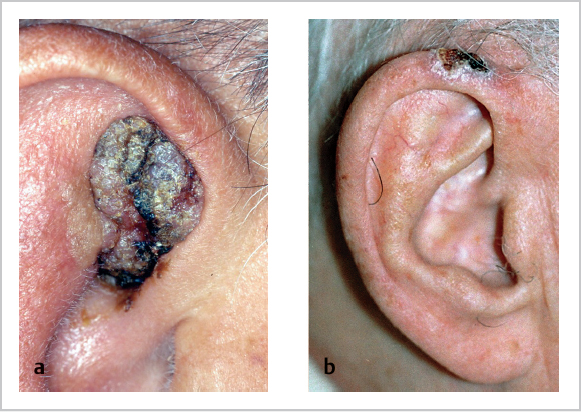
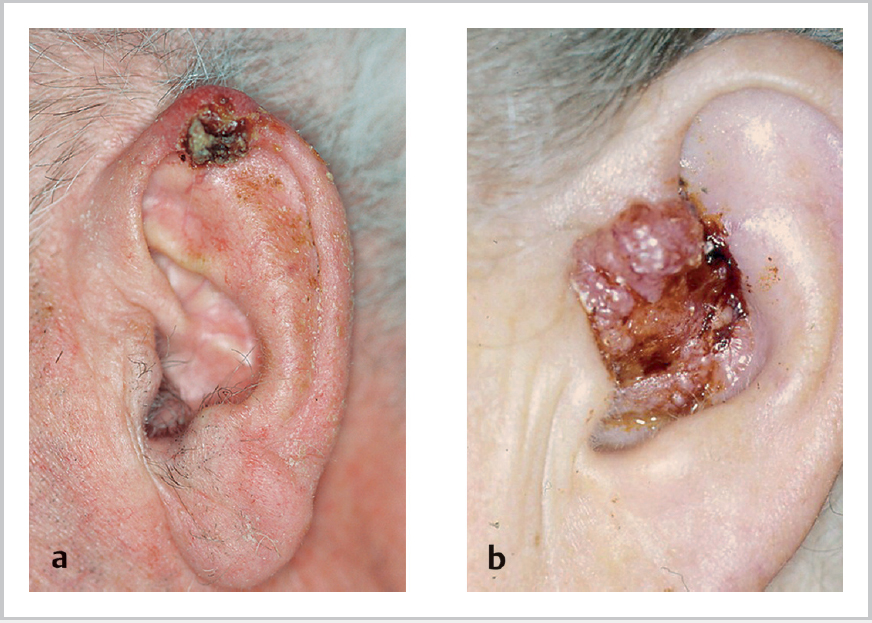
11 Tumours of the Ear and Skin • Tumours of the ear are rare: ~70% pinna, 20% external auditory canal (EAC), 10% middle ear (ME) • Squamous cell carcinoma (SCC) and basal cell carcinoma (BCC) most common (respective incidences vary country to country) (Figs. 11.1 and 11.2a) • Rx: primary resection with appropriate margins; minor superficial lesions with no cartilage invasion or fixation may have radiotherapy (RT) alone • Benign include nevus, epithelioma adenoides cysticum, molluscum contagiosum • SCC (Fig. 11.2b) • Adenocarcinoma: very aggressive (usually fatal within 4 years), often presenting with VII n palsy • Adenoid cystic: most common “ceruminous” tumour; long natural history, painful • Also adenoma, mucoepidermoid carcinoma; malignant melanoma very rare, as is BCC of EAC • Choristoma = normal tissue in abnormal site (e.g., salivary gland in ME): rare; may be attached to VII n • Adenoma (benign): cause unilateral progressive conductive hearing loss (HL), TM intact in 75% cases; 2nd most common after glomus tumours, but still rare • Adenocarcinoma: very rare; cause deafness, pain, VII n palsy • SCC: • Other benign tumours: • Pathology: • Epidemiology:
11.1 Incidence and Site
11.2 Pinna
11.3 EAC
 90% of malignant tumours, slow-growing, spread via cartilage portion and later into ME, parotid, sternocleidomastoid muscle
90% of malignant tumours, slow-growing, spread via cartilage portion and later into ME, parotid, sternocleidomastoid muscle
 20% lymph node (LN) spread (posteriorly to mastoid nodes, inferiorly to level III, anteriorly to preauricular)
20% lymph node (LN) spread (posteriorly to mastoid nodes, inferiorly to level III, anteriorly to preauricular)
 Associated with chronic inflammation, RT
Associated with chronic inflammation, RT
 Rx: consider lateral temporal bone resection, ± neck dissection; post-operative RT
Rx: consider lateral temporal bone resection, ± neck dissection; post-operative RT
 Prognosis very poor if node positive
Prognosis very poor if node positive
11.4 Middle Ear
 Most common epithelial ME malignancy, but rare
Most common epithelial ME malignancy, but rare
 Association with chronic otitis media in 85%, irradiation
Association with chronic otitis media in 85%, irradiation
 Extensive bony destruction, most easily through tegmen to middle cranial fossa (dura is a relatively strong barrier); intracranial invasion along VII n and VIII n in internal auditory canal; IX n and XII n involvement shows skull base involved; can also extend to temporomandibular joint, parotid, via eustachian tube to nasopharynx
Extensive bony destruction, most easily through tegmen to middle cranial fossa (dura is a relatively strong barrier); intracranial invasion along VII n and VIII n in internal auditory canal; IX n and XII n involvement shows skull base involved; can also extend to temporomandibular joint, parotid, via eustachian tube to nasopharynx
 LN involvement in 10 to 15% at presentation, rare distant metastasis; death by cachexia secondary to pain because cranial nerve (CN) involvement, though sometimes invasion of meninges leads to intracranial complications and erosion of jugular bulb or carotid is possible
LN involvement in 10 to 15% at presentation, rare distant metastasis; death by cachexia secondary to pain because cranial nerve (CN) involvement, though sometimes invasion of meninges leads to intracranial complications and erosion of jugular bulb or carotid is possible
 Rx: surgery (petrosectomy) + RT; palliative
Rx: surgery (petrosectomy) + RT; palliative
 5-year survival ~35% (better for EAC than ME); prognosis very poor if node positive
5-year survival ~35% (better for EAC than ME); prognosis very poor if node positive
 Osteoma
Osteoma
 VII n schwannoma (usually at geniculate ganglion)
VII n schwannoma (usually at geniculate ganglion)
 Hemangioma, neurogenic
Hemangioma, neurogenic
 Sarcoma
Sarcoma
 Multiple myeloma
Multiple myeloma
 Malignant xanthoma
Malignant xanthoma
 Rhabdomyosarcoma most common in children; may require surgery ± chemoradiotherapy
Rhabdomyosarcoma most common in children; may require surgery ± chemoradiotherapy
 Also direct extension (e.g., from nasopharynx, external ear, parotid, meningioma) and distant metastases (kidney, lung, prostate, thyroid, breast)
Also direct extension (e.g., from nasopharynx, external ear, parotid, meningioma) and distant metastases (kidney, lung, prostate, thyroid, breast)
11.5 Glomus Tumours
 Correct (WHO) term is paragangliomas; aka chemodectomas; arise from paraganglionic tissue (chemoreceptor cells)
Correct (WHO) term is paragangliomas; aka chemodectomas; arise from paraganglionic tissue (chemoreceptor cells)
 Common embryological origin (neural crest) and association with neural structures
Common embryological origin (neural crest) and association with neural structures
 90% adrenal (phaeochromocytomas); 10% nonadrenal (85% of which are abdominal, only 3% H&N); subdivided into abdominal and extra-abdominal
90% adrenal (phaeochromocytomas); 10% nonadrenal (85% of which are abdominal, only 3% H&N); subdivided into abdominal and extra-abdominal
 H&N paragangliomas associated with parasympathetic system
H&N paragangliomas associated with parasympathetic system
 Relative incidence: carotid > jugulotympanic > vagal
Relative incidence: carotid > jugulotympanic > vagal
 5th decade, F>M, may be multiple (show multicentricity); ~10%, autosomal dominant; usually benign and slow-growing but ~5% malignant; rarely (<1%) secrete neuropeptides (e.g., serotonin, vasoactive intestinal peptide)
5th decade, F>M, may be multiple (show multicentricity); ~10%, autosomal dominant; usually benign and slow-growing but ~5% malignant; rarely (<1%) secrete neuropeptides (e.g., serotonin, vasoactive intestinal peptide)
< div class='tao-gold-member'>
![]()
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree