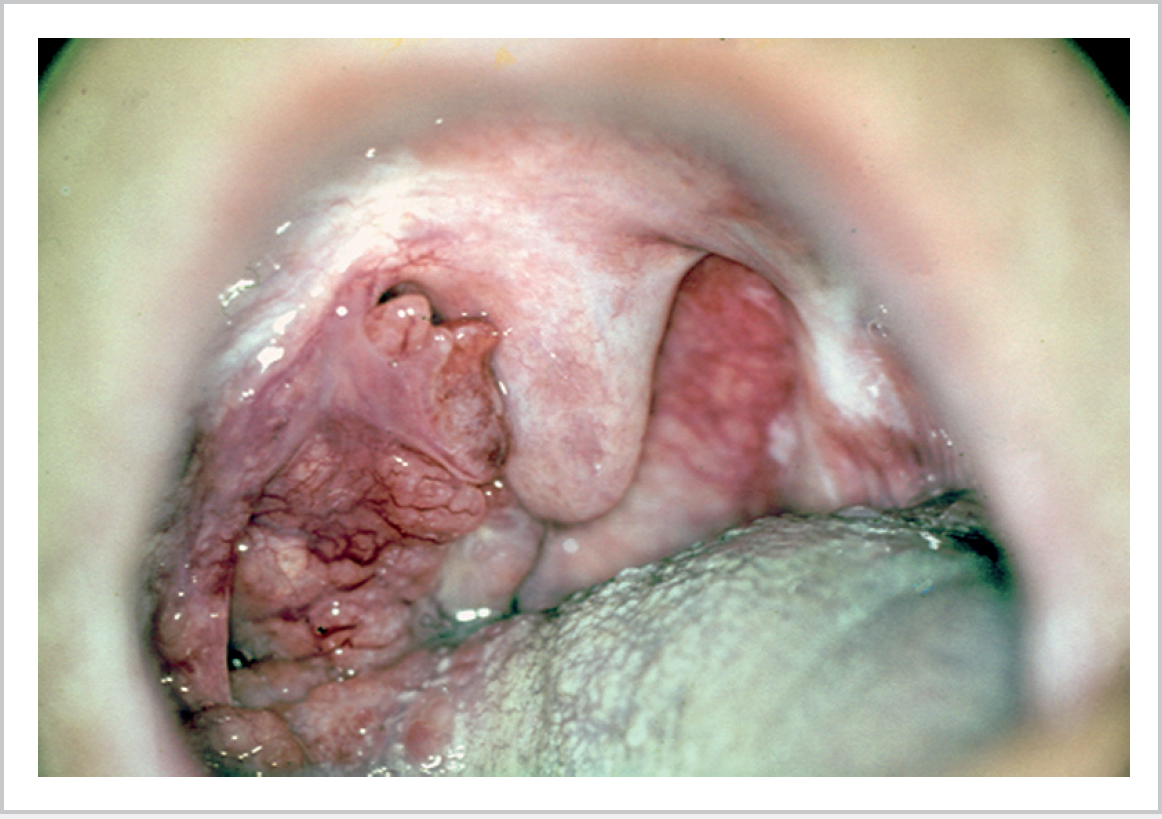
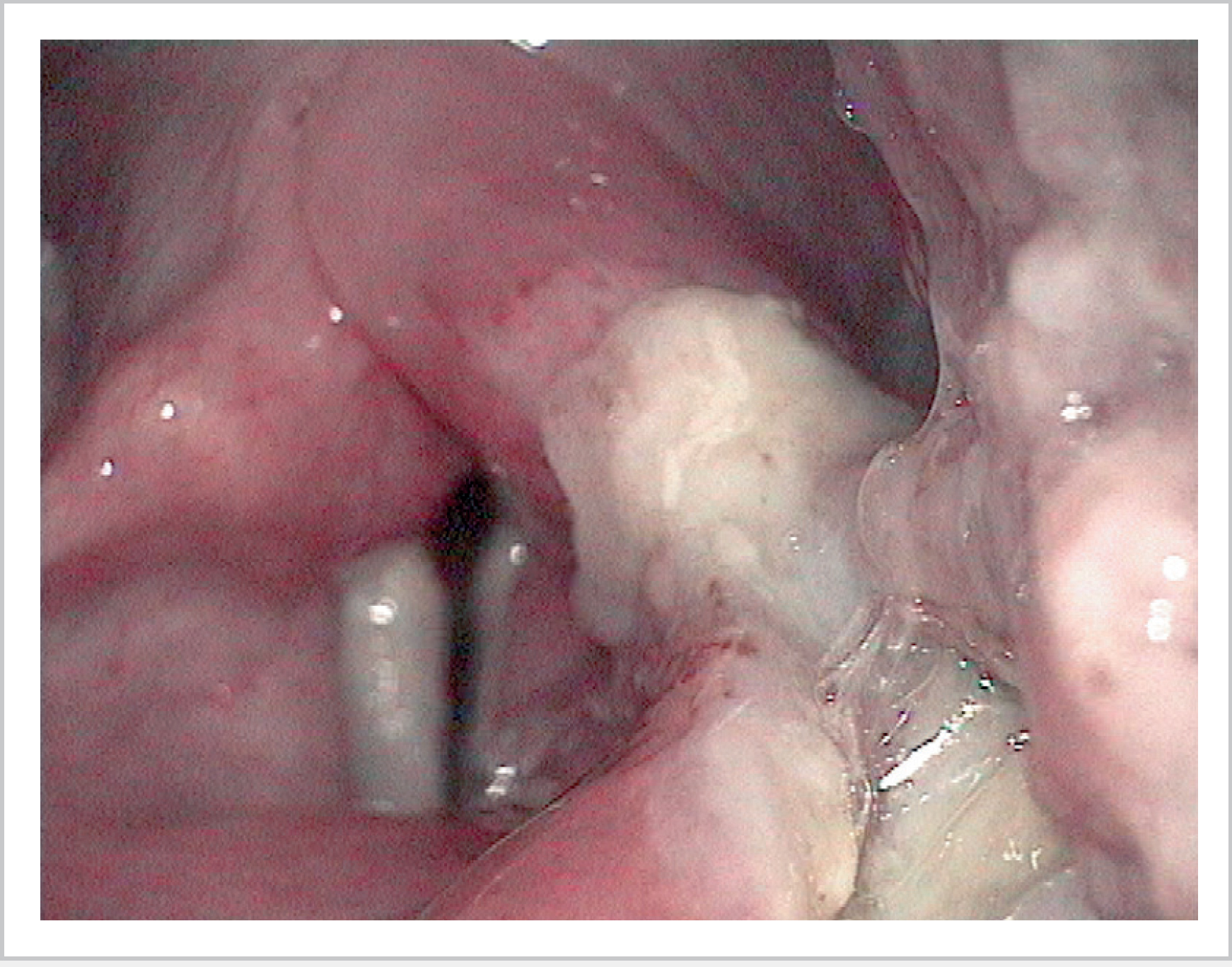
57 Tumours of the Pharynx • Subsites • 2% of all H&N malignancy • 80% SCC • Minor salivary gland tumours (present submucosal) with adenoid cystic most common • Uvular involvement or disease involving midline consider bilateral neck treatment • High rate of occult metastases (20–30%) including retropharyngeal nodes • Velopharyngeal insufficiency with nasal regurgitation can occur following surgical resection • Radiotherapy ± chemotherapy is treatment of choice for most lesions • Post-radiotherapy recurrence and larger tumours surgical treatment includes lip-split, mandibulotomy with preincision plating, floor of mouth incision extending posteriorly, including division of mylohyoid, to gain maximum exposure • Tumour resection with radial forearm free flap reconstruction and covering tracheostomy • Aetiology • SCC most common (Fig. 57.1) followed by lymphoma • Presents with ulceration or asymmetrical tonsil enlargement or lymphadenopathy ± previous presentations • Metastases to neck nodes levels 2 and 3 most common and often cystic (misdiagnosed as branchial cysts) • Trismus indicates pterygoid muscle involvement • Features • Treatment • Staging • Posterior pharyngeal wall—superior level of hyoid bone to inferior border of cricoid • Piriform fossa (Fig. 57.2)—pharyngoepiglottic fold to upper oesophagus • Postcricoid space (Fig. 57.3)—arytenoid cartilages to inferior border of cricoid cartilage
57.1 Oropharynx
 Soft palate—anterior pillar lateral, posterior hard palate, free margin inferior including uvular
Soft palate—anterior pillar lateral, posterior hard palate, free margin inferior including uvular
 Base of tongue—anterior margin is circumvallate papilla, posterior is vallecular
Base of tongue—anterior margin is circumvallate papilla, posterior is vallecular
 Tonsil—most common
Tonsil—most common
57.1.1 Soft Palate
57.1.2 Tonsil
 HPV (better prognosis P16 positive)
HPV (better prognosis P16 positive)
 Smoking
Smoking
57.1.3 Tongue Base
 May present late due to symptoms misinterpreted as infection
May present late due to symptoms misinterpreted as infection
 Submucosal disease may make primary easily missed on examination
Submucosal disease may make primary easily missed on examination
 Palpation of tongue base is vital part of examination and consider general anaesthesia ± biopsy if the gag reflex is too strong but clinically suspicious
Palpation of tongue base is vital part of examination and consider general anaesthesia ± biopsy if the gag reflex is too strong but clinically suspicious
 Can present as metastatic neck disease of unknown primary
Can present as metastatic neck disease of unknown primary
 Need to assess relation to midline and hence whether ipsilateral or bilateral neck requires treatment
Need to assess relation to midline and hence whether ipsilateral or bilateral neck requires treatment
 Surgery, radiotherapy, or chemoradiotherapy
Surgery, radiotherapy, or chemoradiotherapy
 There is a significant impact on speech and swallowing function with all treatment options, particularly with large disease
There is a significant impact on speech and swallowing function with all treatment options, particularly with large disease
 Mandibulotomy for access may be required
Mandibulotomy for access may be required
 Consider supplementary feeding via gastrostomy before or after treatment
Consider supplementary feeding via gastrostomy before or after treatment
 T0: no evidence of primary tumour
T0: no evidence of primary tumour
 T1: tumour ≤ 2 cm
T1: tumour ≤ 2 cm
 T2: tumour 2–4 cm
T2: tumour 2–4 cm
 T3: tumour >4 cm
T3: tumour >4 cm
 T4a: tumour invades adjacent structures, e.g., cortical bone mandible, hard palate, larynx, and deep muscles of tongue
T4a: tumour invades adjacent structures, e.g., cortical bone mandible, hard palate, larynx, and deep muscles of tongue
 T4b: tumour invades lateral pterygoid muscle, pterygoid plates, lateral nasopharynx, skull base, or encases carotid artery
T4b: tumour invades lateral pterygoid muscle, pterygoid plates, lateral nasopharynx, skull base, or encases carotid artery
57.2 Hypopharynx
57.2.1 Subsites
< div class='tao-gold-member'>
![]()
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree