The placement of tympanostomy tubes (TT) is a well-established procedure in most otolaryngology practices. The relative indications, although still debated, are generally accepted to include recurrent acute otitis media affecting the quality of life of the patient and persistent hearing loss due to otitis media with effusion affecting development. Other considerations for the use of TT are the delivery of intratympanic medications, management of the complications of acute otitis media, and the relief of symptoms resulting from tympanic barotrauma (especially air travel).
Each year in the United States more than 600,000 children under the age of 15 years have TT inserted under a general anaesthesia.1 This procedure has consistently been proven to be effective and safe. However, because of the frequency of TT insertion, complications of their use are encountered in most practices. The purpose of this chapter is to illustrate some key points regarding the choice of tube, special circumstances of use, and management of complications of TT insertion.
19.2 Materials, Tube Design, and Flange Design
The number and type of TT on the market is overwhelming, with a variety of manufacturers making multiple tubes with varying sizes and materials. A synopsis of all TT is beyond the scope of this chapter. Rather, an overview of the types of TT is provided so the otolaryngologist can make a more considered choice and tailor TT use to the specific clinical scenario.
19.2.1 Materials
TT materials can be divided into plastics and metals. All materials in TT have the common characteristics of being biocompatible and smooth, which reduces but does not prevent biofilm formation. The following section provides a brief description of the common materials used and the advantages of each product.
Plastics
Polyethylene
Polyethylene is a thermoplastic polymer consisting of long hydrocarbon chains. The density and melting point is dependent on the type of branching, crystal structure, and molecular weight. The most common type of polyethylene used in medical prosthetics is ultra–high-density polyethylene due to its rigidity and high melting point.
Fluoroplastics
These are a group of plastics that contain carbon and fluorine molecules. The most familiar of these is polytetrafluoroethylene (Teflon) by DuPont (Wilmington, Delaware). Like polyethylene, it is rigid and has a high melting point. It is also nonstick and is thought to help retard biofilm growth.
Silicone
Silicone is an inert polymer with a silicone backbone and organic side groups. It can be synthesized in a variety of consistencies or “durometers” for tubes, from soft to firm. Unlike the other plastics, it is soft. This elasticity makes it easy to compress for insertion and allows removal with minimal discomfort in the clinic setting.
Metals
Stainless Steel
This is a steel alloy with a minimum of 10.5% chromium that is resistant to oxygenation and corrosion. Its stiffness allows easy insertion. Stainless steel has a long history of reliability in medical prosthetics.
Titanium
Titanium is progressively becoming the more common choice for metal tubes given that it is durable, lightweight, corrosion-resistant, and MRI-compatible. Lightweight tubes have been shown to decrease tympanosclerosis.2
Each of the above materials can come with a bacteriostatic coating that is the intellectual property of the manufacturers of TT. Conclusive evidence is lacking regarding increased efficacy of any one coating.
19.2.2 Tube Design
Design is dictated by the internal and external diameter of the tube. Theoretically, the wider the internal diameter, the better the drainage of mucoid effusions and resistance to blockage. This is offset by the risk of contamination of the middle ear from external ear pathogens as the surface tension required to breach the middle ear is reduced. The outer diameter dictates the size of perforation that will remain post-extrusion. In the normal setting of short- to mid-term tube extrusion, even a large diameter will have little consequence; however, over the long term, a larger diameter tube will have a higher perforation rate.
19.2.3 Collar and Flange Design
Most TT feature a collar or a set of flanges that are designed to keep the tube from extruding. The wider the profile of the collar or flanges, the more probability that the TT will remain in situ for a longer period of time. In general, flanges are expected to keep a TT in place longer than a collar. A typical TT with a collar or flange diameter of ≤2.5 mm will, on average, extrude between 8 months and 24 months, whereas a T-shaped TT with wide flanges will typically not extrude before 2 years.2 Using a double or triple flange design also reduces movement of the tube and prevents enlargement of the myringotomy.
19.3 Features of TT for Specific Purposes
Broadly, TT can be divided into short/medium-term tubes and long-term tubes. In general, short-term tubes tend to be smaller and have a collar, whereas long-term tubes are larger and have wide flanges. Because the collar of a short-term tube is only a modest barrier to extrusion, it can be used for temporary ventilation with a high degree of confidence that it will spontaneously extrude and heal. Examples of this include the Bobbin (▶ Fig. 19.1) by Grace Medical, Inc. (Memphis, Tennessee) and the Paparella (▶ Fig. 19.2), also by Grace Medical.

Fig. 19.1 Bobbin tympanostomy tube. This grommet-style tube has two collars that keep the tube in place over the short term.
(Image courtesy of Grace Medical.)

Fig. 19.2 Paparella tympanostomy tube. This short-term tube has two collars and a tab to facilitate removal.
(Image courtesy of Grace Medical.)
Long-term tubes featuring flanges can be divided into those with a long barrel and those with a short barrel. The disadvantages of long-term tubes are that biofilm formation can occur and the flange design can increase the risk of a permanent perforation once extrusion occurs. A common long-term tube with a long barrel that most otolaryngologists would be familiar with is the T-Tube by Grace Medical (▶ Fig. 19.3; ▶ Fig. 19.4). An advantage of the T-Tube is that it can be trimmed in length to the surgeon’s desire. The longer barrel has a greater resistance to water intrusion but has the disadvantages of becoming blocked more frequently, having reduced otological drop penetration, and being more difficult to inspect through the tube into the middle ear. In addition, thick, mucoid effusions that are difficult to evacuate will often not drain effectively through a long-barrel tube, risking occlusion and early extrusion. Hence, short-barrel flanged tubes with a wider internal diameter are preferred if the need for ototopical medication administration or blockage is judged to be high (▶ Fig. 19.5).
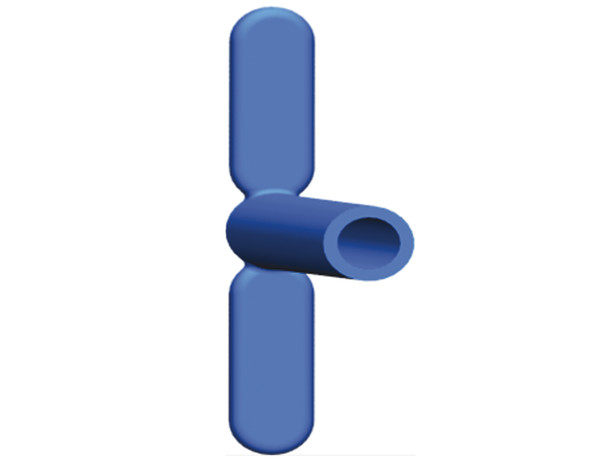
Fig. 19.3 T-Tube tympanostomy tube. This classic long-term tube has a long barrel and two flanges.
(Image courtesy of Grace Medical.)
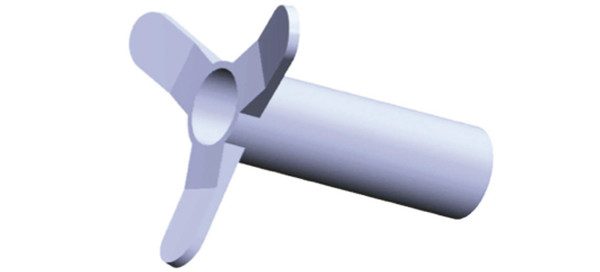
Fig. 19.4 Triune Tube tympanostomy tube. This T-style tube has a long barrel and three short flanges, which are designed to hold the tube in place from a medium to long term.
(Image courtesy of Grace Medical.)

Fig. 19.5 Taper Vent tympanostomy tube. This tube has a short wide barrel and two short flanges, which will keep the tube in place for a medium term. This style of barrel better facilitates entry of ototopical medications compared with traditional T-style tubes.
(Image courtesy of Grace Medical.)
Often the TT selected is based on the preference of the facility that the surgeon attends due to economic or historical reasons. Unfortunately, there is no TT that caters to all scenarios and a one-size-fits-all approach to TT selection will result in inappropriate insertion of TT in specific patients, often with poor results.
19.4 Complications of TT
19.4.1 Early Extrusion/Retention of Tube
Tailoring the correct TT as described above to the correct clinical scenario will help prevent this complication from occurring frequently, but will not prevent it outright. Heaton, Bingham, and Osborne3 demonstrated that tubes placed in the anterior pars tensor had a lower incidence of early extrusion. Bleeding has been shown to increase tube obstruction and extrusion.4 Hence, making the radial incision between the vessels of the tympanic membrane is beneficial. The nature of the middle ear effusion and the number of previous tubes has been shown to influence early extrusion.5 Anecdotally, making the myringotomy only long enough to just allow atraumatic insertion of the TT and avoiding an atrophic tympanic membrane may help to maximize the life of a TT.
19.4.2 Tube Removal
The decision that a TT has been retained for too long is based on the individual patient’s clinical scenario. Traditionally, evidence suggests that a tube that has been in situ for more than 18 months has an increased risk of leaving a perforation.6 In practice, the removal and replacement of a long-term tube is rarely performed on the basis of time alone. Often, a tube will be removed if it is thought to be the nidus of biofilms, myringitis, and recurrent TT otorrhea. More often than not, the decision to remove a TT is based on the fact that the patient no longer requires the tube. Typically, this only has to be carried out for long-term tubes, and the decision is based on symptom-free intervals, normal hearing, age, and the ability to perform the Valsalva maneuver. If the patient can demonstrate resolution of Eustachian tube dysfunction by performing the Valsalva, then the TT is removed.
19.4.3 Perforation
Tube placement can be associated with an inflammatory reaction and secondary development of a fibrous ring around the TT. After extrusion, epithelial cell hyperplasia and migration at the edge of a perforation allow for normal healing, often as a so-called “monomeric” tympanic membrane. Wilson7 suggested that the ingrowth of squamous epithelium onto the undersurface of the tympanic membrane may cause contact inhibition and prevent epithelial hyperplasia and closure of the tympanic perforation. Bingham8 noted the spontaneous closure of a perforation up to 12 months after extrusion and argued that the definition of post-extrusion perforation should be defined as one present at 12 months. Others have defined it as 6 months, making it difficult to quote the actual residual perforation rate. Yum9 quotes a perforation rate of 2.8% at 6 months that can be as high as 16.6% in long-term tubes.10 Apart from the use of long-term tubes, other risk factors for post-extrusion perforation include age >7 years,11 recurrent postoperative otorrhea,12 atrophy of the tympanic membrane,13 and spontaneous extrusion (as opposed to active removal as the edges are freshened in the latter). If the perforation is small, dry and the patient has no desire to dive or join the armed forces, then no intervention may be needed. Tympanoplasty for persistent tube perforations causing concern is covered in Part 4, Roundtable on Tympanic Membrane Reconstruction.
19.4.4 Acute Otitis Media with Tympanostomy (AOMT)
AOMT is a common and separate clinical and microbiological entity to acute otitis media (AOM). AOMT presents with a purulent otorrhea, in contrast to the otalgia, fever, and hearing loss that is expected with AOM without a tube. The microbiological cause of this is typically bacterial, with Streptococcus pneumonia, Haemophilus influenza, Moraxella catarrhalis, Staphylococcus aureus, and Pseudomonas aeruginosa most commonly cultured.14 The mechanism of infection is caused by either influx of bacteria from the external auditory canal or by reflux of contaminated fluid from the nasopharynx up the Eustachian tube. The incidence of AOMT varies but is frequent and ranges from 0.36 to 3.6 episodes/child/year.2 In a systematic review of the literature by Hellström, Groth, and Jörgensen,2 there was no or only slight evidence that water exposure affects otorrhea, and for this reason we do not exclude our patients from water exposure on the basis of preventing AOMT.
The most effective management of AOMT is in the preoperative encounter, with appropriate consenting and education. The importance of educating the patient’s caregiver that TT reduce the frequency, duration, and severity of otitis media but do not eliminate middle ear infections cannot be overstated. Tubes can reduce the duration of otitis media from months to days, allow for the use of topical antibiotics instead of systemic antibiotics,15 and allow the administration of culture-directed antibiotics, if needed, without the need for tympanocentesis.16 In a randomized trial of 270 patients between 1–10 years of age, antibiotics/steroid drops were compared with systemic antibiotics and observation. A significant reduction in time to resolution of otorrhea was observed in the antibiotic/steroid drops group.15 An antibiotic/steroid combination has also been demonstrated to be superior to antibiotics alone.17
19.4.5 Special Circumstances in AOMT
Otorrhea Despite Appropriate Topical Drop Management
Occasional failure of treatment with appropriate ototopical therapy will occur. This most frequently is due to inadequate drop delivery. If the tube is observed to be blocked by keratin debris or crusting, some patients will tolerate clearance of this in the office setting using a micropick or suction. If excessive viscous secretions are the cause of blockage, careful aural toilet is required. Demonstration to parents on how to do this with tissue paper is instrumental. The instillation of drops followed by 5–10 minutes in an ear-dependent position and the use of tragal pumping to help the drops to penetrate may help. Occasionally, the patient will require regular aural toilet and irrigation with warmed sterile saline. At this point, the role that biofilms on the TT may be playing in the ongoing otorrhea needs to be discussed, and TT removal and replacement may need to be considered.
Methicillin-Resistant Staphylococcus Aureus (MRSA) Tube Otorrhea
Swab results showing MRSA are often discovered with trepidation. The most common cause of MRSA colonization of the middle ear is due to repeated use of systemic antibiotics. Hence, the use of further doses of systemic antibiotics in most circumstances is usually not indicated. It is difficult to treat MRSA with systemic antibiotics without also affecting normal flora, which may act as a competitor to MRSA growth. Therefore, the objective of management is control of MRSA, not eradication.
As a first-line treatment, the above advice for all tube otorrhea should be followed. Even in the setting of a report stating resistance to fluoroquinolones, it is this author’s opinion that topical fluoroquinolones with steroid should be considered as first-line medical management.18 Topical antibiotics can have a 1000-fold higher concentration within the middle ear cleft than systemic antibiotics,16 and the minimum inhibitory levels reported do not reflect this high concentration. Often, conventional therapy with drops has already been attempted. If this is the case and proper technique is being demonstrated, then the topical use of mupirocin ointment around the perforation, the promontory, and the ear canal will result in the relief of otorrhea with no ototoxicity, as shown by Furukawa, Minekawa, Haruyama et al.19 In these circumstances, we also recommend treating any other known nidus of MRSA colonization, such as in the nasal cavity, with mupirocin ointment, and to perform chlorhexidine body washing.
If this fails, systemic antibiotic therapy directed by culturing is mandated. Consideration needs to be given to the presence of silent mastoiditis or occult choleasteatoma. Special cultures for mycobacterium should be taken, and immunological screening investigation of systemic causes of middle ear disease and immunodeficiency need to be investigated, as outlined in Chapter 12.
19.5 Long-Term Consequences of Tubes
A 25-year follow-up of a cohort of patients who had a myringotomy in one ear and a tube in the opposite ear conducted by Cayé-Thomasen, Stangerup, Jørgensen, Drozdziewic, and Bonding, 20 demonstrated that myringosclerosis was more frequent (50%) in the tubed ear. Furthermore, it progressed well after the tube had extruded but did not have any clinical effect on audiologic outcomes. In this same study of ears treated for serous otitis media, there was no increase in the incidence of cholesteatoma or other adverse pathology. Retractions increased early but were observed to resolve over time.
19.6 Special Applications of Tympanostomy Tubes in Chronic Ear Disease
19.6.1 Primary T-Tube Cartilage Tympanoplasty
Primary intubation of a cartilage tympanoplasty in the setting of atelectasis was introduced by Hall21 and promoted by Duckert, Makielski, and Helms.22 The latter proposed, in a series of 40 patients, that the union of the cartilage graft and the ventilating tube “offered an attractive option when used simultaneously to reverse atelectasis, reconstruct the tympanic membrane and re-pneumatize the middle ear, so to eliminate recurrent effusion.” We have modified this technique and use the same T-Tube tympanoplasty in a double-island composite graft, as described by Brackman, Shelton, and Arriaga (▶ Fig. 19.6).23 In the experience of Duckert, Makielski, and Helms, they were able to reduce the air-bone gap to <25dB in >80% of patients in the early stages of follow-up. They also experienced no post-extubation perforations and no epithelial ingrowth. Sixty-five percent of patients retained their T-Tube for over 4 years. They did report 7 out of 40 patients having tube otorrhea. Keeping in mind that this technique is reserved for those high-risk ears resistant to traditional therapy, we believe this to be a good result. We also experience episodic otorrhea with this technique and address this in exactly the same manner as described for AOMT, with successful results. Rarely do the tubes need to be removed and replaced.

Fig. 19.6 Intubated cartilage graft. A cartilage graft can be intubated primarily during surgery if there is no ongoing infection or as part of a staged process. Secondary intubation of a cartilage graft can be facilitated by use of a laser.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


