Chapter 66 Vascular Considerations in Neurotologic Surgery
VASCULAR ANATOMY OF THE PETROUS BONE AND CEREBELLOPONTINE ANGLE
Internal Carotid Artery
The petrous segment of the internal carotid artery (ICA) begins as the vessel enters the periosteal-lined carotid canal, whereas the cavernous segment originates as it exits the apex of the petrous portion of the temporal bone and traverses the posterior part of the cavernous sinus. The petrous portion of the ICA, which lies immediately posterior to the bony eustachian tube but anterior to the jugular foramen, can be divided into vertical and horizontal segments that connect at the genu. The ICA is lined by cervical sympathetic ganglia throughout its course in the petrous canal, and aneurysms or lesions of the vessel that compress the nerves can cause a classic Horner’s syndrome.1 The ICA is also lined by a venous plexus in the distal part of the canal. The greater superficial petrosal nerve, which originates from the geniculate ganglion of the facial nerve, usually courses above and parallel to the horizontal portion of the petrous ICA. Special caution should be used when exposing the middle fossa floor and the petrous ICA because excessive traction of this nerve can cause postoperative facial nerve palsy.2 Similarly, the trigeminal ganglion lies over the medial portion of the petrous ICA, but it is usually separated from the vessel by dura or a variable layer of bone.
The petrous ICA has four main branches of importance to the neurotologic surgeon: (1) caroticotympanic artery, (2) stapedial artery, (3) artery of the pterygoid canal (vidian), and (4) periosteal artery.1,3 The caroticotympanic artery is often said to be a remnant of the embryonic hyoid artery, and arises from the proximal vertical part of the petrous ICA laterally and supplies the tympanic cavity. It anastomoses most commonly with the inferior tympanic artery. The stapedial artery is the source of the middle meningeal artery during development, but it rarely persists into adulthood. If present, a persistent stapedial artery passes through the floor of the middle ear and runs superiorly in a bony canal, in the obturator foramen of the stapes, and finally through the fallopian canal into the middle cranial fossa.3 Finally, the artery of the pterygoid canal (vidian) and the periosteal artery are often thought of as small collateral routes most likely branching off from the horizontal segment of the petrous portion or from the internal maxillary artery, and may have relevance in interventional embolization procedures as described later on.1
The intracavernous segment of the ICA begins at the level of the petrolingual ligament near the foramen lacerum, and most consistently gives off two branches known as the dorsal (meningohypophyseal trunk) and lateral (artery of the inferior cavernous sinus) main stem arteries.4 The intracavernous ICA is commonly divided into five segments for anatomic orientation, including a posterior vertical, posterior bend, horizontal, anterior bend, and anterior vertical segments.1
The dorsal main stem artery generally branches from the central one third of the convex outer margin of the posterior bend of the ICA. There is great variability in the origin of the branches of the dorsal main stem, but most investigators agree that three vessels—the tentorial artery (artery of Bernasconi-Cassinari), dorsal meningeal artery, and inferior hypophyseal artery—exist in some form.3 The tentorial arteries travel along the tentorium and may contribute blood supply for tentorial or proximal falcine meningiomas and tentorial dural arteriovenous fistulas, and blood supply to portions of CN III and IV.3,5 The inferior hypophyseal artery supplies the periphery of the anterior pituitary gland and forms a “circulus arteriosus” with the dorsal meningeal arteries around the root of the dorsum sella. The distal branches of the dorsal meningeal arteries may enter the internal auditory meatus as described in a few patients, and may represent a remnant of the fetal trigeminal artery.3
Although the dorsal and lateral main stem vessels are the most common branches given off by the intracavernous segment of the ICA, other arteries have been described. McConnell’s capsular artery, when present in about 8% of the population, originates from the horizontal segment of the intracavernous ICA, and supplies any combination of the inferior and peripheral aspect of the anterior lobe of the pituitary gland, the diaphragma sella, and the floor of the sella turcica.6 A persistent fetal trigeminal artery, although rare with an incidence of 0.06% to 0.6%, usually arises from the posterolateral or posteromedial aspect of the intracavernous ICA.3 It is most notable in the literature for producing unique clinical scenarios, including trigeminal neuralgia, oculomotor palsies, hyperprolactinemia, and an increased incidence of intracranial aneurysms.3 Finally, the ophthalmic artery and a superior hypophyseal artery have been shown to originate from the cavernous ICA in 1% to 7.5% and 16% of individuals, respectively.3,7
External Carotid Artery
Proximal to its terminal bifurcation, the external carotid artery gives rise to an anterior and posterior group of vessels, the latter of which consists of three arteries that relate to the petrous portion of the temporal bone. The ascending pharyngeal artery usually originates at or near the main bifurcation of the ICA and external carotid artery, and supplies the meninges around the jugular foramen as it passes through the foramen lacerum. As it travels upward with the carotid arteries, it gives off the inferior tympanic artery, which travels through the tympanic cavity with Jacobson’s nerve (inferior tympanic) via the tympanic canaliculus.2 The occipital artery arises from the posterior surface of the external carotid artery and traverses upward between the posterior belly of the digastric muscle and the internal jugular vein, and then medial to the mastoid process. After passing the longissimus capitis muscle, the vessel courses deep to the splenius capitis muscle, finally terminating at the fascia between the attachment of the sternocleidomastoid and the trapezius muscles at the superior nuchal line.2 Its branches supply several muscular and meningeal branches and often anastomose with branches of the external carotid and vertebral arteries.2 Its most notable branch is the mastoid artery, which supplies the posterior portion of the mastoid bone and runs through the mastoid foramen. Finally, the posterior auricular artery arises above the posterior belly of the digastric and travels between the parotid gland and the styloid process. The artery divides into posterior auricular and occipital branches, and develops a stylomastoid branch, which supplies the structures of the stylomastoid foramen and the facial nerve.2
Although not technically a direct branch of the external carotid artery, but rather a branch of the internal maxillary artery, the middle meningeal artery has clinical relevance in the various neurotologic approaches. As this vessel courses through the foramen spinosum of the sphenoid bone between the two roots of the auriculotemporal nerve, it enters the middle cranial fossa, dividing into two or three main branches. When performing extradural approaches to the floor of the middle fossa, the foramen spinosum is located anteromedial to the geniculate ganglion and anterolateral to the carotid canal. These branches—the anterior branch (frontalis), posterior branch (parietal), and middle branch—supply most of the supratentorial dura and calvaria. On entering the cranium, it also gives off the superficial petrosal artery, which enters the hiatus of the facial canal and supplies the facial nerve. Manipulation of this branch during transpetrosal approaches can result in facial nerve injury.2 Finally, the middle meningeal artery also gives rise to the superior tympanic artery just superior to the foramen spinosum, which runs with the superficial petrosal nerve through the superior tympanic canaliculus and supplies the canal of the tensor tympani muscle.
Vertebrobasilar Arteries
The AICA typically originates from the lower part of the basilar artery and divides into rostral and caudal trunks as it traverses the central part of the CPA. This main bifurcation often occurs proximal to the facial and vestibulocochlear nerves, and the two trunks formed are usually nerve-related.8 These branches can be divided into a premeatal segment, meatal segment, and subarcuate loop. In one study, a laterally convex curve or “loop” from the meatal segment was found to be medial of the internal acoustic meatus lying in the CPA in 33%, at the entrance of the meatus in 27%, and entering the internal auditory canal (IAC) in 40% of patients.8 A second laterally convex curve, known as a subarcuate loop, can also be seen in the subarcuate fossa and often gives the appearance of an M configuration.8 Although rare, in a few cases the lateral convex loop of the AICA can be embedded in the dura or bone covering the subarcuate fossa, or both.9 In such cases, freeing the artery from the dura and, if necessary, drilling the bone around the margin may aid in freeing this segment in anticipation for exposure of the posterior wall of the internal acoustic meatus.9
In the area of the CPA, the various branches of the AICA give rise to several nerve-related arterial branches from which originate the (1) labyrinthine (IAC), (2) recurrent perforating, (3) subarcuate, and, less commonly, (4) cerebellosubarcuate arteries. The labyrinthine arteries follow the vestibulocochlear nerve into the IAC, supplying the nerves, dura, and bone of the canal, and eventually terminate by giving rise to the anterior vestibular and common cochlear arteries, which supply the inner ear. Although the labyrinthine arteries most commonly arise from the premeatal segment of the AICA, some studies have reported anomalous cases where it originated directly from the basilar artery or from the PICA, or recurrent perforating, subarcuate, and cerebellosubarcuate arteries; however, this difference may be partially explained by the exact anatomic definition of the arteries in the different studies.8 The recurrent perforating arteries often course near the meatus and along the facial and vestibulocochlear nerves before supplying the brainstem. Finally, the subarcuate artery usually travels medial to the meatus, traversing the subarcuate fossa and petromastoid canal, sending branches to the petrous apex, the bone of the semicircular canals, and the posterosuperior portion of the vestibule.
The SCA originates most commonly from the basilar artery below, but adjacent to the origin of the posterior cerebral artery. The SCA generally bifurcates into rostral and caudal trunks, and branches from either make up the cortical arteries, which supply the upper two thirds of the petrosal surface, including both lips of the petrosal fissure.8 The first branch of the cortical arteries, when present in about half of the population, is referred to as a marginal branch, and its surface area supplied is inversely related to the supply of the AICA. Several anastomoses exist between the marginal artery and the AICA.
Dural Venous Sinuses
One must have an intimate knowledge of venous anatomy in neurotologic surgery to decrease the risk of complications from venous congestion. The petrosal vein (Dandy’s vein) parallels the trigeminal nerve just beneath the tentorium and drains into the superior petrosal sinus. The superior petrosal sinus, which lies at the attachment of the tentorium cerebelli to the superior margin of the petrous ridge, connects the cavernous sinus to the lateral extent of the sigmoid sinus. In addition to draining the petrosal veins that drain the cerebellum and brainstem, it also receives vessels from the inferior surface of the temporal lobe and the cavernous sinus. The transverse sinus begins as a confluence of sinuses at the level of the internal occipital protuberance between the tentorium cerebelli and occipitalis bone and runs laterally to join the sigmoid sinus. The anastomotic vein of Labbé, which drains the temporoparietal region, bridges the inferior surface of the temporal lobe to the transverse sinus. This vein is of special importance in petrosal approaches to the skull base because its injury can lead to speech disturbance and contralateral hemiparesis or hemiplegia.2 This vein is particularly at risk during subtemporal exposures. Excessive retraction of the temporal lobe can result in avulsion of the vein from its insertion into the relatively nonmobile transverse-sigmoid junction.
At its entrance to the jugular foramen, the jugular vein is separated from the inferior petrosal sinus by CN IX, X, and XI. This foramen is located at the lower end of the petro-occipital fissure, and is divided into a larger lateral opening that drains the sigmoid sinus and into a small medial petrosal part that receives the inferior petrosal sinus.2 The jugular bulb is inferior to the posterior floor of the middle ear cavity and generally lies inferior to the ampulla of the posterior semicircular canal; however, its location within the tympanic cavity is highly variable. Often, a high-riding jugular bulb can extend superiorly as high as the lateral semicircular canal and can interfere with visualization in Trautmann’s triangle in transpetrosal approaches as discussed in the next section.2 Finally, the internal jugular vein runs inferiorly from the bulb and is located posterolaterally to the ICA.
VASCULAR CONSIDERATIONS IN NEUROTOLOGIC APPROACHES
Transpetrosal Approaches
The transpetrosal approach, also known as the transtemporal approach, consists of three craniotomy techniques that open the posterior fossa dura anterior to the sigmoid sinus, through the posterior aspect of the petrous pyramid (Fig. 66-1). This set of approaches requires removal of 1 to 2 cm of retrosigmoid bone to allow for posterior displacement of the sigmoid sinus. A detailed explanation of the surgical technicalities and indications and exposure to the various approaches is provided elsewhere.
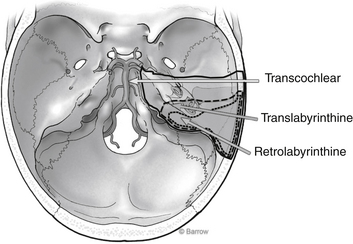
FIGURE 66-1 Surgical corridor afforded by the various transpetrosal approaches.
(Courtesy of Barrow Neurological Institute.)
Retrolabyrinthine
After the initial incision is made behind the postauricular sulcus, and the mastoid air system is thoroughly exenterated, the posterior limit for drilling is the sigmoid sinus. Using a large diamond burr, the sigmoid sinus must be skeletonized carefully. Some authors have suggested that a thin bone plate be left intact over the anterior aspect of the sinus to protect the vessel from the rotating shaft of the drill as it goes deeper into the temporal bone.2 If this bone plate begins to restrict sigmoid retraction, however, one can always fragment it to facilitate posterior mobilization. Other surgeons believe there is no need for preservation of this bony island, and they remove it and guard the vessel with a retractor. Either way, further exposure must be attained by retracting the sinus superiorly from the jugular bulb. In selected patients, the sigmoid sinus can be ligated to improve exposure; however, this can occur only when angiography shows a patent communication between the two transverse sinuses. Mastoid emissary veins are usually encountered and can be controlled with bipolar cautery; similarly, any lacerations to the sinus can readily be controlled with extraluminal tamponade with hemostatic gauze. Intraluminal packing of the sigmoid sinus is not recommended because there is always a risk for embolization of the packing material.
Translabyrinthine
As the dural flap is reflected posteriorly to expose the meatal structures and the CPA, the subarcuate artery or AICA may be encountered. As noted earlier, the subarcuate artery usually stems from the AICA and passes through the dura on the upper posterior wall of the meatus. This vascular anatomy tends to be variable, however, and in some patients the subarcuate artery, along with its origin from the AICA, may be incorporated into the dura on the posterior face of the temporal bone.9



