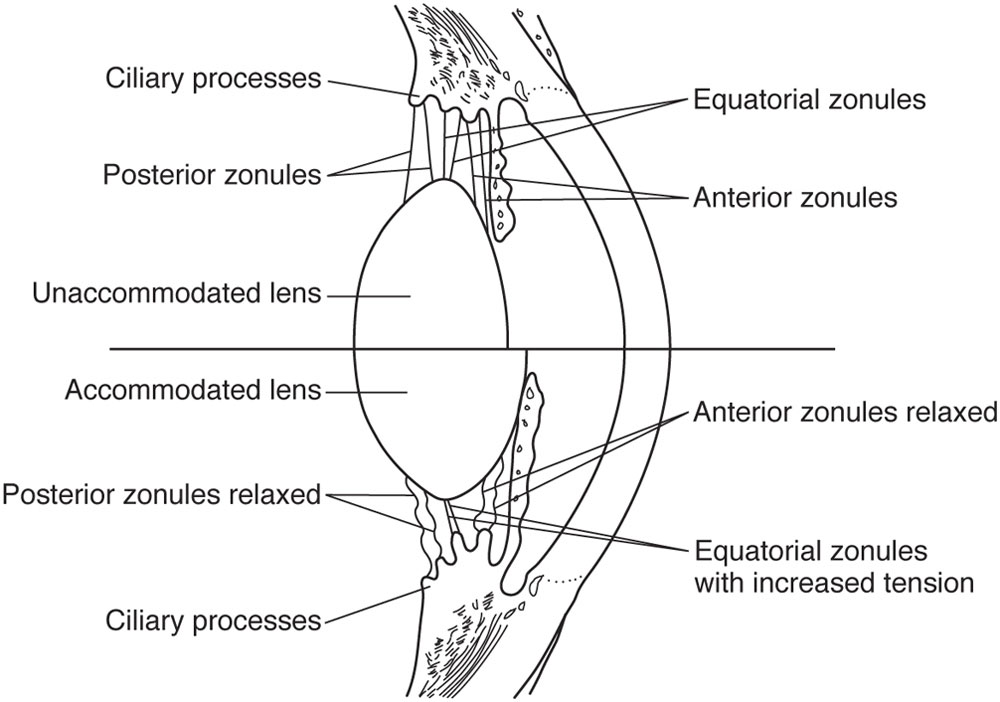
Figure 9-1 Schematic representation of the Helmholtz theory of accommodation, in which contraction of the ciliary muscle during accommodation (bottom) leads to relaxation of the zonular fibers. The reduced zonular tension allows the elastic capsule of the lens to contract, causing an increase in the anterior and posterior lens curvature. (Illustration by Jeanne Koelling.)
In the Helmholtz theory, the equatorial edge of the lens moves away from the sclera during accommodation and toward the sclera when accommodation ends. In this theory, all zonular fibers are relaxed during accommodation and all are under tension when the accommodative effort ends. According to Helmholtz, presbyopia results from the loss of lens elasticity with age. When the zonules are relaxed, the older lens does not change its shape to the same degree as the young lens does; therefore, presbyopia is an aging process that can be reversed only by changing the elasticity of the lens or its capsule.
Diametrically opposed to the Helmholtz hypothesis is the Schachar theory of accommodation. Schachar suggests that during accommodation, ciliary muscle contraction leads to a selective increase in equatorial zonular tension—rather than to the uniform decrease (anterior, equatorial, and posterior) proposed by the Helmholtz theory—with a subsequent pulling of the equatorial lens outward toward the sclera (Fig 9-2). Schachar postulates that accommodation occurs through the direct effect of zonular tension (as opposed to the passive effect proposed by Helmholtz), causing an increase in lens curvature. In this theory, the loss of accommodation with age is a result of the continued growth of the lens, leading to increasing lens diameter and a decrease in the lens–ciliary body distance, which results in a loss of zonular tension. Anything that increases resting zonular tension (eg, scleral expansion) should restore accommodation.
Schachar proposed that the mechanism for functional lens shape change is equatorial stretching by the zonules, which would decrease the peripheral lens volume and increase the central volume, thus producing central steepening of the anterior central lens capsule (Fig 9-3). During accommodation and ciliary muscle contraction, tension on the equatorial zonular fibers increases, whereas tension on the anterior and posterior zonules is reduced. These actions would allow the lens to maintain a stable position at all times, even as it undergoes changes in shape. Schachar theorized that the anterior and posterior zonules serve as passive support structures for the lens, whereas the equatorial zonules are the active components in determining the optical power of the lens.
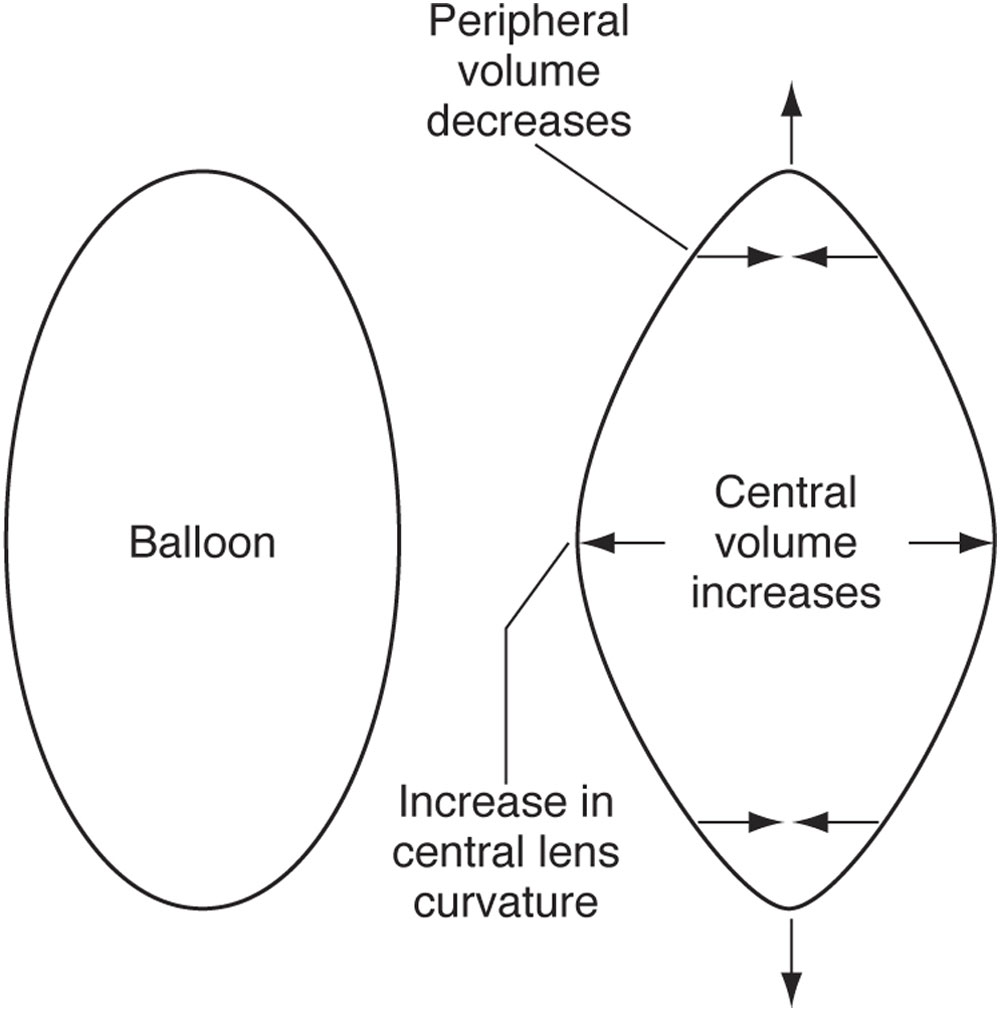
Figure 9-3 The Schachar theory proposes that the increase in equatorial zonular tension causes a decrease in peripheral lens volume and, thus, an increase in central lens volume and central lens curvature. (Illustration by Jeanne Koelling.)
Evidence from recent studies on human and nonhuman primates contest Schachar’s theories on accommodation and presbyopia. Investigations in human tissues and with scanning electron microscopy reveal no zonular insertions (equatorial or otherwise) at the iris root or anterior ciliary muscle. Various imaging techniques consistently indicate that the diameter of the crystalline lens decreases with accommodation so that the equator moves away from the ciliary body. In vitro laser scanning imaging shows that the crystalline lens does not change focal length when increasing and decreasing radial stretching forces are applied. This evidence thus runs contrary to Schachar’s proposal that the lens remains pliable with age and that presbyopia is due solely to lens growth and crowding that prevents optimum ciliary muscle action.
Glasser A, Kaufman PL. The mechanism of accommodation in primates. Ophthalmology. 1999; 106(5):863–872.
Schachar RA. Cause and treatment of presbyopia with a method for increasing the amplitude of accommodation. Ann Ophthalmol. 1992;24(12):445–447, 452.
Strenk SA, Strenk LM, Koretz JF. The mechanism of presbyopia. Prog Retin Eye Res. 2005; 24(3):379–393. Epub 2004 Dec 19.
Nonaccommodative Treatment of Presbyopia
Monovision
Currently in the United States, monovision is the technique used most frequently for modifying presbyopia in individuals with phakic eyes. In this approach, the refractive power of 1 eye is adjusted to improve near vision. Monovision may be achieved with contact lenses, laser in situ keratomileusis (LASIK), surface ablation, conductive keratoplasty, or even lens surgery. The process involves intentionally undercorrecting a patient with myopia, overcorrecting a patient with hyperopia, or inducing mild myopia in an individual with emmetropic vision. Historically, the term monovision typically referred to the use of a distance contact lens in 1 eye and a near contact lens in the other. A power difference between the 2 eyes of 1.25–2.50 D was targeted on the basis of near acuity demands. Currently, many refractive surgeons target mild myopia (–0.50 to –1.50 D) for the near-vision eye in the presbyopic and prepresbyopic population. The term modified, or mini-, monovision is more appropriate for this lower level of myopia for the near-vision eye. Mini-monovision is associated with only a mild decrease in distance vision, retention of good stereopsis, and a significant increase in the intermediate zone of functional vision. The intermediate zone is where many visual functions used for activities of daily life occur (eg, looking at a computer screen, store shelves, or a car dashboard). For many patients, this compromise is an attractive alternative to constantly reaching for reading glasses. Selected patients who want better near vision may prefer higher amounts of monovision correction (–1.50 to –2.50 D) despite the accompanying decrease in distance vision and stereopsis. Future directions in monovision may involve modification of corneal asphericity to improve depth of focus.
Patient selection
Appropriate patient selection and education are fundamental to the overall success of monovision treatment. Although monovision can be demonstrated with trial lenses in the examination room, a contact lens trial period at home is often more useful. Patients whose vision is neither presbyopic nor approaching presbyopia are typically not good candidates for monovision, as they are usually seeking optimal bilateral distance acuity. However, patients in their mid- to late 30s should be counseled about impending presbyopia and the option of monovision.
The best candidates for monovision are patients with myopia who are over the age of 40 years and who, because of their current refractive error, retain some useful uncorrected near vision. These patients have always experienced adequate near vision simply by removing their glasses and therefore understand the importance of near vision. Patients who do not have useful uncorrected near vision (myopia worse than –4.50 D, high astigmatism, hyperopia, or contact lens wearers) may be more accepting of the need for reading glasses after refractive surgery. For some patients, refractive surgeons routinely aim for mild myopia (–0.50 to –0.75 D, occasionally up to –1.50 D) in the nondominant eye. It is prudent to give the patient a trial with contact lenses to ascertain patient acceptance and the exact degree of near vision desired. Patients should understand that loss of accommodation is progressive, so that monovision may not remain fully effective over time, and corrective glasses may eventually be required.
Reinstein DZ, Carp GI, Archer TJ, Gobbe M. LASIK for presbyopia correction in emmetropic patients using aspheric ablation profiles and a micro-monovision protocol with the Carl Zeiss Meditec MEL 80 and VisuMax. J Refract Surg. 2012;28(8):531–541.
Rocha KM, Vabre L, Chateau N, Krueger RR. Expanding depth of focus by modifying higher-order aberrations induced by an adaptive optics visual simulator. J Cataract Refract Surg. 2009;35:1885–1892.
Conductive Keratoplasty
As discussed in Chapter 7, conductive keratoplasty (CK) is a nonablative, collagen-shrinking procedure approved for the correction of low levels of hyperopia (+0.75 to +3.25 D). The procedure is approved by the US Food and Drug Administration (FDA) for the treatment of presbyopia in individuals with hyperopic or emmetropic vision.
Multifocal IOL Implants
The IOL options for patients undergoing cataract surgery have increased in recent years. Patients may select a traditional monofocal IOL with a refractive target of emmetropia, mild myopia, or monovision; or they may opt for a multifocal or an accommodating IOL for greater range of focus.
The first multifocal IOL to be granted FDA approval in the United States has since been replaced by other lens designs originally including zonal refractive and apodized diffractive IOLs. The zonal refractive lens design utilizes refractive power changes from the center of the lens to the periphery to provide distance and near correction. In contrast, diffractive lens designs employ a series of concentric rings to form a diffraction grating (see BCSC Section 3, Clinical Optics) to create 2 separate focal points for distance and near vision (Fig 9-4). Some diffractive lenses are apodized, meaning that the diffractive step heights are gradually tapered to allow a more even distribution of light, which theoretically makes for a smoother transition among images from distance, intermediate, and near targets. Currently there are no zonal refractive IOLs available in the United States. Zonal refractive lenses, however, are available in a variety of styles in Europe. Examples of this type of lens include the Rayner M-flex T (Rayner Intraocular Lenses Ltd, East Sussex, United Kingdom) and the Lentis Mplus intraocular lens (Oculentis GmbH, Berlin, Germany) (Fig 9-5). In addition, IOLs with trifocal optics are available in Europe; examples are the FineVision (PhysIOL, Liège, Belgium) and the AT Lisa tri (Carl Zeiss Meditec, Jena, Germany).