Tumors of the Eyelids
Brian P. Marr
Carol L. Shields
Jerry A. Shields
The eyelids are a highly specialized region of the ocular adnexa consisting of multiple tissue types, all having the potential to give rise to a spectrum of benign and malignant lesions. Accurate identification and classification of these lesions is important for proper care and management.
Tumors of the eyelids can be classified based on origin such as tumors of the epidermis/dermis, tumors of melanocytic origin, and those of glandular, neural, vascular, metastatic, xanthomatous, histiocytic, and inflammatory origin. In this chapter we discuss the various eyelid tumors based on their site of origin.
BENIGN TUMORS OF THE EPIDERMIS
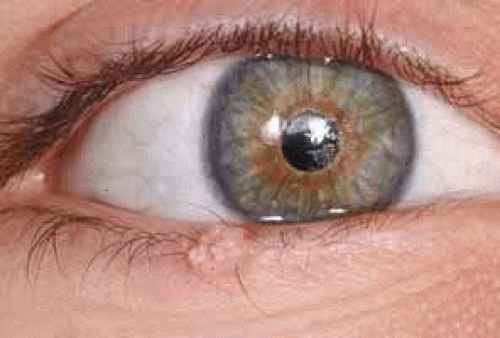
PAPILLOMA
Eyelid papilloma is a common benign growth arising from the periocular skin in older individuals. It is a flesh colored, pedunculated or sessile lesion with a corrugated or cerebriform surface (Fig. 1).1 Clinically it can simulate other benign and malignant lesions such as verruca vulgaris, seborrheic keratosis, inverted follicular keratosis, fibroma, and squamous call carcinoma. The majority of eyelid papillomas can be observed unless they cause mechanical disruption of eyelid function or are cosmetically disfiguring, in which case they can be completely excised. If a papilloma becomes irritated or painful excision is warranted.
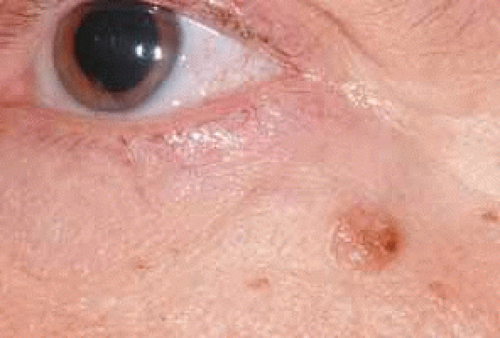
SEBORRHEIC KERATOSIS
Seborrheic keratosis is a pigmented cutaneous lesion that can occur throughout the skin in older individuals but can develop in the eyelid area. This raised lesion can be smooth or verrucous, with varied pigmentation, size, and distribution (Fig. 2).2 It can be mistaken for cutaneous melanoma because of its pigmented appearance. It is managed with observation or surgical excision.3
KERATOACANTHOMA
Keratoacanthoma is a relatively rapidly growing skin lesion that can occur on the face and eyelids. Classically, it appears as a nodular mass with a central keratin-filled crater (Fig. 3). It generally develops on the skin but has been rarely recognized on mucous membranes including conjunctiva.4,5,6,7,8,9 It typically has a rapid onset over a few months and then regresses over a period of months. Clinically, it resembles noduloulcerative basal cell carcinoma or squamous cell carcinoma and may be difficult to differentiate from these lesions. Multiple keratoacanthomas occur in Ferguson-Smith syndrome and Muir-Torre syndrome. These syndromes can be associated with systemic neoplasms, particularly of the gastrointestinal system.4,10,11 Keratoacanthoma can be managed by observation, but has the potential to grow rapidly and be locally destructive or indistinguishable from true malignancy. For these reasons early complete excision is diagnostic and curative. For larger lesions or those involving critical structures, incisional biopsy can be preformed to exclude carcinoma, knowing that sampling error may occur. Other treatments such as cryotherapy, radiotherapy, and intralesional chemotherapy have been used, however, surgical excision is preferred when possible.5
INVERTED FOLLICULAR KERATOSIS
Inverted follicular keratosis, also known as basosquamous-cell acanthoma because of its lack of hair follicle involvement histopathologically, is a papillomatous skin nodule that occurs commonly on the face and eyelid margin in middle-aged adults.12 It is usually a solitary lesion that is more common in males and develops over a period of months. It can appear as a nodule at the eyelid margin often with a crusted surface. Control of these lesions is obtained with complete surgical excision. It is now believed to be an abortive variant of irritated seborrheic keratosis.12
PSEUDOCARCINOMATOUS HYPERPLASIA
Pseudocarcinomatous hyperplasia is a benign condition that simulates an eyelid malignancy. This lesion progresses quickly over a period of weeks and frequently is nodular with a crusted or ulcerated surface. It is usually idiopathic or can be a reactive phenomenon related to previous surgery, trauma, medication, adjacent carcinoma, or mycotic infections.13 Surgical excision is warranted to rule out malignancy.
EPIDERMAL INCLUSION CYST
Epidermal inclusion cyst is a slow-growing, firm, smooth, keratin-filled cystic lesion commonly found on both the upper and lower eyelids. This subcutaneous lesion arises spontaneously from pilar cysts or from trauma. Multiple epidermal inclusion cysts have been described in Torre’s syndrome and Gardner’s syndrome where they are associated with certain systemic malignancies.11,14 Care should be taken to remove the entire cyst to minimize the chance for recurrence.
MALIGNANT TUMORS OF THE EPIDERMIS
BASAL CELL CARCINOMA
Basal cell carcinoma of the skin is the most common malignancy in Caucasians.15 It arises from the basal layer of the epidermis and locally invades surrounding tissues. Although basal cell carcinoma rarely metastasizes, it can be quite invasive and destructive. Basal cell carcinoma commonly affects the periocular skin, comprising 80% to 90% of all eyelid malignancies.16,17 The incidence of eyelid basal cell carcinomas is 14 per 100,000 population per year in white Americans and higher rates have been observed in other countries.18,19,20,21 Basal cell carcinoma typically occurs in older men and woman above the age of 50 and tends to affect individuals with fair complexion (blonde or red hair with blue or green eyes). Risk factors associated with development of basal cell carcinoma include ultraviolet radiation exposure, fair skin, sunburn during childhood, arsenic exposure, immunosuppression, previous basal cell carcinoma, and family history of skin cancer.
Basal cell carcinoma can be categorized into two basic types, the noduloulcerative and morpheaform, or sclerosing, variant. The noduloulcerative variant is the most common and accounts for 75% of basal cell carcinomas.18 It is a raised, firm, slow-growing, pearly or flesh-colored lesion. It typically shows telangiectatic vessels or ulceration, and usually demonstrates loss of overlying cilia (Fig. 4). The lower eyelid is most frequently involved, followed by the medial canthus, upper eyelid and lateral canthus. The morpheaform variant is typically diffuse, light colored, and relatively flat with indistinct borders (Fig. 5). This variant is more aggressive and invasive despite being less obvious, and it is more likely to show recurrence (Fig. 6).22,23 Other variants of basal cell carcinoma include pigmented, superficial, and cystic types.
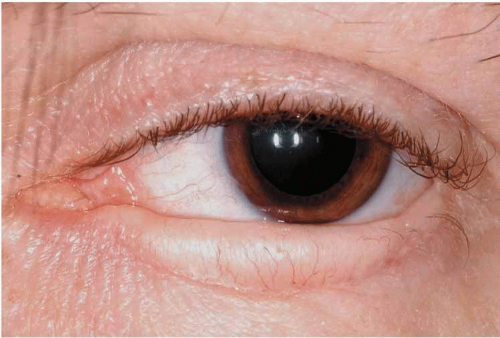 Fig. 5 Morpheaform basal cell carcinoma involving the entire lower eyelid showing a thickened lower eyelid and loss of cilia. |
 Fig. 6 Another morpheaform basal cell carcinoma involving the lower eyelid demonstrating its poorly defined margins. |
Systemic conditions associated basal cell carcinoma includes Gorlin-Goltz syndrome, xeroderma pigmentosum, nevus sebaceous of Jadassohn, and Bazex syndrome. Gorlin-Goltz syndrome is an autosomal dominant condition associated with multiple basal cell carcinomas that occur at an early age. Other findings include odontogenic keratocysts, palmer dyskeratosis, and bifid ribs.24 Xeroderma pigmentosum is an autosomal recessive condition associated with multiple skin carcinomas including basal cell carcinoma, squamous cell carcinoma, and melanoma. It is a result of a dysfunction in the DNA repair mechanism leaving individuals highly susceptible to ultraviolet radiation.24 Nevus sebaceous of Jadassohn is a sporadic condition that can be part of the organoid nevus syndrome. Cutaneous nevus sebaceous is a thickened greasy cutaneous plaque with an 8% to 14% chance of developing basal cell carcinoma and other adnexal neoplasms (Fig. 7).25 Bazex syndrome is an autosomal dominant condition characterized by multiple basal cell carcinomas in younger individuals.26 Associated findings include hypertrichosis, milia, hypohydrosis, and “ice-pick marks” on the extremities. Multiple basal cell carcinomas or occurrence at a young age should raise suspicion for associated syndromes.
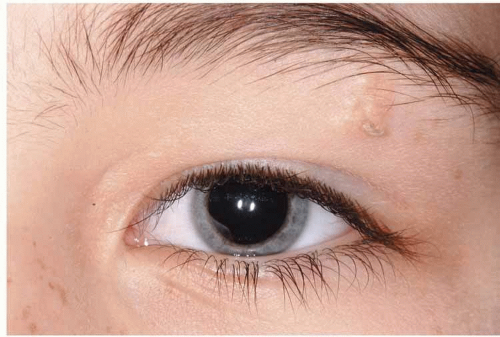 Fig. 7 Nevus sebaceous of Jadassohn located below the lateral eyebrow. Note the small cutaneous horn arising from it. |
Surgical management of primary lesions with wide margins and frozen section control or Mohs surgery is the preferred method of treatment and offers the lowest rates of recurrence.21,22 Most lesions can be removed and closed primarily. However, larger lesions may require reconstruction with grafts or flaps. Advanced lesions with extensive orbital invasion may require exenteration. Cryotherapy has been used in selected cases with reported success in treating small lesions.27 Radiotherapy has been used as a supplemental treatment in advanced cases.
SQUAMOUS CELL CARCINOMA
Invasive squamous cell carcinoma or squamous cell carcinoma in situ (Bowen’s disease) accounts for approximately 2% to 9% of eyelid malignancies.28,29,30 Lesions are typically seen in older individuals and have a predilection for Caucasian males, with a history of excessive exposure to ultraviolet radiation. Clinical presentation is variable but most lesions have associated skin damage or actinic keratosis (Fig. 8). The lower eyelid is affected more frequently and the lesion can involve the eyelid margin. It appears as a nodule or plaque with crusting and telangietatic vessels and rolled edges. Squamous cell carcinoma is locally invasive and can rarely metastasize to regional and distant lymph nodes. It is more commonly seen in immunocompromised patients.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree