 Tumors of the Lacrimal Drainage System
Tumors of the Lacrimal Drainage SystemLacrimal Drainage System Tumors
General Considerations
A variety of tumors can arise in the canaliculus, lacrimal sac, and the nasolacrimal duct, with the majority originating in the lacrimal sac. The section introduces the subject of tumors and pseudotumors of the lacrimal drainage system and provides some selected general references (1,2,3,4,5,6,7,8,9,10,11,12). Following that, a few of the specific lesions will be discussed, illustrated, and referenced in more detail.
Various surveys of lacrimal sac tumors and pseudotumors have shown considerable differences in the incidence of these lesions. In one series of 115 solid tumors of the lacrimal sac, 55% were malignant (4). The most common primary neoplasms of the lacrimal sac appear to be epithelial tumors, particularly squamous papilloma and squamous cell carcinoma. However, one study reported that non-Hodgkin’s B-cell lymphoma was the most common lacrimal sac neoplasm (11). Other tumors and pseudotumors that have been reported less often in the lacrimal drainage system include melanoma, oncocytoma, hemangiopericytoma, solitary fibrous tumor, peripheral nerve tumors, angiofibroma, granular cell tumor, cavernous hemangioma, pleomorphic adenoma, adenocarcinoma, and adenoid cystic carcinoma. A series of 35 cases of nonepithelial tumors of the lacrimal sac revealed that fibrous histiocytoma was most common, followed by lymphoma and melanoma (9). Non-neoplastic conditions that can simulate lacrimal sac tumors include cyst, hematoma, pyogenic granuloma, and juvenile xanthogranuloma. Many of these tumors are the same as those that develop in the eyelid and conjunctiva and they are discussed in detail elsewhere in this atlas. However, because of their location, they usually have a different clinical presentation and are less visible than those on the eyelids and conjunctiva. Because lacrimal sac tumors are uncommon, we do not have examples of every condition. Hence, most of them are discussed in general terms, but not illustrated.
Clinical Features
Most neoplasms of the lacrimal sac are indistinguishable clinically and must be differentiated from the more common dacryocystitis. The latter occurs more often in infants or young children and is associated with inflammatory signs, is soft and fluctuant, and often has a purulent discharge that can be expressed with pressure. It generally is evident inferior to the medial canthus. In contrast, a solid neoplasm generally appears in adults as a progressive, firm, subcutaneous mass, usually, but not always superior to the medial canthus. Secondary epiphora, sometimes tinged with blood, is a common presenting feature (2). Melanoma can occur in the lacrimal sac as a de novo lesion or from epithelial extension from conjunctival melanoma, usually in association with primary acquired melanosis (PAM).
Diagnostic Approaches
Most tumors of the eyelid and conjunctiva can be appreciated clinically by direct visualization. However, those in the lacrimal sac are not so readily visible and imaging studies, including computed tomography (CT), magnetic resonance imaging (MRI), and dacryocystograms may provide more important information about the extent and nature of the lesion. Most tumors are initially circumscribed, defined by the walls of the lacrimal sac. Later, the more aggressive neoplasms lose their definition and become more diffuse or ill defined on imaging studies.
Pathology
The histopathology of tumors and pseudotumors of the lacrimal sac is discussed under the same tumor categories in the eyelid and conjunctival sections of this atlas. The only exception is that squamous cell carcinoma of the lacrimal sac generally arises from an inverted papilloma and often has an invasive spindle cell component. There is controversy as to pathogenesis of hemangiopericytoma, fibrous histiocytoma, and solitary fibrous tumor, all of which have been reported to arise in the lacrimal sac. All are similar histopathologically and are discussed further in the section on orbital tumors. Human papillomavirus (HPV) appears to be involved in the pathogenesis of epithelial neoplasms of the lacrimal sac, with HPV type 11 reportedly associated with benign lesions and HPV type 18 reportedly associated with malignant lesions (6,12).
Management
The management of a lacrimal sac neoplasm varies with the clinical findings and suspected diagnosis. When possible, primary neoplasms are managed initially by complete surgical removal by dacryocystectomy. The specific surgical approach depends on the surgeon’s preference. A nasal cutaneous approach (Lynch incision) generally provides adequate surgical exposure.
Additional treatment may be required, depending on the final histopathologic diagnosis. More malignant epithelial tumors, lymphoma, and metastasis may require local irradiation or chemotherapy, depending on the specific diagnosis. Wide excision is important for papilloma, because lacrimal sac papilloma is invasive and has a high incidence of recurrence. In advanced cases, orbital or sinus exenteration may be necessary. Inflammatory conditions like juvenile xanthogranuloma and pyogenic granuloma can be treated with supplemental local or oral corticosteroids. Regardless of the diagnosis, subsequent reconstruction of the lacrimal drainage system can be undertaken, provided there is no tumor recurrence within a few months (11). The prognosis varies with the specific diagnosis.
Selected References
1. Ryan SJ, Font RL. Primary epithelial neoplasms of the lacrimal sac. Am J Ophthalmol 1973;76:73-88.
2. Hornblass A, Jakobiec FA, Bosniak S, et al. The diagnosis and management of epithelial tumors of the lacrimal sac. Ophthalmology 1980;87:476-490.
3. Ni C, D’Amico DJ, Fan CQ, et al. Tumors of the lacrimal sac: a clinicopathological analysis of 82 cases. Int Ophthalmol Clin 1982;22:121-140.
4. Stefanyszyn MA, Hidayat AA, Pe’er JJ, et al. Lacrimal sac tumors. Ophthalmol Plast Reconstr Surg 1994;10:169-184.
5. Flanagan JC, Stokes DP. Lacrimal sac tumors. Ophthalmology 1978;85: 1282-1287.
6. Madreperla SA, Green WR, Daniel R, et al. Human papillomavirus in primary epithelial tumors of the lacrimal sac. Ophthalmology 1993;100:569-573.
7. Pe’er J, Hidayat AA, Ilsar M, et al. Glandular tumors of the lacrimal sac. Their histopathologic patterns and possible origins. Ophthalmology 1996; 103:1601-1605.
8. Anderson NG, Wojno TH, Grossniklaus HE. Clinicopathologic findings from lacrimal sac biopsy specimens obtained during dacryocystorhinostomy. Ophthalmol Plast Reconstr Surg 2003;19:173-176.
9. Pe’er JJ, Stefanyszyn M, Hidayat AA. Nonepithelial tumors of the lacrimal sac. Am J Ophthalmol 1994;118;650-658.
10. Stokes DP, Flanagan JC. Dacryocystectomy for tumors of the lacrimal sac. Ophthalmic Surg 1977;8:85-90.
11. Parmar DN, Rose GE. Management of lacrimal sac tumours. Eye 2003;17: 599-606.
12. Nakamura Y, Mashima Y, Kameyama K, et al. Detection of human papillomavirus infection in squamous tumours of the conjunctiva and lacrimal sac by immunohistochemistry, in situ hybridisation, and polymerase chain reaction. Br J Ophthalmol 1997;81:308-313.
Lacrimal Sac Squamous Papilloma and Carcinoma
General Considerations
The most important primary epithelial neoplasms of lacrimal sac are squamous papilloma and squamous cell carcinoma with squamous papilloma often evolving into carcinoma (1,2,3,4,5,6,7,8,9,10,11,12,13,14,15,16,17). Unlike the benign, noninvasive papilloma of the eyelid skin described previously, papilloma of the lacrimal sac is usually of the inverted type, also called transitional cell carcinoma or schneiderian papilloma, and is more invasive. It can arise primarily from the lacrimal sac or can extend into the sac from the nose or maxillary sinus.
Clinical Features
Both inverted papilloma and squamous cell carcinoma are slowly invasive and frequently recur after excision. Local intracranial extension can develop in more aggressive tumors, such as mucoepidermoid carcinoma (13). Transformation of inverted papilloma into squamous cell carcinoma occurs in 10% to 15% of cases, at which time the tumor becomes more locally invasive and can occasionally exhibit orbital recurrence, brain invasion, and distant metastasis (2).
Pathology
The histopathology of squamous papilloma and squamous cell carcinoma were discussed in the section on squamous neoplasms of the conjunctiva. Squamous cell carcinoma can also arise in the lacrimal sac de novo, without a prior papilloma. The mucoepidermoid variant of squamous cell carcinoma has also been found to arise primarily in the lacrimal sac (7,8,13).
Management
Management of lacrimal sac neoplasms was discussed in the previous section.
Selected References
1. Streeten BW, Carrillo R, Jamison R, et al. Inverted papilloma of the conjunctiva. Am J Ophthalmol 1979;88:1062-1066.
2. Elner VM, Burnstine MA, Goodman ML, et al. Inverted papillomas that invade the orbit. Arch Ophthalmol 1995;113:1178-1183.
3. Nakamura Y, Mashima Y, Kameyama K. Human papilloma virus DNA detected in case of inverted squamous papilloma of the lacrimal sac. Br J Ophthalmol 1995;79:392-393.
4. Williams R, Ilsar M, Welham RA. Lacrimal canalicular papillomatosis. Br J Ophthalmol 1985;69:464-467.
5. Fechner RE, Sessions RB. Inverted papilloma of the lacrimal sac, the paranasal sinuses and the cervical region. Cancer 1977;40:2303-2308.
6. Katircioglu YA, Altiparmak UE, Akmansu H, et al. Squamous cell carcinoma of the lacrimal sac. Orbit. 2003;22:151-153.
7. Hornblass A, Jakobiec FA, Bosniak S, et al. The diagnosis and management of epithelial tumors of the lacrimal sac. Ophthalmology 1980;87:476-490.
8. Kohn R, Nofsinger K, Freedman SI. Rapid recurrence of papillary squamous cell carcinoma of the canaliculus. Am J Ophthalmol 1981;92:363-367.
9. Bonder D, Fischer MJ, Levine MR. Squamous cell carcinoma of the lacrimal sac. Ophthalmology 1983;90:1133-1135.
10. Ni C, Wagoner MD, Wang W, et al. Mucoepidermoid carcinomas of the lacrimal sac. Arch Ophthalmol 1983;101:1572-1574.
11. Blake J, Mullaney J, Gillan J. Lacrimal sac mucoepidermoid carcinoma. Br J Ophthalmol 1986;70:681-685.
12. Anderson KK, Lessner AM, Hood I, et al. Invasive transitional cell carcinoma of the lacrimal sac arising in an inverted papilloma. Arch Ophthalmol 1994;112:306-307.
13. Khan JA, Sutula FC, Pilch BZ, et al. Mucoepidermoid carcinoma involving the lacrimal sac. Ophthalmol Plast Reconstr Surg 1988;4:153-157.
14. Bambirra EA, Miranda D, Rayes A. Mucoepidermoid tumor of the lacrimal sac. Arch Ophthalmol 1981;99:2149-2150.
15. Stephenson JA, Mayland DM, Ingall G, et al. Squamous cell carcinoma of the lacrimal sac. Otolaryngol Head Neck Surg 1988;99:524-527.
16. Fishman JR, Gladstone GJ, Jackson IT. Squamous cell carcinoma of the lacrimal sac. Plast Reconstr Surg 1993;92:1375-1379.
17. Katircioglu YA, Altiparmak UE, Akmansu H, et al. Squamous cell carcinoma of the lacrimal sac. Orbit 2003;22:151-153.
Lacrimal Sac Squamous Cell Papilloma and Carcinoma
Bonder D, Fischer M J, Levine M R. Squamous cell carcinom a of the lacrim al sac. Ophthalmology 1983;90:1133-1135.
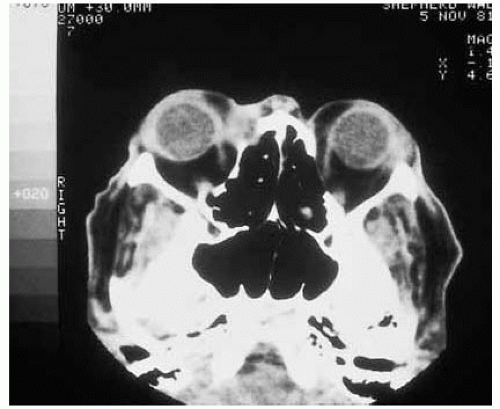 Figure 14.2. Axial computed tomography of the lesion shown in Figure 14.1, disclosing the 2-cm, soft tissue density in the region of the right lacrimal sac. (Courtesy of David Bonder, MD, and Mark R. Levine, MD.) |
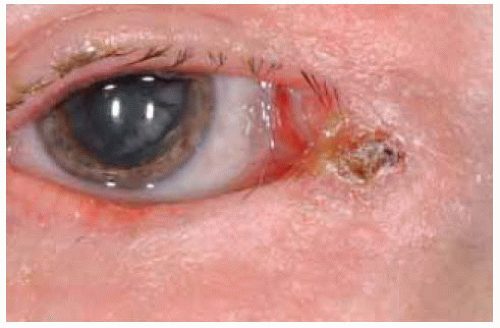 Figure 14.4. Closer view of lesion in Figure 14.3, showing fleshy mass in the medial canthal area and excoriation of the overlying skin. (Courtesy of David Bonder, MD, and Mark R. Levine, MD.)
Stay updated, free articles. Join our Telegram channel
Full access? Get Clinical Tree
 Get Clinical Tree app for offline access
Get Clinical Tree app for offline access

|

