Voice Therapy for the Treatment of Voice Disorders
Jackie Gartner-Schmidt
The otolaryngologist and speech-language pathologist are critical members of the voice care team (1). The role of each, however, is different. Patients enter the medical setting with the medical intervention model in mind; namely, is there a medicine or surgery that will fix their voice problem? Whereas otolaryngologists take responsibility for effecting change either medically or surgically, a speech-language pathologist teaches patients to adopt responsibility for behavioral change because, in its most basic sense, voice therapy teaches patients to modify faulty or compensatory vocal behavior. Persuading patients to become responsible for their vocal behaviors may be difficult, but it is paramount to successful voice therapy (2,3,4). Otolaryngologists are the first people to impress this message to their patients: voice therapy is often successful but requires active participation from the patient. Unfortunately, there are high rates of attrition in voice therapy (5,6,7). It is important for otolaryngologists to refrain from saying “I want you to try voice therapy” as often this verbiage can plant the seeds of noncompliance and attrition. In addition, because most patients assume the medical model of rehabilitation, a rapid restoration (i.e., “quick fix”) of voice is expected. Behavioral modification is not a “quick fix” and patients need to understand this basic premise.
A common question posed by otolaryngologists to speech-language pathologists is, “What do you do in voice therapy?” In this chapter, a model of the component parts of voice therapy will first be illustrated followed by a condensed description of some of the most commonly used voice therapies and their applications to specific voice disorders. In addition, approximate treatment durations, reference to appropriate referrals, and limitations to therapeutic success will be discussed.
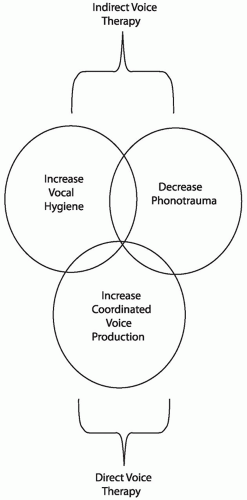
The Venn diagram in Figure 71.1 illustrates the key categories of any voice therapy program: increase vocal hygiene, decrease phonotrauma, and increase coordinated voice production. Although the circles delineate separate entities, they are not mutually exclusive. This model is very similar to the component parts (i.e., categories) of voice therapy. The speech-language pathologist determines which category (i.e., circle) to work with the patient, so modification of the appropriate maladaptive behaviors can be emphasized. The speech-language pathologist must also realize that patients may be in more than one circle. The first two circles, increase vocal hygiene and decrease phonotrauma, represent indirect approaches to voice therapy, whereby the speech-language pathologist essentially educates the patient concerning how his or her laryngeal mechanism works and what may cause harm. The third circle, increase coordinated vocal production, represents a direct approach to voice therapy; here, the speech-language pathologist directly alters the patient’s speaking technique in an attempt to increase vocal quality and efficiency. Indirect voice therapy usually requires 1 to 2 weekly sessions, whereas direct voice therapy usually requires 4 to 6 sessions (e.g., weekly sessions are ideal but not mandatory). This therapy schedule mirrors preoperative and postoperative therapy, in that patients generally receive 1 to 2 sessions of preoperative voice therapy and 4 to 6 sessions of postoperative therapy. Patients may also benefit from a subsequent series of voice therapy (1 to 3 sessions) months after the initial voice therapy to evaluate transfer and retention of the new vocal behaviors.
VOCAL HYGIENE
Vocal hygiene is the foundation of voice therapy. Patients are taught to take care of their vocal fold tissues by keeping hydrated and limiting laryngeal irritants. The best voice therapy starts with the patient taking active control of his or her vocal health. In addition, good vocal hygiene may decrease susceptibility to postoperative scarring (8). Two general topics are included in this circle: hydration and laryngopharyngeal reflux (LPR).
Hydration
Laryngeal sicca is increased viscosity of laryngeal secretions and is a result of the reduction of water in the body. Patients should be educated concerning why drinking water is important to the physiology of vocal production; they should not simply be told “to drink 8 glasses of water a day.” Increased viscosity of secretions may cause increased viscosity of vocal fold surfaces and, in turn, cause increased heat, friction, and edema of the vocal folds, which may increase the risk of phonotrauma (9). Research has shown that hydrated vocal folds vibrate with less subglottic pressure than do nonhydrated vocal folds, especially at high pitches (10,11,12,13,14). Hydrated vocal folds are less predisposed to trauma than dry vocal folds and show more resilience from trauma (i.e., phonotrauma) than dry vocal folds (9,12,13,14,15). Interested readers are referred to a review article by Leydon et al. (16). Patients may hydrate internally (i.e., drink water), externally (i.e., steam shower, steam inhaler, and/or hot water vaporizer), or both, based on medical history and individual need. Hygiene programs should be individualized for each patient. For example, if a patient is diagnosed with congestive heart failure, they may not be able to drink large quantities of water. In addition, smoking cigarettes or other substances should be eliminated. Engaging in voice therapy when patients continue to use laryngeal irritants (e.g., smoking) is obviously counterproductive to therapeutic success.
Laryngopharyngeal Reflux
Patients diagnosed with LPR should be medicated (e.g., proton pump inhibitors, H2 blockers, antacids) for this disease and engage in behavioral LPR treatment if needed (see Chapter 59). LPR may inflame the vocal folds, change the biomechanics of phonation, and potentially influence vocal fold pathologies (17). Initiating voice therapy with the healthiest vocal folds possible is the launch pad of therapy. Voice therapy is often used in conjunction with medical intervention in this circle.
DECREASE PHONOTRAUMA
The second circle is entitled decrease phonotrauma (vocal abuse/overuse) and is defined as a voice produced with too much effort for increased durations of time or at an inordinately high volume, often resulting in organically based vocal fold pathology. Phonotraumatic vocal behaviors may result in benign vocal fold lesions (e.g., nodules, cysts, fibrous mass, polyps) and scar. Such vocal behaviors as screaming, yelling, throat clearing, continued voicing while sick, vocalization during vigorous exercising, vocal overuse, and speaking over background noise are examples. Although modern-day voice therapy is much more than a “do/don’t” list, the prevailing “don’t” recommendation in voice therapy is “don’t scream.” High-pitched screaming may result in vocal fold hemorrhage. Vocal overuse may also cause vascular changes (i.e., vascular permeability) in the vocal folds, which may predispose patients to have small and large hemorrhages, often recurrent in nature. Cumulative microtrauma to the vocal fold tissues may result in scarring, sulcus vocalis, or both. Voice therapy is often used in conjunction with surgical intervention for phonotraumatic lesions in this circle.
Patients should be educated concerning the first two circles (increase vocal hygiene and decrease phonotrauma) in the first and second sessions of voice therapy. If patients show difficulty with compliance to increasing vocal hygiene and decreasing phonotrauma, prognosis for improvement in voice therapy is guarded.
INCREASE COORDINATED VOICE PRODUCTION
The third circle, increase coordinated vocal production (vocal misuse), is the crux of voice therapy. Uncoordinated vocal production is defined as an abnormal-sounding voice production resulting from the imbalance of respiration, phonation, and resonation. As illustrated in Figure 71.2, patients may have initially engaged in phonotraumatic behaviors and developed benign vocal fold lesions only to perpetuate their problems by producing voice in an unbalanced manner. Although faulty hygienic and phonotraumatic behaviors may have decreased, the patient now uses maladaptive compensatory voicing techniques, which places them in the third circle. Alternatively, patients may have a normal larynx but produce voice in an unbalanced manner. Examples of this include primary muscle tension dysphonia (MTD) and, the most extreme case, functional aphonia. Examples of poor balance between respiration, phonation, and resonation include “holding breath back” at the level of the vocal folds and respiratory mechanism (e.g., faulty airflow management), extra intrinsic and extrinsic laryngeal muscular tension (e.g., high larynx and glottal/supraglottic constriction), and abnormal pitch and intensity. These examples frequently define MTD. Often patients will complain of vocal fatigue and general tightness/constriction in the neck region. It is important not only to ask patients about the sound of their voice production but also about the “feel” of their voice production. Some patients are not so bothered by the sound of their voice but rather the feel.
VOICE THERAPY APPROACHES
The following is a brief synopsis of a variety of different voice therapy approaches that “rebalance” the voice production system. The types of therapies listed in the following are not intended to be comprehensive nor instructive in nature; instead, they are a description of the most commonly used voice therapies. “Typical” voice disorders may be paired with specific voice therapies; however, there is no general agreement among speech-language pathologists about which voice therapies to use with specific voice disorders. In part, this is because the medical disorder (e.g., nodules or vocal fold paralysis) does not necessarily determine how the patient uses his or her mechanism. Thus, it is much more important to treat the vocal behavior versus the voice disorder. Most speech-language pathologists use a combination of the therapies listed and do not use one therapy in particular. Although the following list defines each specific therapy, voice therapy is not “cookbook care.” Each patient presents with individual needs, and some therapies work better with some patients than others.
Accent Method
The accent method, originally developed by Smith and Thyme (18), focuses on rhythmic breathing as the primary control mechanism and pairs body movement with respiration and phonation to rebalance the system. The method trains patients to produce easy voicing, abdominal breathing movements (by alternating contraction and release), and open throat postures. These productions are achieved by using rhythmic vocalizations of consonant sounds (called accents), in combination with body movements (e.g., swaying arms or rocking back and forth), while stressing respiratory support for each accent. Proponents of this method report that patients acquire optimal respiratory support, coordination of exhalation and phonatory onset, and phonatory effort (19). Research investigating the efficacy of the accent method shows good outcomes (19,20).
Anatomic/Physiologic Explanation
The rhythmic pairing of timing with respiration and phonation may promote motor learning of new phonatory behaviors (21).
Application
The accent method may be used to treat benign lesions, MTD, vocal fatigue, paradoxical vocal fold motion, and mild glottal incompetence.
Confidential Voice
Confidential voice therapy is used to reduce the force of vocal fold collision and excessive laryngeal hyperfunction during phonation. A breathy voice produced with slightly abducted vocal folds (22) is the therapeutic goal. The slight abduction of the vocal folds results in increased airflow, decreased loudness, and decreased collision force. Although a breathy voice is not the final goal of therapy, it is encouraged for a prescribed period to promote mucosal healing. Confidential voice therapy allows surgical
sites to heal without strong collision forces/stress impact, decreases lesion size, eliminates excessive muscular activity, and increases awareness of habitual loudness levels.
sites to heal without strong collision forces/stress impact, decreases lesion size, eliminates excessive muscular activity, and increases awareness of habitual loudness levels.
Anatomic/Physiologic Explanation
Producing a breathy voice results in slightly abducted vocal folds, which results in smaller amplitudes of vibration and decreased collision force/stress impact. As a result, the vocal folds should be protected from further injury and allowed to heal.
Application
Confidential voice therapy may be used to treat benign lesions, MTD, and it can be used during the postoperative period of voice reinstatement. It is not appropriate for patients with voice problems related to glottal incompetence. Also, confidential voice is only used for a period of time to promote vocal fold healing; once that period is finished, the voice production is shaped into a healthy vocal production by other therapies mentioned in this chapter. A soft, breathy voice is not an appropriate goal of any voice therapy technique.
Lee Silverman Voice Treatment
Lee Silverman voice treatment (LSVT) is the most researched voice therapy protocol to date. LSVT was developed to address the hypokinetic dysphonia most frequently associated with Parkinson disease. LSVT is a systematic voice therapy approach that focuses on increasing loudness during four sessions per week for 4 weeks (23,24,25). Patients are trained to “recalibrate” their habitual speaking volume to one louder because the loudness that they think is normal is, in reality, too quiet. Having patients use a very loud voice also improves their articulatory precision and inflection. Treatment and home practice are intensive, and a high degree of independent compliance is required by the patient. The efficacy of this treatment has been well researched (23,24,25,26,27). It should be mentioned that there is a modified version of LSVT called Pitch Limiting Voice Treatment, which requires patients to voice in a low and loud pitch to increase loudness and speech intelligibility (28). Two other therapy programs designed from the LSVT theoretical framework are LSVT (LOUD) and LSVT (BIG) that may be used with patients with Parkinson disease, the aging voice, and other conditions including stroke, multiple sclerosis, cerebral palsy, and Down syndrome (29).
Anatomic/Physiologic Explanation
Loud speech tends not only to be more intense but also more intelligible. Many of the characteristics of speech produced in noise (i.e., loud speech) are perceptually more intelligible than conversational speech produced in quiet (29




Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree