8 Uveitis
Pathophysiology
Inflammatory reaction
Anterior uveitis
Inflammation of iris (iritis) and ciliary body (cyclitis)
Most common cause of anterior uveitis in adults is idiopathic (followed by HLA-B27 associated)
Most common cause of acute, noninfectious, hypopyon iritis is HLA-B27-associated iritis
Etiology
Classification
Findings
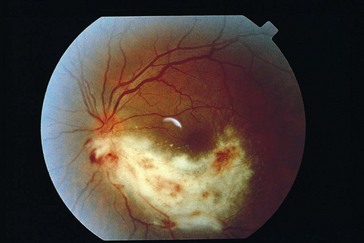
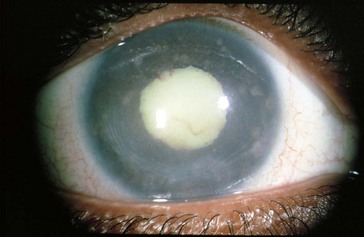
conjunctival and episcleral injection, ciliary injection (circumcorneal flush from branches of anterior ciliary arteries), miosis (iris sphincter spasm), AC reaction; may have hypopyon, keratic precipitates, iris nodules, dilated iris vessels (occasionally, rubeosis), synechiae (posterior [iris adhesions to lens; seclusio pupillae is a complete adhesion that can result in iris bombe] or anterior [iris adhesions to cornea and angle]) (Figure 8-1)

Figure 8-1 Severe idiopathic anterior uveitis with fibrinoid reaction.
(From Hooper PL: Idiopathic and other anterior uveitis. In Yanoff M, Duker JS [eds]: Ophthalmology, London, Mosby, 1999.)
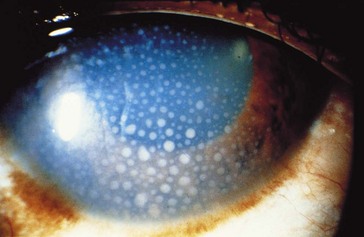
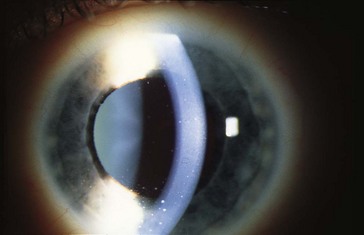
Figure 8-2 Keratic precipitates in anterior uveitis.
(From Forster DJ: General approach to the uveitis patient and treatment strategies. In Yanoff M, Duker JS [eds]: Ophthalmology, London, Mosby, 1999.)
Diagnosis
Treatment
topical steroids, cycloplegic; may require systemic steroids, immunosuppressive agents, antibiotics
Reiter’s Syndrome
Triad of conjunctivitis, urethritis, and arthritis
Associated with infections: Chlamydia, Ureaplasma urealyticum, Yersinia, Shigella, Salmonella
Psoriatic Arthritis
Associated with HLA-B17 and HLA-B27
Uveitis does not occur in psoriasis without arthritis
Inflammatory Bowel Disease (IBD)
Uveitis occurs in ulcerative colitis (10%) and Crohn’s disease (3%)
Fuchs’ Heterochromic Iridocyclitis
Occurs in young adults; unilateral
Associated with chorioretinal scars (toxo)
Findings
diffuse small white stellate KP, minimal AC reaction, no posterior synechiae, iris heterochromia (diffuse atrophy of stroma, loss of iris crypts; involved iris is paler; 15% bilateral), fine-angle vessels (may bleed during gonioscopy, cataract surgery, or paracentesis) (Figure 8-4)
Lyme Disease
Due to Borrelia burgdorferi (spirochete)
Ocular involvement is usually bilateral
Affected organ systems: skin, CNS, cardiovascular, musculoskeletal
Posner-Schlossman Syndrome (Glaucomatocyclitic Crisis)
Recurrent anterior uveitis and increased IOP; episodes are typically self-limited
Phacoanaphylactic Endophthalmitis
May develop severe uveitis with hypotony, secondary open-angle glaucoma
Intermediate uveitis
Pars Planitis
Most common cause of intermediate uveitis (85–90%)
Usually young adults; females > males; 75% bilateral
Accounts for 25% of uveitis in children
Associated with HLA-DR15 and MS
Findings
light flare with a few KP, anterior vitritis, snowballs (white vitreous cellular aggregates near ora serrata; may coalesce to form peripheral fibrovascular accumulation [snowbank] over inferior pars plana and vitreous base), peripheral retinal periphlebitis, hyperemic disc, no chorioretinitis, no synechiae (Figure 8-5)
Posterior uveitis
Most common cause of posterior uveitis in adults is toxoplasmosis (followed by retinal vasculitis)
Infections
Cytomegalovirus (CMV)
Progressive hemorrhagic necrotizing retinitis involving all retinal layers
Occurs in 15–46% of AIDS patients; usually when CD4 count <50 cells/mm3
Rare syndrome of neonatal cytomegalic inclusion disease
Findings
well-circumscribed necrotizing retinitis (2 appearances), mild AC and vitreous reaction
Treatment
antiviral therapy (induction during first 2 weeks)
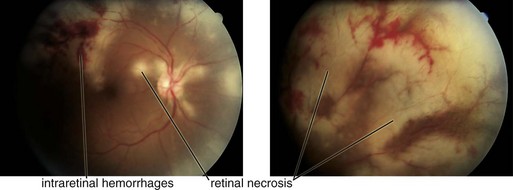
Acute Retinal Necrosis (ARN)
Usually occurs in immunocompetent individuals; 33% bilateral (BARN), commonly in immunosuppressed
Association with HLA-DQw7 (50%)
Findings
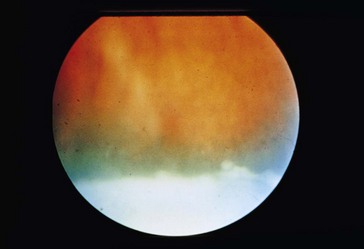
diffuse episcleral injection, mild iritis with granulomatous KP, vitritis; ‘thumbprint’ nummular infiltrates posterior to equator with isolated peripheral patches of necrotizing retinitis that becomes confluent; sawtooth demarcation line between necrotic and healthy retina, generalized obliterative retinal arteritis (with peripheral vaso-occlusion), pale disc edema (Figure 8-7); within 2 months, retinitis gradually resolves and necrotic retina sloughs; coarse salt and pepper pigmentation
Progressive Outer Retinal Necrosis (PORN)
Variant of ARN in AIDS but painless with minimal intraocular inflammation
Often have history of cutaneous zoster
74% unilateral at presentation, 70% become bilateral
Findings: multiple discrete peripheral or central areas of retinal opacification/infiltrates (deep with very rapid progression), ‘cracked mud’ appearance after resolution; vasculitis is not prominent (Figure 8-8)
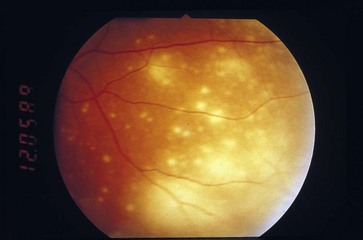
Figure 8-8 Progressive outer retinal necrosis, early stage.
(From Hudson HL, Boyer DS, Martin DF, et al: Viral posterior uveitis. In Yanoff M, Duker JS [eds]: Ophthalmology, London, Mosby, 1999.)
Treatment: combination of foscarnet and ganciclovir; poor response to antivirals
 with exacerbations)
with exacerbations)