Vitreoretinal Dystrophies
Hermann D. Schubert
William Tasman
Vitreoretinal dystrophies may present on routine ophthalmologic examination as high myopia, strabismus, retinal detachment, vitreous hemorrhage, or abnormal fundus pigmentation. The ocular findings are either isolated1,2,3,4 or part of a syndrome, such as Robin syndrome (also known as the Pierre-Robin syndrome)5; one of the clefting syndromes;6 or skeletal dysplasia.7 Although the gestalt of retinoschisis,1 familial exudative retinopathy (FEVR),2 or original Wagner disease (4) emerges with ease, lengthy deliberation is needed for conceptual separation of some of the syndromes that are not restricted to the eye.7,8,9,10,11,12 Although the identification of specific genes is rapidly emerging.13,14,15,16,17,18,19,20,21,22,23,24,25,26,27,28,29,30,31,32,33,34,35,36,37,38,39,40,41,42,43 molecular screening is still guided by history and clinical findings. Until large-scale genetic screening becomes routine, at which point it may precede and replace clinical examination, it is not always clear to the practicing physician which of the polymorphous signs to include at this mostly descriptive stage of nosology, with subsets and syndromes based on somewhat arbitrary definitions.
An ocular dystrophy is a congenital bilateral degeneration of ocular tissues, here predominantly involving the vitreous and retina. The degeneration may be either stationary or progressive. Dystrophic vitreal changes involve liquefaction (synchysis) of the gel and collapse (syneresis) of the collagenous structure. Thus, destruction of the vitreous gel is superimposed on the aging process.12,44 Microscopically, the liquefied vitreous appears optically empty; collapse of the vitreous collagen causes it to appear veil-like. Vitreoretinal adhesions may be absent or abnormally firm. Dystrophic retinal changes include intraretinal splitting, atrophy, hole formation, and the accumulation in or migration of pigment from the pigment epithelium. In addition, extraretinal changes sometimes occur. These changes present as selective atrophy of the retinal pigment epithelium (RPE), which appears as choroidal tesselation. Independent of this, choroidal stromal atrophy has been described.8
Although vitreoretinal dystrophies are rare in everyday clinical practice, they are found with greater ease by the prepared examiner. Once a genetic disease is clinically suspected, a search for information on mutations can be initiated through the Online Mendelian Inheritance in Man website (OMIM at www.ncbi.nlm.nih.gov/Omimfaq.html).
It is the purpose of this review to present the basic pathology, as well as the genetic and clinical features, of nine vitreoretinopathies in which primary retinal involvement is accompanied by passive secondary vitreal changes. The habit of thinking of vitreoretinal dystrophies, especially in children, may lead to earlier recognition of patients at risk for retinal detachment and consequent visual loss.
X-Linked Hereditary Retinoschisis
Although both peripheral and macular retinoschisis were first described in 1898,45 the other vitreoretinal dystrophies have been described only more recently. The history of the recognition and naming of retinoschisis is particularly interesting, mirroring the progressive characterization of the lesion, and thus may be helpful in understanding it:
1913: Pagenstecher noted the inheritance of “solutio retinae” in hypermetropic children.46
1932: Anderson localized the “anterior dialysis” to the inferotemporal quadrant in nonmyopic young males.47 Thomson emphasized macular involvement.48
1938: Mann and MacRae theorized that the “congenital vascular veils” in the vitreous are the result of retinal splitting.49
1948: Juler described retinal detachment in children with thinning and ruptures of the inner linings of the cysts.50 It was then assumed that the pathology was retinal but involved secondary changes in the vitreous.
1950: Sorsby and colleagues recognized the sex-linked inheritance of retinoschisis.1 Combining this finding with the previous views, they postulated that the veils represent ruptured retinal cysts, which, at a later stage, probably progress to congenital falciform detachment and pseudoglioma.
1953: Jager coined the term “retinal schisis”.51
1953–54: Kleinert52 and MacRae53 agreed with the concept of central and peripheral splitting of the retina.
1960–61: Balian and Falls54 and Gieser and Falls55 emphasized that the congenital vascular veils in the vitreous are combined with macular changes.
1964–66: Sarin and associates56 and Sabates57 identified members of the same families who had “hereditary retinal schisis.”
1973: Forsius and colleagues confirmed the X-linkage of retinal schisis and found that the maculopathy is present in virtually all cases.58
1976: Harris and Yeung classified retinoschisis into stages based on its degree of severity, specifically with respect to the occurrence of striation and atrophic and pigmentary changes.59
1983: Wieacker and coworkers assigned the responsible gene to band Xp 22.2 of the human X chromosome by linkage analysis.13
1997: Sauer and coworkers cloned the gene and named it XLRS1.14
1998: The Retinoschisis Consortium published an updated list of XLRS mutations. Today, these updates are published on the Internet at www.dmd.nl/rs/rs.html.15
2000: Grayson and coworkers demonstrated retinoschisin, the X-linked retinoschisis protein secreted by photoreceptor cells.16 This protein also is found in bipolar cells, but not in Muellerian cells.17 Retinoschisin is important for cell–cell and cell–matrix interactions, in that it maintains normal retinal architecture.18 Defective cell–cell interaction related to mutations might be the link to structural schisis.19
X-linked retinoschisis can be called a retinovitreal dystrophy because retinal schisis, not vitreous syneresis is the predominant sign. The common denominator of the retinal changes is thought to be Mueller-cell degeneration related to defective retinoschisin,19,60 the sequelae of which are most visible in the fovea and in the periphery of the inferotemporal fundus,61 Only peripheral changes may be present in the rare autosomal-dominant form.62
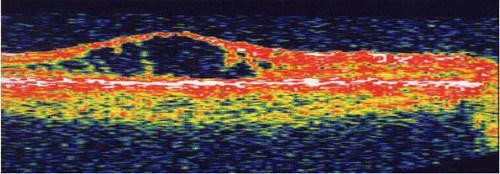
The wide range of biomicroscopic findings changes with the duration of the condition and age of the patient.1 The posterior vitreous adhesion (premacular and prepapillary, as well as perivascular) is well developed in young individuals. Vitreous attachments to the inner layer of the schisis can cause the progression of schisis through traction, particularly if vitreous contraction is accelerated by vitreous hemorrhage. Vitreous traction may lead to nasal dragging of the retina.63 The inner schisis layer consists of glia, nerve fiber layer, and vessels.61 Ultrastructural studies confirm the split along the ganglion cell and nerve fiber layer that separates cell processes from their bodies in the inner nuclear layer; this results in a picture of “decapitated and degenerated Mueller cells”.64 Although the inner layer of the schisis consists mostly of glial cells, the outer layer also provides a glial lining of the schisis cavity.18,64 Because vascularization of the inner retinal layers extends to the middle limiting membrane.65 schisis, however, takes place internal to the inner nuclear layer; the deep retinal capillaries may be disrupted, appearing angiographically as areas of nonperfusion.66 Inner-layer atrophy also may ensue as a result of chronic inner-layer ischemia and glial-cell decapitation. Atrophic holes in the inner layer and perivascular gliosis may be the biomicroscopic corollaries of angiographic nonperfusion. The outer layer may undergo atrophy or may be invaded by proliferations of the pigment epithelium60,61 Retinal schisis involves a delicate balance between vitreous traction on the inner layer and the opposing strength of residual intraretinal bridges of tissue and adhesions on the outer layer of schisis to the pigment epithelium. Intraretinal strands of tissue that bridge the schisis cavity have been shown in vivo using the retinal thickness analyzer and optical coherence tomography (OCT).67,68 If the vitreous gel is collapsed, the inner wall of the schisis is found in the retrolental space.54,61 Not surprisingly, such bullous schisis is more common in the young (i.e., in children younger than 10 years).69,70,71 often accompanied by vitreous and/or intraschisis hemorrhage.69 Exudative, Coats-like maculopathy, as well as intraschisis hemorrhage, may be related to angiomatous proliferations.72 Visual loss in young patients often is associated with a contraction of the adherent vitreous, as well as bullous schisis and its complications. This is a dynamic process; therefore, with increasing age, bullous schisis tends to flatten spontaneously in the vast majority of cases.69,71 The application of a laser beam to the area of schisis has been shown to disrupt the equilibrium of vitreous traction and retinal adhesions and to produce rhegmatogenous detachments resulting from outer layer breaks, as well as from full-thickness retinal breaks.73
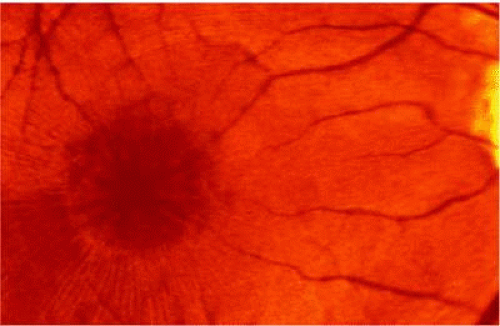
Clinically, retinal schisis presents with decreased central visual acuity, absolute scotomas, or both.1,54,59 Children may have strabismus and nystagmus.46,69 As in FEVR, but in contrast to Wagner and Stickler syndrome, the refraction tends to be hypermetropic (hypermetropic amblyopia) (1,46,47,52,53,54,55,61,70). On biomicroscopic examination, edema and cystic central macular schisis of the retina are apparent in virtually all cases.58,59 Loss of macular reflex, which may be an early sign,55,56 is followed by a wheel-like formation.58 a multicystic radiate appearance (Fig. 61.1),59 pigmentary degeneration, and cystic macular atrophy (Fig. 61.2).59 These macular changes, not bullous schisis per se, determine visual loss in patients, particularly those in the fourth or fifth decade of life.74
The electroretinogram (ERG) is characterized by preservation of the negative A-wave and loss of the positive B-wave, resulting in the so-called “electronegative dark-adapted ERG” in X-linked retinal schisis.29 Exceptions to this pattern exist; indeed, a normal ERG may occur.29 It has been suggested that the Mueller cell makes little contribution to the B-wave and that the reduced B-wave response to light onset is related to dysfunction of the postreceptor bipolar system.30 This is in keeping with the finding that retinoschisin functions in the inner layer, which includes bipolar cells.16,19
Peripheral retinal schisis is present in approximately half of all patients and, in 96% of these patients, it is located in the inferotemporal quadrant.70 At least initially, the inner layer of the schisis is attached to the vitreous and features vessels, an internal limiting membrane, and a nerve fiber layer. These tissues undergo progressive atrophy as well as reactive gliosis, which in a perivascular location may appear as vascular sheathing (Fig. 61.3). Total atrophy may result in dehiscences and peripheral arborization of the retinal vasculature.54,55,66 Optic atrophy may follow.61 The outer layer of the schisis cavity also undergoes atrophy, reactive gliosis, intralayer pigment migration, and hole formation. A rhegmatogenous detachment is the sequela in 4% to 22% of all patients.51,63,71,74,75,76 With time, the vitreous undergoes syneresis and detachment.52,54,61 Vitreous detachment actually may improve the schisis by releasing traction. Adhesions to retinal vessels are responsible for frequently found vitreous hemorrhages.50,52,61
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree