Purpose
To describe the ultrasound biomicroscopy (UBM) findings of the ciliary body in patients with ocular/oculodermal melanocytosis.
Design
Retrospective observational case series study.
Methods
A retrospective chart and imaging database review was conducted for patients with unilateral ocular/oculodermal melanocytosis who underwent UBM examination at the Ocular Oncology Clinic of Princess Margaret Hospital. Radial images of the ciliary body at the 3-, 6-, 9-, and 12-o’clock positions were obtained in both eyes. UBM characteristics included ciliary body thickness and reflectivity. The eye with ocular/oculodermal melanocytosis was compared with the contralateral unaffected eye as a control. Statistical significance was analyzed with Student t test.
Results
Twelve patients were included. All patients showed unilateral diffuse pigmentation involving episclera and anterior chamber angle. The iris showed diffuse pigmentation in 10 cases and sectorial in 2. Mean ciliary body thickness of the affected eyes was 0.581 ± 0.058 mm (range 0.489-0.744) compared with 0.475 ± 0.048 mm (range 0.406-0.622) in the contralateral eye, which was found to be a statistically significant difference ( P < .001). The affected ciliary body showed hyperreflectivity when compared with the unaffected eye. All affected eyes were graded as medium to high reflectivity compared with the unaffected eyes that showed a medium to medium/low reflectivity.
Conclusion
Ciliary body involvement in ocular/oculodermal melanocytosis presents as increased thickness and higher ultrasound reflectivity on UBM when compared with the unaffected eye. UBM is helpful in imaging clinically undetectable areas of melanocytosis involving the ciliary body.
Ocular melanocytosis is a congenital hyperplasia of melanocytes in ocular tissues. Oculodermal melanocytosis or nevus of Ota was first described by Ota and Tanino in 1939. It is a congenital hamartoma of dermal melanocytes involving the ophthalmic and maxillary divisions of the trigeminal nerve, producing blue to brown pigmentation along their dermatomal distribution, which also involves the ipsilateral ocular and orbital tissues, and cerebral meninges. The etiology and pathogenesis of oculodermal melanocytosis is unknown. It is postulated that oculodermal melanocytosis and other dermal melanocytic disorders may result from incomplete migration of melanocytes from the neural crest to the epidermis during embryonic life. Both ocular and oculodermal melanocytosis have been previously encompassed as a single entity, since they have the same ocular features and carry the same risks in ocular tissues. These patients are at higher risk to develop uveal melanoma and pigmentary glaucoma. It has been estimated that 1 in 400 white patients with ocular/oculodermal melanocytosis will develop uveal melanoma in their life, hence the importance of periodic surveillance for early melanoma development in ocular tissues involved with melanocytosis. Ciliary body evaluation represents a special challenge, since its location impedes direct visualization by the clinician. Ultrasound biomicroscopy (UBM) has been widely used in imaging anterior segment structures, and provides the most useful way of evaluating the ciliary body. In this report we evaluate the UBM features of ocular/oculodermal melanocytosis and its role in detecting clinically occult areas of melanocytosis involving the ciliary body.
Methods
In a retrospective observational case series study, an electronic chart and imaging database review was conducted for all patients with unilateral ocular/oculodermal melanocytosis who underwent UBM examination at the Ocular Oncology Clinic of Princess Margaret Hospital, Toronto, Canada, between July 1, 2008 and November 30, 2011. Institutional review board approval for this retrospective review of patient data was prospectively obtained from the Cancer Registry of Canada and Research Ethics Board of the Princess Margaret Hospital/University Health Network.
All patients evaluated for ocular/oculodermal melanocytosis in the clinic during the specified years underwent a comprehensive ophthalmic examination including UBM scanning of both the affected and unaffected eye.
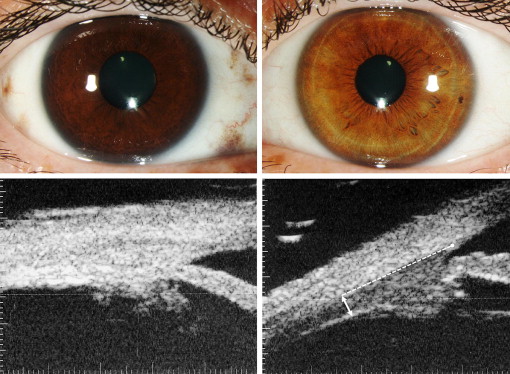
Patient demographics included age, race, and sex. Clinical data included dermal pigmentation involvement, laterality, scleral involvement of melanocytosis in quadrants, iris heterochromia (including monocular sectorial heterochromia), angle pigmentation, fundus heterochromia, and associated malignancies if present. Anterior segment clinical images were obtained for all patients. High-resolution ultrasonographic imaging of the ciliary body was performed using the commercial version of the UBM with a 50-MHz transducer (Humphrey Instruments, San Leandro, California, USA) at a standard gain of 80 dB for all scans. Radial imaging of the ciliary body at the 3-, 6-, 9-, and 12-o’clock positions was obtained in both eyes (affected and unaffected). UBM characteristics included measurements of the ciliary body thickness and internal reflectivity. Measurements of the ciliary body thickness were electronically calculated using digital calipers, using GIMP Software ( www.gimp.org ). The vertical ciliary body thickness was measured just posterior to the junction of the pars plana and pars plicata at a point located 2.5 mm posterior to the scleral spur ( Figure 1 , Bottom right). This position was selected to avoid the ciliary processes thickness variability. All scans were individually measured by the same person (J.P.V.M.). Internal reflectivity is a qualitative measurement that compares the intensity of the sound returning to the probe within a structure, in this case the ciliary body. All scans were individually evaluated by the senior author (C.J.P.) and were graded on a 5-point scale (low, medium/low, medium, medium/high, and high). In UBM imaging, a tissue with high internal reflectivity would be the sclera and one with low internal reflectivity would be the cornea. UBM characteristics in the eye with ocular/oculodermal melanocytosis were compared with the contralateral unaffected eye as a control in all cases. Statistical significance of the mean differences in thickness of the ciliary body between both eyes was analyzed with Student t test.
One patient (Case 10) presented with a large choroidal melanoma without ciliary body involvement in the eye with ocular melanocytosis, and was treated with enucleation. Pathologic microscopic images of the ciliary body were obtained and compared with the ultrasound biomicroscopic image in the same region.
Results
Inclusion criteria matched 12 patients, 5 male and 7 female, with 7 right eyes and 5 left eyes affected. Median age at first evaluation was 45.5 years (range 29-71). Nine patients were white and 3 Asian. Four patients presented with choroidal melanoma in the initial visit and 2 developed choroidal melanoma during follow-up. Seven patients (58.3%) presented with ocular melanocytosis and 5 (41.7%) with oculodermal melanocytosis. None of the cases was associated with pigmentary glaucoma or other systemic relevant diseases.
All patients showed unilateral diffuse pigmentation involving the episclera and anterior chamber angle. Eleven patients (91%) presented with fundus heterochromia and 1 patient (Case 1) showed normal fundus pigmentation in both eyes. The iris showed diffuse pigmentation in 10 cases and monocular sectorial iris heterochromia presented in 2 patients. Iris in the unaffected eye was brown in 6 patients and green in 5 patients, and only 1 patient had a blue iris. Table 1 shows distribution of pigment in all cases.
| Case | Cutaneous Involvement | Episcleral Involvement (Quadrants) | Iris Involvement (Quadrants) | Involved Iris Color | Angle Involvement (Quadrants) | Fundus Heterochromia |
|---|---|---|---|---|---|---|
| 1 | No | 1 | 2 | Dark brown | 2 | No |
| 2 | No | 3 | 3 | Dark brown | 3 | Yes |
| 3 | Yes | 4 | 4 | Dark brown | 4 | Yes |
| 4 | Yes | 4 | 4 | Dark brown | 4 | Yes |
| 5 | Yes | 3 | 4 | Dark brown | 4 | Yes |
| 6 | Yes | 4 | 4 | Light brown | 4 | Yes |
| 7 | No | 2 | 4 | Dark brown | 4 | Yes |
| 8 | No | 4 | 4 | Dark green | 4 | Yes |
| 9 | No | 4 | 4 | Blue/brown | 4 | Yes |
| 10 | No | 4 | 4 | Dark green | 4 | Yes |
| 11 | No | 4 | 4 | Dark brown | 4 | Yes |
| 12 | Yes | 4 | 4 | Dark brown | 4 | Yes |
Mean thickness of the ciliary body of the affected eyes for all patients was 0.581 ± 0.058 mm (range 0.489-0.744) compared with 0.475 ± 0.048 (range 0.406-0.622) in the contralateral eye. The difference in the mean thickness between the affected eyes and the contralateral unaffected eyes was found to be statistically significant ( P < .001). Each case was also individually evaluated and all cases were found to have statistically significant differences between the affected and the contralateral unaffected eye ( P < .05) ( Table 2 ).
| Case | Quadrants of Involvement | Involved Eye CB Thickness, mm (SD) | Contralateral Eye CB Thickness, mm (SD) | P Value |
|---|---|---|---|---|
| 1 | 2 | 0.626 (±0.016) a | 0.462 (±0.058) | .01 b |
| 2 | 3 | 0.588 (±0.032) a | 0.494 (±0.020) | .002 b |
| 3 | 4 | 0.544 (±0.043) | 0.434 (±0.032) | .001 b |
| 4 | 4 | 0.586 (±0.030) | 0.453 (±0.050) | .01 b |
| 5 | 4 | 0.651 (±0.084) | 0.537 (±0.066) | .04 b |
| 6 | 4 | 0.595 (±0.093) | 0.447 (±0.023) | .02 b |
| 7 | 4 | 0.602 (±0.042) | 0.474 (±0.061) | .01 b |
| 8 | 4 | 0.583 (±0.058) | 0.523 (±0.040) | .01 b |
| 9 | 4 | 0.577 (±0.052) | 0.482 (±0.041) | .04 b |
| 10 | 4 | 0.573 (±0.078) | 0.478 (±0.040) | .03 b |
| 11 | 4 | 0.523 (±0.017) | 0.473 (±0.029) | .01 b |
| 12 | 4 | 0.557 (±0.029) | 0.449 (±0.034) | .002 b |
| Overall | 0.581 (±0.058) | 0.475 (±0.048) | <.001 b |
a Only affected sectors included.
The ciliary body of eyes with ocular/oculodermal melanocytosis showed hyperreflectivity on UBM imaging when compared with the contralateral unaffected eye ( Figure 1 ) in all patients. Individual reflectivity evaluated by clock-hour position is summarized in the Supplemental Table (available at AJO.com ). All affected eyes were graded as medium to high internal reflectivity compared with the unaffected eyes, which showed a medium to medium/low reflectivity.
Cases 1 and 2 presented sectorial involvement. The difference in thickness between the affected and nonaffected sectors in the same eye was found to be statistically significant in both cases ( P = .004 for Case 1 and P = .02 for Case 2). Furthermore, comparing the nonaffected sector in the involved eye with the uninvolved eye, we found no statistically significant difference ( P = .1 for both cases). Also, the affected sectors were classified with a medium/high to high reflectivity in the affected sectors compared with a medium reflectivity in the unaffected sectors in the same eye ( Figure 2 ).

Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


