Varicella and Herpes Zoster Ocular Disease
Vincent P. De Luise
Varicella zoster virus (VZV) is a herpesvirus (Herpesvirus varicellae, family Herpesviridae) that causes both the cutaneous exanthem varicella (chickenpox) in children and the dermatomal eruption herpes zoster (shingles) in adulthood.1,2,3 The ocular manifestations of VZV infection can be divided into the ophthalmic sequelae of varicella and the ophthalmic sequelae of herpes zoster, the latter condition termed herpes zoster ophthalmicus. This distinction is useful because varicella ocular infection usually occurs in childhood and is self-limited, whereas herpes zoster ophthalmicus tends to arise later in life and can lead to protracted ocular complications and chronic neuralgic pain.
Humans are the only known natural hosts for VZV. As with the other herpesviruses, such as herpes simplex virus (HSV), cytomegalovirus (CMV), and Epstein-Barr virus, VZV can persist in a latent form. Nearly everyone with an initial VZV infection (varicella) recovers, but can harbor the latent virus in the trigeminal ganglion or in one of the sensory ganglia of the spinal cord. Although the majority of patients who have had varicella experience no further problems, approximately 20% will develop herpes zoster later in life, as a result of either reactivation of or reexposure to the VZV virus.2,3,4,5,6
VARICELLA
EPIDEMIOLOGY
Virtually all who live in a populous society eventually contract varicella, usually before 9 years of age.2,7,8 Transmission of the disease occurs less readily in uncrowded areas of the world, and infection occurs more often later in life in those areas.2,7,8
VZV present in respiratory secretions or cutaneous lesions can transmit varicella.9 The virus usually enters the host by way of the respiratory mucosa. After an incubation period of 10 to 21 days, during which time the virus replicates in regional lymph nodes, a systemic viremia ensues.2,7,8,9
The high prevalence of varicella has been reduced as a result of the development of a safe and effective vaccine (Varivax®), now approved for general use.10,11 The Varivax® vaccine is obtained from live attenuated viruses of the Oka strain of VZV.10,11 Immunization begins in childhood and booster injections are needed. The vaccine has been shown to be immunogenic and clinically effective in both healthy and immunocompromised children.12 Routine varicella vaccination programs for healthy children would result in significant savings in medical and work-loss costs.13 Herpes zoster may still occur after immunization, caused by reactivation of either the vaccine strain or a wild-type strain; however, herpes zoster appears to occur less frequently in patients who have received the vaccine than in patients who have had natural varicella.11,14,15
SYSTEMIC MANIFESTATIONS AND THERAPY
The main clinical manifestations of varicella are fever, malaise, and a mucocutaneous exanthem, all of which develop at the time of, or shortly after, the viremia. The cutaneous rash begins with macular and papular lesions, which evolve into vesicles before crusting. Although the varicella skin eruption is generalized, the lesions are more numerous on the face and trunk (Fig. 1) than on the extremities, creating a so-called centripetal rash. Mucosal vesicles occur but are less common than cutaneous lesions. New “crops” of macules, papules, and vesicles appear on the skin and evolve over the course of a few days, so lesions in different stages of maturity are typically present at any given time. The vesicles rupture and become encrusted approximately 1 week after their initial appearance, at which time the patient is no longer contagious. In the absence of secondary bacterial infection, cutaneous scarring in varicella is unusual.8,16
 Fig. 1 Varicella. Facial pocks in a 9-year-old black child. Cutaneous lesions are in various stages of evolution. |
Recovery from varicella is generally rapid and uneventful, occurring 1 to 2 weeks after onset of clinical disease. The immunocompetent patient is able to eliminate the viremia quickly by means of humoral antibodies, while cellular (lymphocyte-mediated) immunity controls intracellular virus. Nevertheless, some virus can enter sensory ganglia and may remain permanently dormant.17 Subsequent reactivation of the latent virus produces the quite different clinical picture of herpes zoster, presumably because the host is partially immune. Reactivation of the virus can occur idiopathically or in association with a decline in the patient’s immune status, reexposure to the virus, or surgical or other traumatic insults to the sensory nerves whose ganglia contain latent virus.2,5,6,7
Varicella is often more severe in infants and adults than in children, even in those at the extremes of age who seem otherwise healthy. The disease can be fatal in infants, probably because their immune systems are immature. Adults are especially susceptible to varicella pneumonitis.3,18 Immunocompromised patients at any age can develop widespread and sometimes fatal involvement of the viscera, vascular system, and central nervous system.2,3,19
Varicella is usually a benign disease that requires only symptomatic therapy with analgesics, antipyretics, antipruritics, and general hygienic measures. Aspirin should be avoided because its use is thought to be associated with an increased risk of postvaricella Reye’s syndrome.
Zoster immune globulin (containing antibodies against VZV) can prevent or ameliorate varicella in immunodeficient patients who have been exposed to the virus but who have not yet developed the disease.2,3 In addition to passive immunization, vaccination with the recently approved live attenuated varicella vaccine (Varivax®) may help to decrease the occurrence and severity of varicella in these patients. Immunocompromised patients with chronic varicella or varicella pneumonitis have been helped by the administration of intravenous vidarabine.20 Kunitomi and colleagues21 found that intravenous vidarabine and intravenous acyclovir were equally effective in treating immunocompromised children with varicella, whereas Balfour and co-workers22 and Shepp and co-workers23 found intravenous acyclovir to be significantly more effective than intravenous vidarabine in this situation, with minimal side effects.24
OCULAR MANIFESTATIONS AND THERAPY
Ocular manifestations of varicella infection include epibulbar conjunctival or limbal corneal “pocks” (round, focal accumulations of inflammatory cells, lymphocytes and neutrophils), punctate keratitis, nonherpetic dendriform keratitis, nummular keratitis, disciform keratitis or keratouveitis (Fig. 2).7,25,26,27,28,29,30,31,32 Rarely, varicella has been associated with gangrene of the eyelids, interstitial keratitis, progressive corneal ulceration (“melting”), extraocular muscle palsies, internal ophthalmoplegia, cataract, uveitis, retinopathy, or optic neuritis.26,28,33,34,35,36,37,38,39,40 Infants born with varicella (congenital varicella syndrome) can manifest microphthalmos, chorioretinitis, cataracts, microcephaly, deafness, and cardiac anomalies.28,41
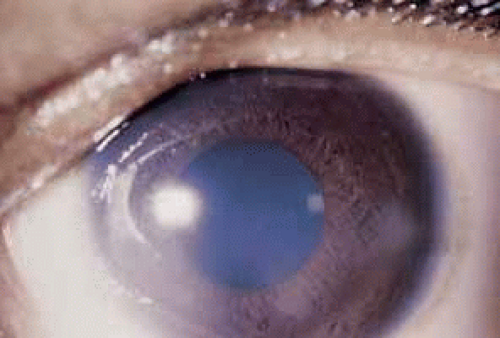 Fig. 2 Varicella nummular keratitis (same patient as in Fig. 1). |
Epibulbar pocks occur most often during active systemic varicella and are suspected to harbor live virus. Pocks can also develop weeks or months after the systemic disease, at which time they probably represent a sterile, phlyctenule-like, cell-mediated immunologic reaction to retained viral antigen (but not the live virus). In either case, the pocks persist for 1 to 2 weeks and then resolve spontaneously. These conjunctival lesions are visually insignificant, but corneal pocks can leave scarring and vascularization. Varicella pocks are can be treated empirically with a topical antiviral agent such as trifluridine or simply observed. Pocks that develop later respond to short-term pulsed topical corticosteroid therapy.
Punctate or dendritic epithelial keratitis can rarely occur during active varicella infection and is thought to be caused by proliferation of VZV in the corneal epithelium. Varicella keratitis closely resembles herpes simplex keratitis, including the presence of dendriform lesions and decreased corneal sensation,29 although varicella dendrites, similar to those of herpes zoster, consist of heaped up (rather than ulcerated as in herpes simplex) epithelium and are less responsive to topical antiviral therapy. The varicella dendrites can be removed by mechanical debridement using a sterile cotton-tipped applicator.
Varicella disciform keratitis (keratouveitis) resembles the disciform keratitis of herpes simplex and herpes zoster, but it generally lasts for a shorter time (2 to 5 months for varicella versus 5 to 10 months for herpes simplex disciform keratitis or more than 1 year for herpes zoster disciform keratitis).7,32 Varicella disciform keratitis is the mildest of the viral disciform keratitides and leads to less corneal scarring.7,32 Viral disciform keratitis is caused by sterile, immunologic reactions to viral antigen that has been retained in the corneal stroma, following prior replication of live virus in the corneal epithelium.42 Varicella disciform keratitis can be treated with topical corticosteroids, but such therapy poses steroid-related risks such as secondary infection, corneal melting, glaucoma, cataract, and prolongation of the disease. If possible, avoid topical steroids and allow the disciform keratitis to run its natural course with supportive therapy such as topical antibiotics and cycloplegics, lubricants, hypertonic agents.
Late, and presumably immunologic, manifestations of varicella, such as chorioretinitis and optic neuritis, may be treated with systemic corticosteroids. This strategy should be avoided during the early stages of systemic varicella because widespread viral dissemination can occur.6
Varicella keratitis, unlike herpes simplex keratitis, tends not to recur. Childhood varicella infection can recur later in life as herpes zoster.
HERPES ZOSTER OPHTHALMICUS
EPIDEMIOLOGY
The term herpes zoster derives from the Greek words herpein, meaning “to creep or to spread,” and zoster, which means “a girdle, sword, belt, or zone,” applied because of the belt-like dermatomal distribution of the disease. When there is involvement of the ophthalmic branch of the trigeminal nerve, the term herpes zoster ophthalmicus (HZO) is used. In 1818, Mahlis reported that the cutaneous eruption of herpes zoster followed the distribution of nerves, but it remained for Hutchinson in 1865 to describe HZO in detail and to report on several cases.43,44
Herpes zoster causes approximately 1% of all skin disease, and most commonly affects the dermatomal distributions of the thoracic (56%) and trigeminal nerves (15%).45 In aggregate, the thoracic dermatomes are the most common areas involved in herpes zoster, but the trigeminal nerve is the single most common dermatomal site. Herpes zoster is four to five times more common in patients who have been immunocompromised by malignancy or immunosuppressive therapy than in those who have not, however, most patients with herpes zoster have no underlying systemic disease.46 A retrospective study of 1000 patients with HZO found that only 12 patients (1.2%) presented either with a malignancy or in an immunocompromised state. No new examples of malignancy or immunosuppression were found in follow-up evaluations.47 For 15 years, Ragozzino and co-workers48 followed prospectively 590 patients with herpes zoster who did not have underlying malignancy. They found that: (1) 9.3% had trigeminal nerve involvement; (2) there was an equal incidence of herpes zoster between male and female patients; (3) there was a relatively low incidence of malignancy (1.1% per year, which is similar to the normal population); and (4) the average annual incidence rate was 1.3 per 1000 person–years. HZO does not appear to be more prevalent in a particular race or gender, but it does seem to have a predilection for elderly patients, who are also more likely to develop other systemic complications from the disease.
Herpes zoster nearly always occurs in patients who have had previous exposure to VZV (chickenpox). Two theories have been proposed to explain the adult form of VZV infection, namely the latency theory and the theory of altered immunity with reinfection.
The latency theory states that after an initial VZV infection the virus remains latent in one or more dorsal root ganglia.3,17 Later in life and as a function of T-cell alterations, varicella reappears from the nerve root ganglion as herpes zoster, in a specific dermatomal area and not in a diffuse cutaneous distribution.3,17,48 This so-called secondary (or symptomatic) zoster occurs in patients in whom the host-parasite relationship to latent VZV has been altered by age, trauma, systemic disease, surgery, or iatrogenic immunosuppression.16 There is a decrease in VZV-neutralizing antibody preceding this event.7,49,15
Herpes zoster may also develop in immunocompetent patients who harbor the latent virus and who are re-exposed to it, by contact with someone who has an active varicella or zoster infection (so-called primary, spontaneous, or infectious zoster).16,50,51 This is the theory of altered immunity with reinfection, but it is not known whether reactivation or fresh exogenous infection by VZV is the cause.16,51,52
Age is the most common predisposing factor to herpes zoster, probably as a result of alterations in T cells and a decrease in neutralizing VZV antibody associated with senescence, allowing reactivation of latent virus.16 Herpes zoster occurs most commonly in the fifth to seventh decades of life; however, some patients with zoster are younger, have a history of recent exposure to someone with active varicella or zoster, and have not had serious predisposing underlying systemic disease.7,8
PATHOGENESIS AND HISTOPATHOLOGY
After primary VZV infection, the virus becomes latent within one or more sensory nerve root ganglia and later reactivates in association with age, immunocompromised state or trauma to the involved ganglion.7,17,52 Other presumed triggers include tuberculosis, syphilis, radiation therapy, and systemic corticosteroid use.16 Viral proliferation in the nerve root ganglion causes inflammation and tissue destruction.
Some of the ophthalmic sequelae of zoster are the result of chronic inflammation and ischemia secondary to vasculitis.53 The inflammatory reaction can be granulomatous or diffusely lymphocytic.53,54,55 Granulomatous intracranial arteritis is a specific complication of HZO.53,54,55
Inflammatory sequelae may also be caused by direct viral infection. VZV has been identified in sensory neural ganglia and has been recovered from the skin and corneal surface during the early stages of zoster.53,55,56 The duration of VZV DNA detection on the ocular surface from rash onset varies from 2 to 34 days.57 Live intraocular VZV has been recovered in a case of acute retinal necrosis syndrome reported by Culbertson and co-workers.58 Herpes zoster–like particles have been found in the retina and in the iris as well.59,60
CLINICAL CHARACTERISTICS
Dermatomal Considerations
The first (ophthalmic) division of the trigeminal nerve is most frequently involved in HZO, 20 times more often than the second (maxillary) or third (mandibular) divisions.16 The predilection of VZV for the ophthalmic division may result from trauma (leading to virus reactivation) or because the localization of herpes simplex virus in the portions of the ganglion that supply the maxillary and mandibular branches has an interference effect against later-acquired VZV.16 HSV preferentially resides in those portions of the ganglion that supply the upper and lower lid, whereas VZV more commonly resides in the portion that supplies the upper lid and nasociliary branch of the trigeminal nerve—usually a sign of dissemination in an immunocompromised host. The diagnosis of HZO is applied if the area of distribution of the ophthalmic division of the trigeminal nerve is involved, even if the globe itself is not inflamed.7
The ophthalmic division of the trigeminal nerve has three parts: the frontal nerve, the lacrimal nerve, and the nasociliary nerve (Fig. 3). The supraorbital and supratrochlear branches of the frontal nerve supply the upper lid and forehead and are most often involved in HZO. The nasociliary nerve provides sensory innervation to the cornea, ciliary body, iris, and conjunctiva. Its terminal branch is the anterior ethmoidal nerve, which innervates the sides of the tip of the nose (alae nasae) via the external nasal nerve.
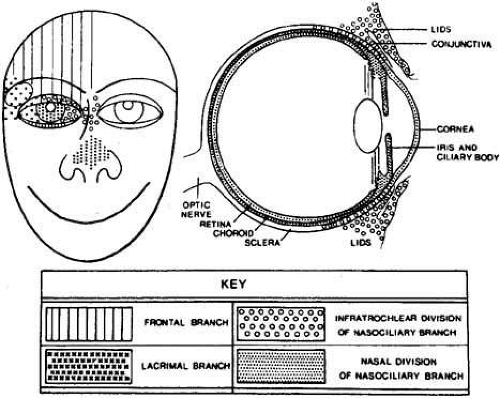 Fig. 3 Distribution of the major branches of first division of trigeminal nerve (cranial nerve V). (Courtesy of Pavan-Langston D Herpes Zoster Ophthalmicus: Int Ophthalmol Clin 10(4): 174, 1975) |
Hutchinson43 was the first to observe that ocular involvement is much more common in herpes zoster patients who had VZV involvement of the nasociliary branch of the trigeminal nerve. The classic Hutchinson’s sign of cutaneous VZV involvement on the alae nasae, that is, the side of the tip of the nose (and not just the tip of the nose), is evidence of nasociliary nerve involvement. Ocular sequelae occur in 50% to 85% of such cases.16 It is important to remember, however, that the eye may be seriously affected in half of all cases, even if Hutchinson’s sign is absent (Fig. 4). Thus, Hutchinson’s sign is not entirely reliable as a predictor of ocular involvement; however, if present, ocular inflammation is more likely to occur.
 Fig. 4 Severe eruption of herpes zoster ophthalmicus with cutaneous necrosis and sloughing. Involvement of the upper lid and sparing of the lower lid is evident. |
HZO begins with a prodrome of severe burning or lancinating pain, dysesthesia or hyperesthesia over the affected dermatome, mild fever, nausea, and malaise (Fig. 5). The preeruptive pain may be insidious. At this stage, the cerebrospinal fluid shows a mild lymphocytic pleocytosis. A cutaneous eruption usually appears over one dermatomal area 3 to 5 days after the onset of pain (Figs. 6 and 7). The erythema and swelling may be mistaken for an insect bite or cellulitis. Initially, the HZO eruption is erythematous and maculopapular, but soon becomes vesiculopapular, ulcerative, and eventually cicatrizing. Material in the vesiculopapular eruption is at first clear, but becomes yellow-brown and purulent as the vesicles erupt and crust. Because VZV involves the dermis, cutaneous scarring, sloughing, and subsequent exposure and superinfection can occur (Figs. 8 and 9). Herpes zoster without cutaneous eruption, called zoster sine herpete or zoster sine eruptione, has been observed. Schwab61 reported 16 patients with zoster sine herpete, in whom an anterior uveitis or iridocyclitis was present without ipsilateral skin lesions; in 9 of these 16 cases there was a documented rise and fall in VZV titers.
 Fig. 5 Herpes zoster ophthalmicus (HZO). Preeruptive phase of HZO, 2 days before cutaneous vesiculation. |
 Fig. 6 Herpes zoster ophthalmicus. Same patient as in Figure 5, 1 day before cutaneous eruption. There is mild scleral injection as well as upper lid vesicles. |
 Fig. 7 Herpes zoster ophthalmicus. Same patient as in Figure 5. Severe hemorrhagic cutaneous eruption and involvement of the side of the tip of the nose (positive Hutchinson’s sign). Note the presence of secondary contralateral eyelid edema (this is not dissemination). |
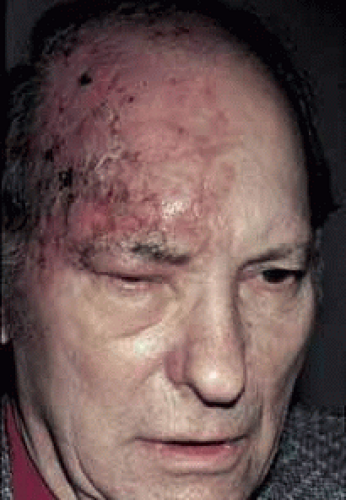 Fig. 8 Herpes zoster ophthalmicus. Initial crusting of vesicles in a 60-year-old white man, 1 week posteruption. |
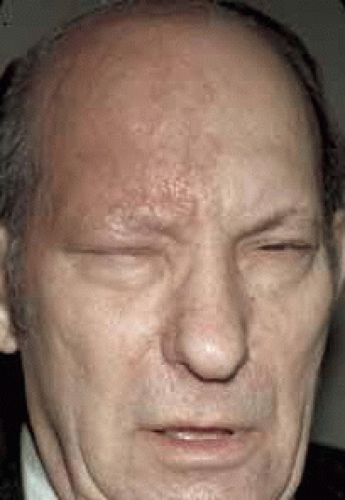 Fig. 9 Herpes zoster ophthalmicus. Same patient as in Figure 8. Prominent scarring 3 months posteruption. |
Edema and vesicular cutaneous eruption of the lower eyelid in HZO do not necessarily indicate involvement of the maxillary division of the trigeminal nerve but may just represent local sequela of frontal nerve involvement. The infratrochlear branch of the nasociliary nerve supplies the medial aspect of the lower lid and conjunctiva. Therefore, VZV vesicles can erupt along the medial aspect of the lower lid margin as a result of involvement of the ophthalmic division of the nerve. Similarly, contralateral eyelid edema is not usually a sign of dissemination, but a local consequence of intense inflammation and swelling on the involved side (see Fig. 7).
The cutaneous eruption of herpes zoster usually follows classic dermatomal patterns, but vesicular eruption may occur several millimeters outside a particular dermatomal distribution and still not signify dissemination.7 True herpes zoster dissemination is defined by involvement of two or more noncontiguous dermatomes. Multiple crops of vesicles in more than one noncontiguous dermatome are almost always a sign of an immunocompromised state, and the patient should be appropriately evaluated (see “Systemic Work-Up” section).
Ocular Involvement
A convenient categorization is to define the ophthalmic manifestations of HZO anatomically. All ocular and adnexal tissues can be affected by herpes zoster inflammation (Table 1). HZO can cause blepharitis, canaliculitis, conjunctivitis, dacryoadenitis, keratitis, keratouveitis, iridocyclitis, vitritis, retinitis, acute retinal necrosis, retinal vasculitis, choroiditis, inflammatory glaucoma, optic neuritis, meningeal encephalitis, inflammatory extraocular muscle palsies, anterior segment ischemia, episcleritis, scleritis, postherpetic neuralgia (PHN), and cephalalgia. Secondary cataract can result from uveitis or prolonged topical or systemic corticosteroid therapy. Ocular sequelae can occur immediately, a few weeks later, or seemingly idiopathically months to years after the cutaneous eruption. It is imperative for the clinician to ask about a prior history of herpes zoster or “shingles” in any patient with chronic inflammatory eye disease.
TABLE 1. Ocular Involvement in Herpes Zoster Ophthalmicus | ||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
|
LIDS AND LASHES.
During the active vesiculoulcerative cutaneous disease, VZV can usually be cultured from skin lesions (see “Laboratory Evaluation” section). Zoster dermal involvement can cause cutaneous sloughing and secondary infection, usually from Staphylococcus aureus or Streptococcus species.16 The pain and hyperesthesia of the eyelid skin may be so intense during the first 3 to 5 days of cutaneous eruption that it may be impossible to examine the conjunctiva, cornea, or internal eye (see Fig. 7). Eyelid involvement can be lead to permanent scar formation, cicatricial ectropion or entropion, trichiasis, eyelash whitening (poliosis), eyelash loss (madarosis), or even frank loss of eyelid tissue. Chronic contracted eyelid scars may occur. Zoster scarring of the lacrimal punctum can cause punctal stenosis and epiphora.
The skin vesicles and ulcerations are virologically sterile after 5 to 7 days and heal within 2 or 3 weeks. Occasionally these lesions require several months to heal totally as a result of secondary bacterial infection or an allergic contact dermatitis caused by topical medication.7
Dysesthesia, hyperesthesia, and pain are common throughout the distribution of the cutaneous eruption, especially in the elderly. PHN may be mild, moderate, severe, or occasionally incapacitating (see “Neurologic Involvement” section).
Hemorrhagic complications may occur, especially in patients who have underlying hematopoietic diseases (e.g., thrombocytopenia, anemia) (see Fig. 7) in association with the cutaneous crisis. Subdural, subarachnoid, and intracranial hematomas have been described in herpes zoster patients taking anticoagulant medications concurrent with the onset of the herpes zoster skin eruption.26
CONJUNCTIVA
Herpes zoster conjunctivitis can manifest as papillary, pseudomembranous, membranous, or follicular. Transitory nonulcerative vesicles, hemorrhages, and conjunctival cicatrization may occur.16 Conjunctival cytology reveals mostly a mononuclear and lymphocytic infiltration, but polymorphonuclear leukocytes can be found in severe cicatrizing membranous forms of the disease, even in the absence of microbial superinfection. After the occurrence of pseudomembranous, membranous, or vesicular types of conjunctivitis, chronic scarring and symblepharon formation can occasionally ensue.16
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


