and it is exceedingly rare for only a single extraocular muscle (including the iris sphincter) to be involved. Relative pupillary sparing and pupillary involvement is of considerable importance in differential diagnosis. Loss of pupillary function is extremely concerning for aneurysmal compression. The common situation is total pupillary paralysis with ruptured or unruptured posterior communicating aneurysms that involve the third nerve, but important exceptions exist. Of course, in the clinical setting of sudden onset of a painful third-nerve palsy, with severe headache and nuchal rigidity, angiography is indicated whether or not the pupil is involved.
In approximately one-half of patients with ruptured posterior communicating artery aneurysms, third-nerve
palsy develops either immediately or within a day. Aneurysms can cause ipsilateral frontal headache and thirdnerve palsy by compression before they actually rupture. Approximately 70% of symptomatic but unruptured aneurysms show a third-nerve palsy, and by far the most common location is at the origin of the posterior communicating artery.
29 The incidence of oculomotor palsy with posterior communicating artery aneurysms varies from 34% to 56%.
45After third-nerve palsy, especially when caused by aneurysm or trauma, if recovery does not begin within a few weeks, the phenomenon of misdirection usually occurs (see
Chapter 12). Aberrant regeneration can result in oculomotor synkinesis, a phenomenon seen with compressive cranial nerve III lesions, but extremely rare with ischemic lesions. Ductions referable to cranial nerve III can become coupled to one another, to miosis, to eyelid retraction, or to a combination.
46 Presentation of new synkinesis referable to the third nerve merits evaluation for aneurysm or alternate compressive lesion. Hepler and Cantu
47 assessed the ultimate ocular status in 25 patients with third-nerve palsies secondary to aneurysms and
found that all patients had some residual abnormality of third-nerve function, but it was usually of trivial importance to the patient. Only 5 of 25 patients in this series complained of significant difficulty with diplopia, and 1 patient had a persistent, complete third-nerve palsy. In another study of patients treated by a direct surgical approach to the posterior communicating artery aneurysm within 10 days of symptomatic onset, a better prognosis existed for the recovery of third-nerve function than in those operated on after a longer interval.
45,
48
Middle Cerebral Artery
Presentation
Aneurysms in the distribution of the middle cerebral artery are common and have a relatively good prognosis even after rupture. They usually do not give rise to neuroophthalmologic symptomatology until they hemorrhage. Thereafter, blood may dissect into brain parenchyma, producing intracerebral hematomas with resultant contralateral paralysis, sensory loss, and homonymous visual field defect. Rarely, an isolated visual field defect may be the only focal neurologic sign of a bleeding aneurysm located distally on a posterior branch of the middle cerebral artery, with the hematoma having dissected into the visual
radiations. Ipsilateral hemicranial, hemifacial, or periorbital pain may herald minor leakage preceding frank subarachnoid hemorrhage.
49
Anterior Communicating Artery
Epidemiology
They are the most common location for an intracranial aneurysm, constituting roughly 20% to 30% of all intracranial aneurysms.
50,
51
Presentation
Anterior communicating artery aneurysms rarely produce focal neurologic signs prior to rupture despite being situated just above the optic nerves. Chan et al.
52 reported six cases collected over 37 years that caused monocular blindness by rupture of downward pointing aneurysmal sacs. With rupture, bleeding occurs into the optic nerve with symptoms of severe headache and monocular blindness.
Vertebrobasilar System
Epidemiology
Between 5% and 15% of all intracranial aneurysms are located in the posterior fossa, but these are often not clinically suspected until rupture. The majority of such aneurysms are at or about the bifurcation of the basilar artery.
Saccular basilar aneurysms tend to present at a younger age (<60 years) and are most common in middleaged women, whereas fusiform ectasia is associated with arteriosclerosis in hypertensive men in the sixth and seventh decades. In one study,
53 the majority of patients with saccular aneurysms died of rupture, as opposed to those with fusiform basilar artery aneurysms, in whom death tended to occur from myocardial infarction.
Presentation
The bifurcation of the basilar artery approaches the brainstem exit of the oculomotor nerves, but it is rare that thirdnerve palsy occurs prior to aneurysm rupture. Only those aneurysms found just distal to the basilar bifurcation on the proximal posterior cerebral arteries are likely to compromise the oculomotor nerve. When such aneurysms enlarge, they can exert pressure beneath the third ventricle and chiasm simulating the signs of a parasellar tumor, or the aneurysm may invaginate the third ventricle and thus mimic a colloid cyst.
54 Saccular vertebrobasilar aneurysms usually present with subarachnoid hemorrhage, without concurrent or premonitory focal neurologic signs and symptoms. Among the 28 patients reported by Höök et al.,
55 only 8 patients had prerupture symptoms (headache) and 4 had prerupture signs. However, prodromal signs that falsely suggest either vertebrobasilar insufficiency or a posterior fossa mass lesion have been amply documented. McKinna
56 reviewed eye signs in a series of 611 posterior fossa aneurysms and found diplopia, major field defects, retinal or vitreous hemorrhage, or papilledema present in 50%. The double vision (present in 35%) was caused by cranial nerve palsy, skew deviation, defective upward gaze, and bilateral external ophthalmoplegia.
In a series of 50 patients with basilar artery aneurysm, Nijensohn and associates
53 found 27 patients with saccular aneurysms and 23 with fusiform basilar dilations. In the former group, symptoms such as episodic diplopia, transient hemiplegia, and paresthesia mimicked the signs and symptoms of vertebrobasilar vascular disease. Various brainstem signs, such as progressive quadriparesis, nystagmus, and multiple cranial nerve involvement, occur with such aneurysms even before rupture. Isolated oculomotor paralysis has been reported with both saccular and fusiform aneurysms of the basilar system.
57 Posterior fossa aneurysms can thus mimic mass lesions, with progressive cranial nerve palsies and hydrocephalus.
58
Management
Management is difficult secondary to the tight space and the proximity to multiple brain structures. Treatment of such aneurysms presents a formidable technical problem well described elsewhere.
59
Posterior Cerebral Artery
Epidemiology
Aneurysms of the posterior cerebral artery are rare lesions. Their incidence in the Cooperative Study of Intracranial Aneurysms and Subarachnoid Hemorrhage was 0.8%.
29
Presentation
Although such aneurysms arise in vessels supplying the major portions of the visual radiations and cortex, Pool and Potts
28 remarked that they knew of no instance in which visual symptoms occurred before the rupture of the
aneurysms. Drake and Amacher
60 reported their experience in eight patients, only one of whom had a temporary homonymous field defect after hemorrhage. Rarely, such aneurysms arise from the first portion of the posterior cerebral artery near the junction of the posterior communicating artery; more commonly, they occur at the first major branching of the posterior cerebral artery as it courses around the midbrain. In the former location, ruptured aneurysms are associated with third-nerve palsy and contralateral hemiparesis. These signs might be anticipated because the proximal segment of the posterior cerebral artery is closely related to the cerebral peduncle and third nerve at its emergence between the posterior cerebral artery and the superior cerebellar artery.
Childhood Aneurysms
Epidemiology
Intracranial aneurysms uncommonly become symptomatic in children, in whom hemorrhage is less frequent and mass effect is more likely. Patel and Richardson
61 found 58 patients younger than 19 years (1.9%) among 3,000 cases of ruptured intracranial aneurysms. Of 2,951 patients with cerebral aneurysm in the Cooperative Study of Intracranial Aneurysms and Subarachnoid Hemorrhage summarized by Locksley,
29 only 41 patients showed evidence of aneurysmal rupture by the age of 19. Because of their rarity in pediatric patients, aneurysms are infrequently suspected in children with signs of intracranial hemorrhage or mass lesions. Yet early diagnosis and treatment of aneurysms in children, as in adults, can be lifesaving.
Although there is no doubt that intracranial aneurysm is the most frequent source of subarachnoid hemorrhage in adults, it is a long-established maxim that AVM more commonly leads to subarachnoid hemorrhage in children than does aneurysm. Yet when large series of patients up to 20 years of age with subarachnoid hemorrhage are considered, aneurysm is a more common etiology than AVM. In the 124 young patients with subarachnoid hemorrhage reported by Sedzimir and Robinson,
62 for example, 50 patients had aneurysms and 33 had AVMs. These authors also summarized 321 patients through 20 years of age, including their own patients and those from three other series, and found 36% with aneurysm and 27% with AVM. Thus, if patients up to age 20 are included, intracranial aneurysms cause subarachnoid bleeding more frequently than do vascular malformations. AVMs predominate if only preadolescent patients with subarachnoid hemorrhage are considered because symptomatic aneurysms are rare in younger groups. There appears to be a biphasic presentation of intracranial aneurysms of the first two decades, with the lesions most often becoming symptomatic after age 10 or before the age of 2 years.
63 Aneurysms in children rarely become symptomatic between 2 and 10 years of age.
Pathogenesis
Most intracranial arterial aneurysms seen in children are saccular, and they may be associated with heritable connective tissue disorders, including autosomal dominant polycystic kidney disease, Ehlers-Danlos syndrome type IV, neurofibromatosis-1, and Marfan syndrome.
16 Amacher and Drake
64 noted that pediatric aneurysms may reach giant size, may be fusiform in configuration, especially in the vertebrobasilar system, and may be causally related to bacterial endocarditis or other infections. Such mycotic aneurysms are the result of arterial damage from a septic embolus.
65 Neurofibromatosis-1 is associated with proliferation of Schwann cells within arteries, with secondary degenerative changes; in this disorder, there is a predilection for arterial occlusions or aneurysms of the cervical carotid and anterior communicating arteries.
66 Fusiform aneurysms of the basilar or carotid arteries, although a common sequel of atheromatous degeneration of the intracranial arteries in adult patients, are rare in children and may be associated with neurofibromatosis-1
61 or have another pathologic basis.
Presentation
Intracranial aneurysms in children are more common than has previously been recognized owing to a greater awareness, widespread use of noninvasive CT and MRA,
67 and the relative safety of catheter angiography.
68 There are clinical tendencies in children with intracranial aneurysms that differ from those in adults: (1) multiple aneurysms are less common in children; (2) associated congenital anomalies, especially coarctation of the aorta and polycystic kidneys, are more commonly seen in children with symptomatic aneurysms; (3) the mortality from initial hemorrhage in children admitted to hospital is less than in adults; and (4) children tend to recover more quickly and completely from neurologic defects. The usual presentation is intracranial hemorrhage, but ophthalmoplegia, diabetes insipidus, and other signs mimicking tumor have rarely been reported with aneurysms.
65
Traumatic Aneurysms
Presentation
Traumatic aneurysms of the intracavernous segment of the internal carotid artery come to attention because of recurrent, often massive, epistaxis, with variable involvement of the ocular motor nerves.
69 Postsurgical aneurysms are documented after sinus surgery, transsphenodial pituitary resection, and yttrium-90 implantation.
70 Despite the large number of transsphenoidal procedures, this complication appears unusual. Paullus and coworkers
71 have reported an extraordinary case of progressive bilateral ophthalmoplegia caused by false aneurysm complicated by a CCF component. It is to be recalled that, according to microdissections of Rhoton and associates,
72 the carotid arteries may approach the midline within the sella to as close as 4 mm, and that adherence to a strictly midline approach seems advisable.
Aneurysms of the extracranial carotid system are distinctly uncommon and may follow trauma or are associated with atherosclerosis or fibromuscular dysplasia.
73 Neuroophthalmologic signs are rare, including headache or ipsilateral oculosympathetic palsy. Penetrating orbital trauma with false aneurysm of the ophthalmic artery has been noted.
43
Fusiform Aneurysms
Pathogenesis
These aneurysms are usually associated with but not necessarily caused by advanced atheromatous degeneration, which explains the term atherosclerotic ectasia.
Presentation
The neurologic complications of such dilatations, which can involve either the carotid or vertebrobasilar system, are most often secondary to direct pressure effects rather than to rupture and subarachnoid hemorrhage.
Carotid System
Pathogenesis
As previously noted, fusiform aneurysms have been described even in young children and have been associated with connective tissue diseases and neurofibromatosis.
16,
64,
66,
74,
75 Thus, congenital causes must be suspect in youth, as well as in the situation of spontaneous arterial dissections.
Presentation
A dilated and tortuous carotid may flatten the optic nerve against the falciform dural fold above the opening of the optic canal. Such compression rarely may be responsible for instances of slowly progressive visual loss with eventual optic atrophy, some instances of which may be mistakenly diagnosed as normal-tension glaucoma.
Hilton and Hoyt
76 reported a case of bitemporal hemianopia associated with fusiform dilation of the internal carotid and anterior cerebral arteries. The latter actually prolapsed between the optic nerves. The patient’s slowly progressive bitemporal hemianopia and optic atrophy, with normal sella, was not believed to be the result of compression by the dilated vessels, but was considered more likely the result of impaired circulation caused by traction on, and obstructions of, the small vessels supplying the anterior aspect of the chiasm. Colapinto et al.
77 have also described optic nerve compression by fusiform ectasia of internal carotid artery demonstrated by MRI and cerebral angiography (see
Chapter 5, Part II).
Vertebrobasilar System
Epidemiology
Tortuous or redundant basilar arteries are not uncommon in the older age group. As opposed to saccular basilar aneurysms, fusiform aneurysms tend to occur in the older age group (older than 60 years) and are found predominantly in men.
16,
53
Pathogenesis
They are commonly associated with hypertension and atherosclerotic cardiovascular disease, and a notable association with abdominal aortic aneurysms also exists.
Presentation
Occasionally, gross dilation or ectasia develops so that the basilar artery acts as a mass in the posterior fossa. This phenomenon produces signs of low-pressure hydrocephalus,
cranial nerve palsies, and long tract and sensory signs and may even simulate a cerebellopontine angle tumor or tumor at the foramen magnum.
78The association of insidious multiple cranial nerve palsies and long tract signs referable to a brainstem level, in an elderly patient with evidence of atherosclerosis, should make fusiform basilar artery dilation a diagnostic consideration.