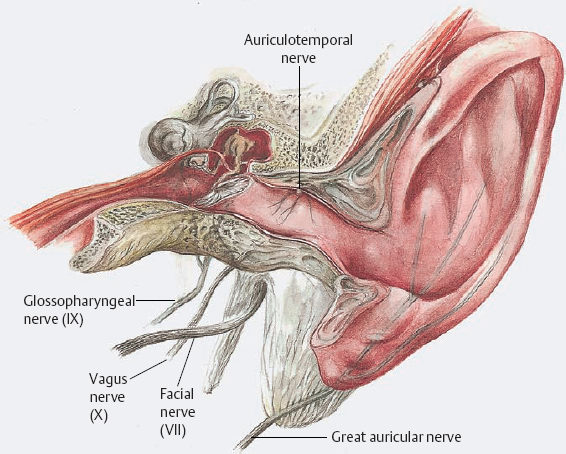
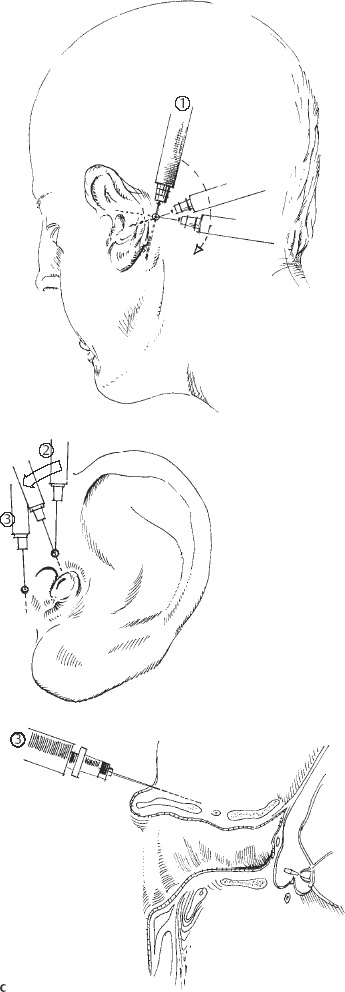
3 Anesthesia and Monitoring Modern anesthesiology has enabled otosurgeons to carry out prolonged operations in patients of all ages. It has thus not only made an immense contribution to the advances in ear and skull base surgery that have been achieved, but has also helped obliterate the dubious reputation of painful and hasty ear “butchery” from which otosurgery suffered for many decades. In addition to providing complete analgesia, anesthesia ensures undisturbed homeostasis of vital functions during and after surgery, making possible the fundamental qualities of precision and sophisticated reconstruction that the specialty of otosurgery today requires. Middle ear operations can generally be carried out with the patient receiving local anesthesia, and many ear surgeons use this method. At my department, all stapes surgery for otosclerosis is performed under local anesthesia, but general anesthesia is preferred for tympanomeatoplastic procedures. On the one hand, patients prefer it, and on the other the surgeon can also work more comfortably, with easier management of bone work and soft-tissue dissections. The following nerves provide the sensorineural supply for the external and middle ear: Fig. 3.1 Sensorineural supply to the external and middle ear. These nerves are visible as such during surgery only in the sulcus behind the squamotympanic suture at the roof of the external auditory canal (1), over the promontory (3), and below the auricle (5). However, the sensory periphery of the nerves spreads over the meatal walls and the middle ear spaces as a network, and they are therefore susceptible to infiltration anesthesia. Figure 3.1 shows the topography of these nerves around the external auditory canal (EAC). Complete analgesia is provided by infiltration of about 8–10 ml of a 1% lidocaine solution, with the addition of 1 : 200 000 epinephrine (=5μg/ml), into three subregions (Fig. 3.2). The first injection infiltrates the mastoid cortex to its tip, and continues anteriorly to the meatal entrance and superiorly to the temporalis muscle. This lifts the skin in the trago-helical incisure. The second injection enters this region, advances to the bone in the squamotympanic suture, and continues medially along the meatal roof over about 1 cm. Another injection may be brought into the floor of the EAC, starting in the terminal notch of the auricle. This technique is satisfactory for painless dissection of the soft tissues and for standard bone resections, including stapedectomy or cochlear fenestration. If I anticipate that more extensive bone resection may be needed at the anterosuperior meatal wall, I add a pretragal injection at a depth of 1–2 cm, with the risk of temporary (1–2 h) postoperative facial weakness. If some pain occurs—e.g., with sharp dissection of the fibrous annulus or around the chorda tympani—some drops of the lidocaine solution can be rinsed over this area, but it should be immediately removed from the oval and round niches. Although local anesthesia works very well in primary ear operations, diffusion of the anesthetic agent is obstructed by fibrous scars, so that local anesthesia is less satisfactory in revision cases or in highly inflamed ears. Local anesthesia is much supported by premedication with benzodiazepines, for instance 20 mg dipotassium-chlorazepat (tranxilium). During critical phases of surgery the patient’s comfort can be enhanced by repeated boli of 1 mg of midazolam (dormicum) for anxiolysis. H. Mang, J. Schüttler General anesthesia is generally preferred for all types of surgery of the ear and temporal bone, with the exception of stapes surgery in otosclerosis and not for minor interventions. Since hemorrhage is definitely reduced by local anesthesia, and tends to be exacerbated by general anesthesia, local infiltration of lidocaine with added epinephrine is also carried out immediately after tracheal intubation. Controlled mechanical ventilation is obligatory. The combination of anesthetic gas inhalation with intravenous application of narcotics and relaxants has changed in recent years. At present, intravenous administration with automatic dosage, but without anesthetic gas inhalation, is preferred. The principles of application in adults and children are detailed below. The preoperative preparation of the child scheduled for ear surgery is in accordance with the general rules of pediatric anesthesia. No laboratory tests in otherwise healthy children are required. A chart review, physical examination, and informing the parents about the approach to anesthesia are mandatory. We use Emla cream (Astra, Inc., Westboro, Massachusetts, USA) to reduce the pain associated with the percutaneous insertion of an intravenous cannula. Premedication is given to the child in the parents’ presence by either the anesthetist or a nurse anesthetist, in a quiet room adjacent to the recovery room. The premedication route depends on whether an intravenous line can be established outside the operating room. With an intravenous line in place, we administer midazolam in 1mg increments. Without intravenous access, we administer midazolam 0.5–0.8 mg/kg body weight (b.w.) rectally. In all cases, we wait until the child can be readily separated from the parents. Standard monitoring consists of pulse oximetry, temperature, electrocardiography, and automated noninvasive blood pressure measurement, and is established before the induction of anesthesia. Inhaled anesthetics: if it is not possible to place an intravenous line before the patient enters the operating room, we use an oxygen/nitrous oxide mixture (1 : 1) and sevoflurane, administered via a pediatric anesthesia circuit. As soon as adequate depth of anesthesia is achieved, peripheral intravenous access is established. Intravenous anesthetics:
 Local Anesthesia
Local Anesthesia
 General Anesthesia
General Anesthesia
Infants and Children
![]()
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


