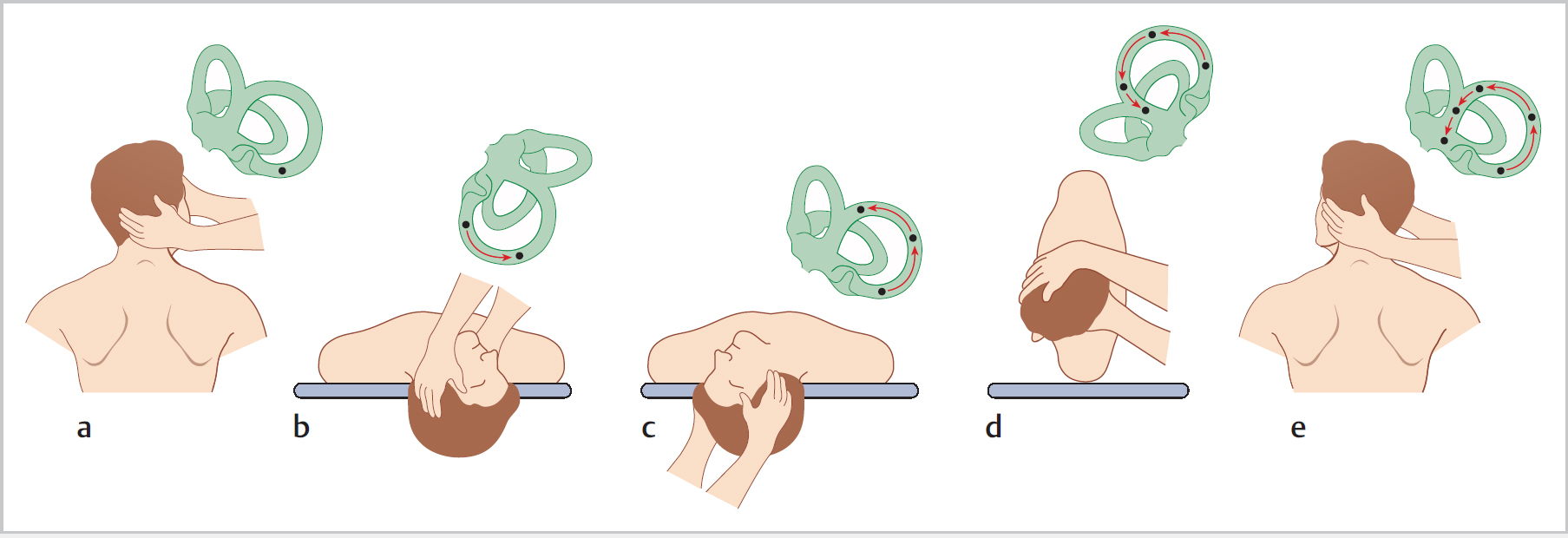
17 Vestibular Disorders • Postural control required to maintain stable image on the retina despite head movements and to prevent falling and possible injury • Balance is dependent upon visual input (~70%), proprioception (~15%), and vestibular input (~15%) • Dizziness encompasses various symptoms, including vertigo, which tends to be associated with peripheral vestibular disorders • However, vertigo can be seen with migraine, multiple sclerosis (MS), cerebrovascular accident (CVA), vestibular schwannoma, epilepsy, medication • Vertigo is the sensation of rotation or movement of one’s self or of one’s surroundings in any plane; it is disabling • Dysequilibrium is when the brain gets inadequate information from somatosensory, visual, or vestibular systems and patient feels unsteady • An individual with vertigo or dizziness that impairs their driving has an obligation to inform the relevant authority to assess their fitness to maintain a license; attacks coming on without enough warning to be able to safely get to the side of the road will be significant, as will response to treatment; specific guidance is usually available (such as from the DVLA in the United Kingdom) • Multi-level vestibulopathy: in elderly people where reduced quality and quantity of sensory information arise from multiple sensory pathways, all of which may be optimized to aid the patient • Anxiety can lead to hyperventilation with light-headedness and dizziness rather than true vertigo; the anxiety may result from a previous vestibular insult that has been compensated for • The British Society of Otology has a selection of videos relating to benign paroxysmal positional vertigo (BPPV) assessment and management, and clinical balance function testing (https://entuk.org/bso/videos). These include: • Pathology: • Aetiology: • Epidemiology: • Symptoms: • Ix: – Nystagmus rotatory with latency of a few seconds, fatigues after 30 to 40 s – Torsional, beats towards floor (geotropic), direction reverses on sitting up • Assessment and management – Testing for posterior and anterior canal BPPV: http://www.youtube.com/watch?v=Ew14aZqiUrw – Treatment for canalithiasis of posterior and anterior canal: http://www.youtube.com/watch?v=o4CKy3R1SPA – Stapedectomy: http://www.youtube.com/watch?v=h2G2xuB0kOo – Rinne and Weber tuning fork tests: http://www.youtube.com/watch?v=RVH4K4EcsiA – Hearing mechanism: http://www.youtube.com/watch?v=GGqfRvCkt-w • Less common; can be tested for by sitting patient at 30° head-up on couch and laterally rotating head to either side • Will give geotropic nystagmus (horizontal) when head turned to either side • Epley equivalent involves “barbecue-spit” rotation • Potential to surgically occlude affected canal • Downbeat nystagmus with torsional component • Disease described below; syndrome associated with other diagnoses (e.g., syphilis, otosclerosis) • Pathology: uncertain and all theories have flaws: Fig. 17.1a–e The Epley manoeuvre (shown testing the right ear). a The patient is seated upright with the head turned 45° to the right. b The patient is moved rapidly into the supine position with the head extending just beyond the examining table and the right ear downward. The position is held until nystagmus fatigues, usually ~30 s. c The head is rotated 90° to the opposite side, stopping with the right ear upward. The position is held for ~30 s. d The patient rolls onto the left side while the examiner maintains the head position looking over the left shoulder such that the nose is now angled to the floor. The position is held for ~30 s. e The patient is lifted to a sitting position, swinging their legs over the left side of the bed.
17.1 Principles and Definitions
17.2 Benign Paroxysmal Positional Vertigo
17.2.1 Assessment and Management
 Testing for posterior and anterior canal BPPV: http://www.youtube.com/watch?v=Ew14aZqiUrw
Testing for posterior and anterior canal BPPV: http://www.youtube.com/watch?v=Ew14aZqiUrw
 Treatment for canalithiasis of posterior and anterior canal: http://www.youtube.com/watch?v=o4CKy3R1SPA
Treatment for canalithiasis of posterior and anterior canal: http://www.youtube.com/watch?v=o4CKy3R1SPA
 Stapedectomy: http://www.youtube.com/watch?v=h2G2xuB0kOo
Stapedectomy: http://www.youtube.com/watch?v=h2G2xuB0kOo
 Rinne and Weber tuning fork tests: http://www.youtube.com/watch?v=RVH4K4EcsiA
Rinne and Weber tuning fork tests: http://www.youtube.com/watch?v=RVH4K4EcsiA
 Hearing mechanism: http://www.youtube.com/watch?v=GGqfRvCkt-w
Hearing mechanism: http://www.youtube.com/watch?v=GGqfRvCkt-w
17.2.2 Posterior Scc BPPV
 Usually in posterior Scc
Usually in posterior Scc
 Canalolithiasis or free-floating debris (otoconia) in endolymph causes continuing stimulation after movement of head has ceased
Canalolithiasis or free-floating debris (otoconia) in endolymph causes continuing stimulation after movement of head has ceased
 Cupulolithiasis: debris from otolith organ becomes attached to cupula
Cupulolithiasis: debris from otolith organ becomes attached to cupula
 Usually idiopathic; ~20% associated with minor head trauma
Usually idiopathic; ~20% associated with minor head trauma
 Any age (peak 6th–7th decades); most common cause of vertigo
Any age (peak 6th–7th decades); most common cause of vertigo
 Associated with preceding inner ear disease (e.g., Ménière, vestibular neuritis)
Associated with preceding inner ear disease (e.g., Ménière, vestibular neuritis)
 Vertigo of seconds to minutes duration associated with rapid changes in head position (e.g., rolling over in bed, turning to reach objects on high shelves)
Vertigo of seconds to minutes duration associated with rapid changes in head position (e.g., rolling over in bed, turning to reach objects on high shelves)
 Attacks often in clusters, may recur after period of remission
Attacks often in clusters, may recur after period of remission
 Dix–Hallpike manoeuvre: provokes vertigo and nystagmus (affected ear downwards)
Dix–Hallpike manoeuvre: provokes vertigo and nystagmus (affected ear downwards)
 Spontaneous remission rate high
Spontaneous remission rate high
 Epley manoeuvre (Fig. 17.1) to disperse canal debris into utricle (where it is inactive); effective in ~85% cases
Epley manoeuvre (Fig. 17.1) to disperse canal debris into utricle (where it is inactive); effective in ~85% cases
 Semont manoeuvre is alternative: head rotated 45° away from affected ear; lie quickly on side of affected ear; stay 1 min then quickly over onto opposite side (i.e., for R side, go from R ear down to L eye down)
Semont manoeuvre is alternative: head rotated 45° away from affected ear; lie quickly on side of affected ear; stay 1 min then quickly over onto opposite side (i.e., for R side, go from R ear down to L eye down)
 Brandt–Daroffhead exercises
Brandt–Daroffhead exercises
 Avoid vestibular sedatives (e.g., prochlorperazine)
Avoid vestibular sedatives (e.g., prochlorperazine)
 Posterior Scc occlusion in severe recurrent cases; singular neurectomy possible
Posterior Scc occlusion in severe recurrent cases; singular neurectomy possible
 The British Society of Otology has a selection of videos relating to BPPV assessment and management, and clinical balance function testing (https://entuk.org/bso/videos). These include:
The British Society of Otology has a selection of videos relating to BPPV assessment and management, and clinical balance function testing (https://entuk.org/bso/videos). These include:
17.2.3 Lateral Canal or Horizontal BPPV
17.2.4 Superior Scc BPPV
17.3 Ménière Disease
 Disease of the membranous inner ear, with excess endolymph (endolymphatic hydrops) production (stria vascularis), or reduced absorption (endolymphatic sac)
Disease of the membranous inner ear, with excess endolymph (endolymphatic hydrops) production (stria vascularis), or reduced absorption (endolymphatic sac)
Vestibular Disorders
Only gold members can continue reading. Log In or Register to continue

Full access? Get Clinical Tree