(1)
Narayana Hridayalaya Multispeciality, Bangalore, India
Surgical Anatomy
The nose and paranasal (PNS) sinus have complex anatomy. It is related to various important structures that serve vital functions. It is essential to have clear understanding of the anatomy of this region to adequately address these tumors. The paranasal sinus is a common term used for group of sinuses that drains into the nasal cavities. The maxillary sinus is the largest and the most common to be involved in the pathology. The frontal, ethmoid, and sphenoid sinuses do get involved by pathology occasionally, and this mostly happens due to the extension of tumor from the nasal cavity. Primary tumor can occur in these sinuses but is relatively less common, and discussion in this chapter will focus on maxillary sinus and its pathology.
Figure 11.1 demonstrates the schematic anatomy of the nose and PNS and their relation to surrounding structures. The inferior part is formed by the palate and alveolus. The superior part is related to the ethmoid sinus, to the skull base and frontal sinus medially, and to the orbital floor and eye laterally. The posterior compartment is formed by the muscle of mastication in ITF.
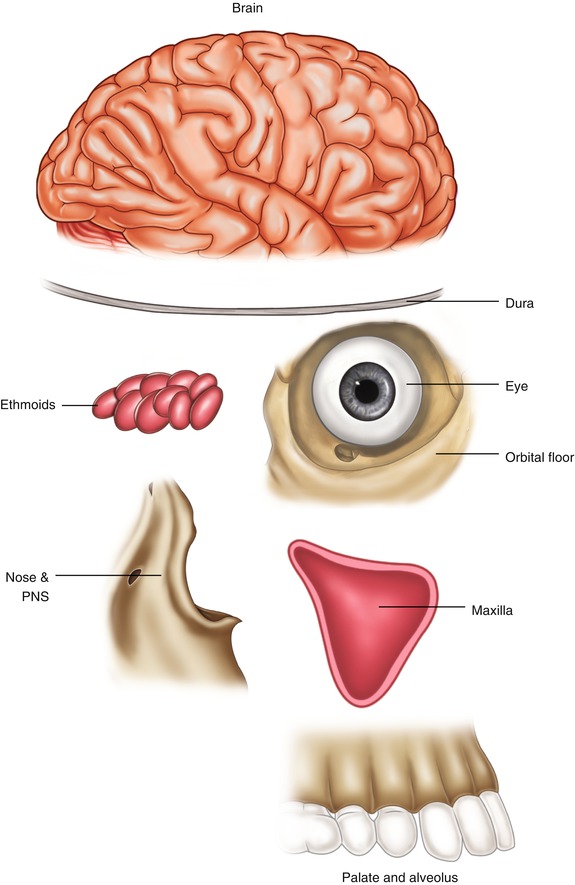
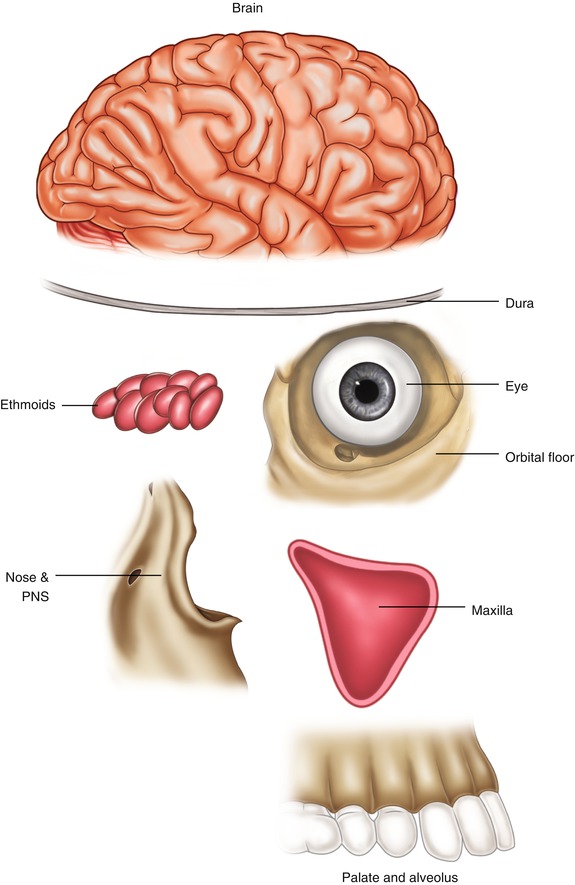
Fig. 11.1
Schematic representation of paranasal sinus
Surgical Pathology
This is one of the most challenging areas to deal with surgically, and understanding the pattern of spread of the tumor is critical in achieving clear margins. Figure 11.2 shows the path of spread of the tumor in a schematic manner. It is mandatory to have imaging studies in the form of CT scan and MRI to evaluate the extent of disease spread. Many times both CT scan and MRI are needed for detailed evaluation. CT scan is always the first imaging modality that outlines the extent of spread. MRI is done to see soft tissue involvement in relation to the orbit and optic nerve, dura, and brain involvement and assess perineural spread. There is possibility of variety of tumor pathology. It is essential to know exact tumor pathology, and one should not hesitate to ask for immunohistochemistry studies to confirm the histopathology result. This is important to plan treatment protocol and overall prognosis depends upon the tumor biology.
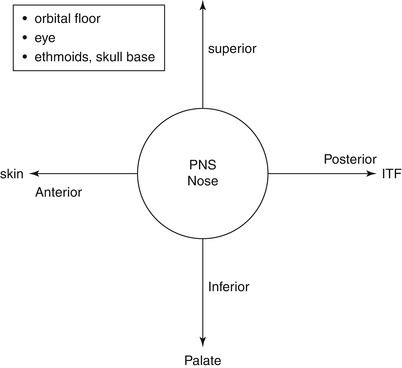
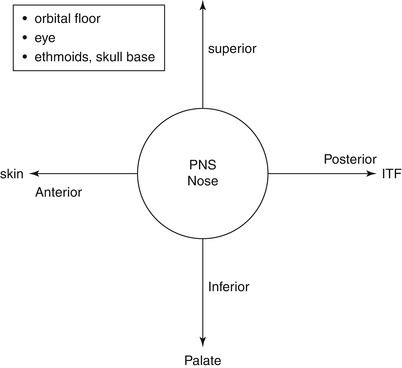
Fig. 11.2
Pattern of spread of paranasal sinus tumors
The surgical planning is in accordance with the extent of disease spread. Figure 11.3 demonstrates various surgical approaches to address these tumors. Tumor spreading inferiorly is addressed by infrastructure maxillectomy, while tumor spreading upwards needs maxillectomy with orbital exenteration. If the skull base is involved, anterior skull base resection is required. The tumor limited to anterior ethmoid can be cleared by trans-facial resection, while combined approaches are required for posterior and superior ethmoid involvement of the lesion. The posterior spread into ITF is the most challenging and requires posterior to anterior approach (compartment approach) to address the 3rd margin. This procedure is described in the chapter addressing ITF resection.
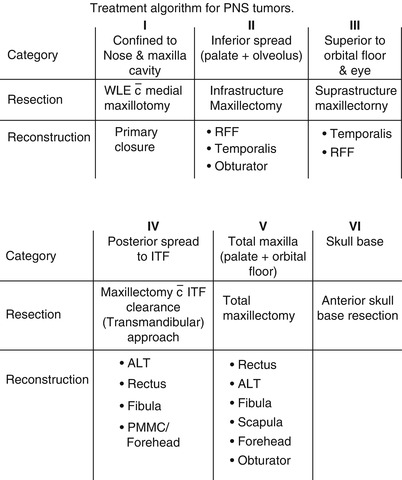
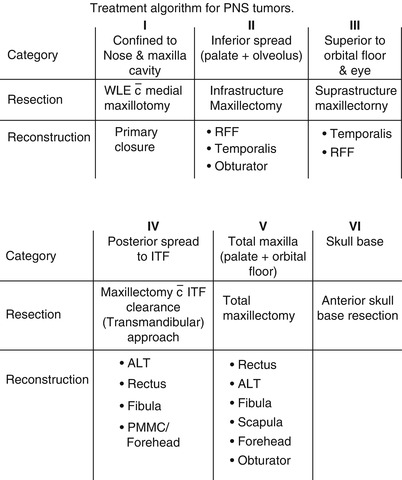
Fig. 11.3
Treatment algorithm for PNS tumors
Surgical Concepts
Imaging studies with CT scan and MRI are essential before planning the surgery.
It is advisable to accurately map the tumor and outline various structures involved by the tumor. This helps in planning the surgical approach and reconstruction.
Surgery remains the primary treatment approach, but long-term outcome depends upon tumor biology.
Removal of the eye is a sensitive issue and every chance should be given to conserve it. The eye needs to be resected if the tumor involves the rectus muscle, ocular fat, and optic nerve. Involvement of periorbita is not an indication for orbital exenteration.
The majority of tumors are addressed by lateral rhinotomy incision. One can have vertical extension (lynch extension) or lateral extension (Weber–Ferguson extension) depending upon the structures to be removed.
It may be difficult to achieve wide margins for tumor in this area. It is essential to dissect in a clear tissue plane between the tumor and vital structure. The decision to sacrifice structure is taken when clear plane is not available.
The tumor with posterior spread needs transmandibular approach.
Combined craniofacial resection is reserved for lesions involving the cribriform plate, dura, and brain.
Trans-nasal endoscopic approach has become popular in recent time. One needs to be very careful in applying this approach to malignant neoplasm, and surgical clearance should not be compromised at any cost. It is essential to have the capacity to perform extensive endoscopic sinus surgery and open anterior skull base surgery before attempting endoscopic removal of malignant lesion. It is best reserved for early, low-grade malignancy in experienced hand.
The reconstruction poses a difficult challenge and one has to plan carefully to have a good functional outcome.
Wide Excision
This section demonstrates a surgical procedure for early nose and paranasal sinus tumor.

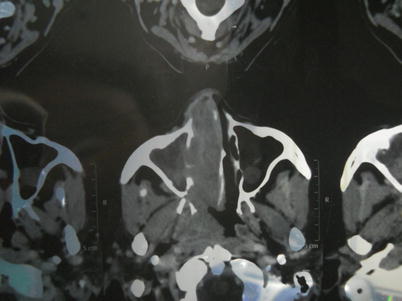

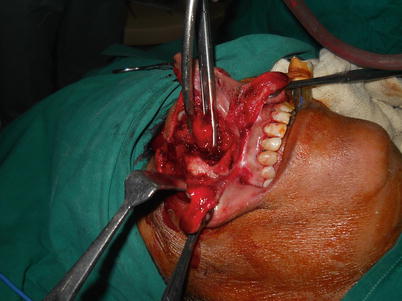










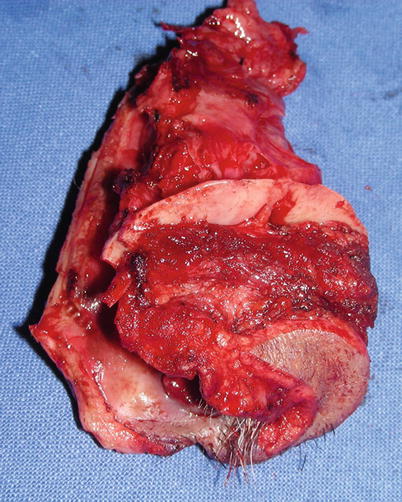

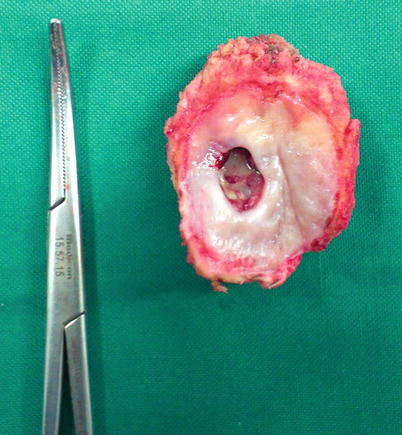
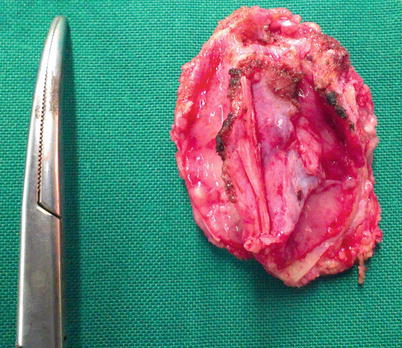







Fig. 11.4
This is a lateral rhinotomy incision with lip split extension. The lip split is not essential in all cases but does provide good excess to perform bone cuts
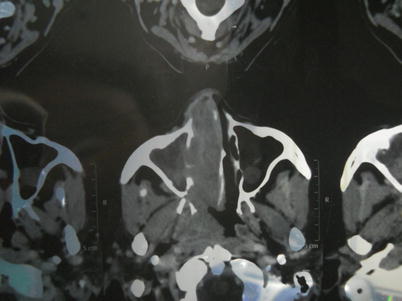
Fig. 11.5
Tumor extension on a CT scan plate showing involvement of the lateral nasal wall in the entire length. This lesion can be addressed endoscopically provided the surgeon has adequate experience of doing endoscopic surgeries and performing open cancer surgeries

Fig. 11.6
The flaps are raised to expose the lesion and anterior maxilla
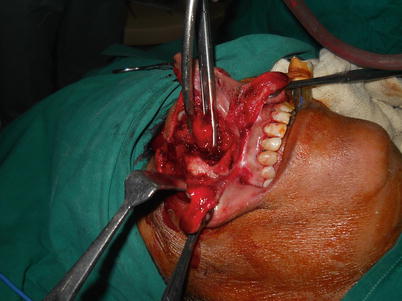
Fig. 11.7
The medial wall of the maxilla is exposed for bone cuts

Fig. 11.8
Cuts are made to perform medial maxillotomy. The removal of the anterior wall of the maxilla in medial part allows easy access to the lateral nasal wall in the entire length

Fig. 11.9
The resection is complete. This surgery results in bleeding and one has to learn to work with bleeding. The systolic blood pressure can be kept low to reduce the bleeding. It stops once the lesion is completely out

Fig. 11.10
The closure of the wound. The nasal cavity is packed for 2–3 days, and the patient is advised to clean the cavity with salt water in postoperative period to avoid crusting

Fig. 11.11
Patient with nasal tumor involving part of the skin

Fig. 11.12
Similar approach to the first case to perform wide excision of lesion including the skin

Fig. 11.13
Photograph showing specimen

Fig. 11.14
The reconstruction was planned with radial forearm free flap

Fig. 11.15
The flap is inserted to cover the skin defect

Fig. 11.16
The closure is complete. This defect could have been closed primarily with an advancement flap

Fig. 11.17
Long-term outcome
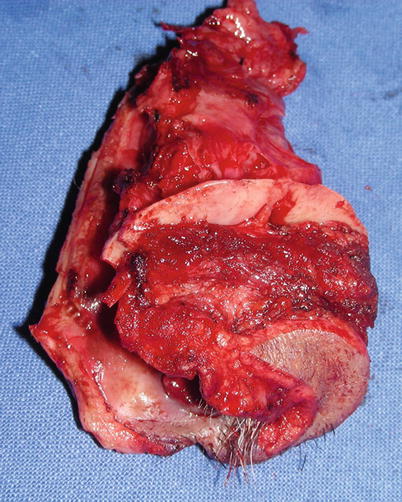
Fig. 11.18
Patient with lesion in the hard palate. The biopsy result suggested malignant neoplasm, and CT scan showed palatal bone was not involved. It is important to remember that one needs to take extra layer of tissue in depth to have a clear margin. Removal of the palatal bone for all malignant neoplasm is mandatory

Fig. 11.19
Wide excision with palatal bone is complete and hemostasis is achieved
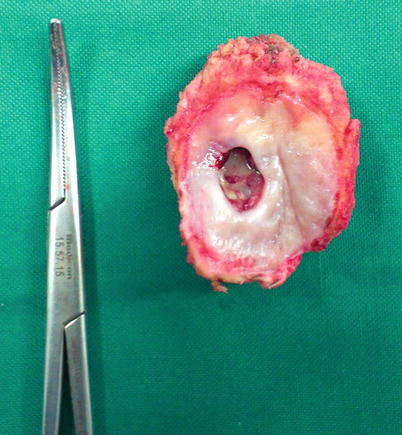
Fig. 11.20
Specimen showing clear margins
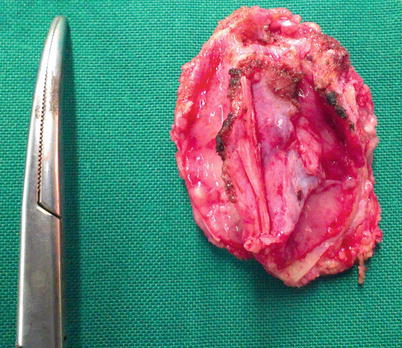
Fig. 11.21
The septum side showing normal anatomy confirming clear margins

Fig. 11.22
The reconstruction was planned with a combination of buccal rotation flap and palatal rotation flap. Smaller defects can be addressed with palatal rotation alone or facial artery myomucosal flap (FAMM)

Fig. 11.23
Both the flaps are sutured together to have complete seal for palatal defect

Fig. 11.24
Photograph showing completed procedure

Fig. 11.25
Patient with palatal defect

Fig. 11.26
The reconstruction was performed with obturator

Fig. 11.27
The final outcome. The obturator is a simple method to rehabilitate these patients and gives very good outcome in the majority of cases
Infrastructure Maxillectomy
This section shows surgical procedure to remove PNS tumor that spreads inferiorly and involves the palate and alveolus.
 < div class='tao-gold-member'>
< div class='tao-gold-member'>





Only gold members can continue reading. Log In or Register to continue
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


