(1)
Narayana Hridayalaya Multispeciality, Bangalore, India
The infratemporal fossa (ITF) has been a challenging area for clinicians for a long time. This area has complex anatomy with communications to many surrounding areas. Accurate assessment of disease spread is limited by the edema of tissue, and the area has a tendency to bleed heavily during surgery. These factors make the treatment of patient with lesion in ITF very complicated and challenging. There is very little in published literature regarding surgical approaches for ITF. This chapter focuses on various surgical approaches for ITF clearance. These approaches are based on our clinical experience of treating these cases over the past few years.
Surgical Anatomy and Pattern of Spread
Figure 13.1 is a schematic representation of the anatomy of masticator space. The masticator space includes masseter muscle, both the pterygoid muscles, temporalis muscle, ascending ramus of mandible, and pterygoid plates. The ITF consists of space medial to the mandible and masseter muscle is excluded. This area contains various neurovascular bundles and also harbours pterygoid venous plexus. The tumor can easily spread from ITF to various surrdunding areas to which it is connected (Fig. 13.2). The oral cavity tumors, particularly buccal mucosa and RMT tumors, have a high tendency to spread to masticator space due to close proximity to muscles of mastication. The ITF can also get involved by posteriorly located maxillary sinus lesions, and this poses a difficult surgical challenge. Tumors of temporal bone and orbital apex can also spread to this region. The ITF is connected to the middle cranial fossa through various foramina and lesion can spread to intracranial compartment early in its spread. Appropriate imaging studies are required to evaluate disease spread in this area.
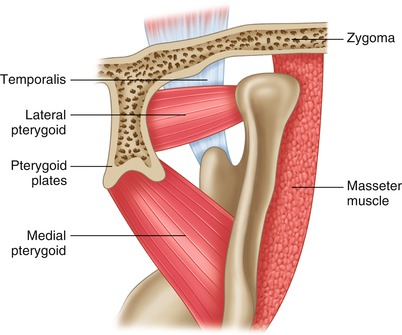
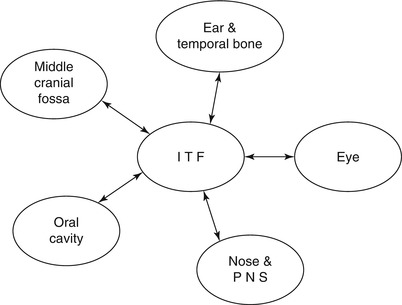
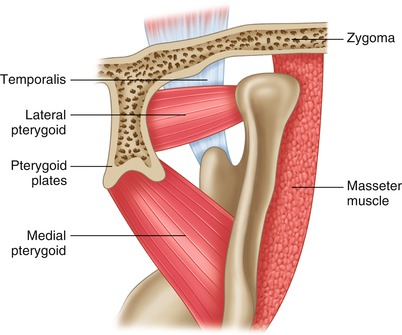
Fig. 13.1
Surgical anatomy of masticator space
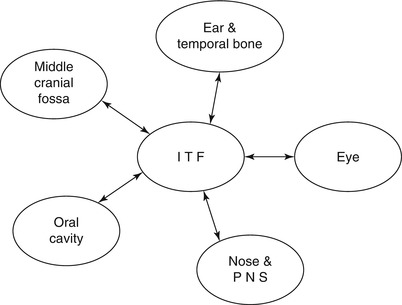
Fig. 13.2
Pattern of spread to and from ITF
Surgical Concepts
It is advisable to remove the entire masticator space as a single unit once involved (compartment approach). There are many advantages of this approach. The bleeding is minimal as we go around contents rather than through it. The entire content is removed, and hence a chance of leaving behind the disease is minimal and error in personal judgment about the extent of disease spread and surgical resection is avoided. The functional outcome remains largely similar to conventional approach.
The oral cancer spreading to ITF is best dealt with compartment clearance described in this chapter. We have classified these lesions to simplyfy their management. It is not ideal to group all such patients in one compartment and it is important to understand their pattern of spread.
The maxillary sinus tumors with ITF spread are best dealt by transmandibular approaches or posterior to anterior approaches. This is the only way to remove these tumors in en bloc fashion and achieve negative margin in depth.
The oral cavity tumors (mainly buccal mucosa and RMT) and PNS tumors involving only masticator space have fewer tendencies for distant metastasis. These tumors with extensive primary tumor spread have relatively less involvement of lymph nodes and distant organs. This warrants an aggressive surgical approach with a real possibility of curing them. This fact changes when tumor spreads to involve lateral pharyngeal wall and nasopharynx area. They present with large nodes and outcome reduces significantly for this group. If addressed surgically, it is advisable to remove parapharyngeal lymph nodes as we have found them involved in many instances.
Oral Cancer with Masticator Space Involvement (T4b)
The oral cancers that spread to masticator space are staged as T4b and are considered inoperable in majority of cases. There is a recent trend to stage these tumors as low ITF (below sigmoid notch) and high ITF (above sigmoid notch). The low ITF tumors are considered operable and are offered curative intent surgery while high ITF tumors are treated with palliative intent. However, this guideline is based on very limited data (eight cases for high ITF) and needs further evaluation [1, 2]. Buccal cancers generally involve the entire masticator space, while the tongue and oropharynx tumors tend to involve ITF.
The concept of compartment clearance for masticator was proposed by our group [3, 4]. The masticator space is essentially a soft tissue compartment containing various muscles, fats, lymphatics, and neurovascular bundles that are related closely to each other. This area is highly vascular and bleeds heavily during surgery. It is also very difficult to assess the exact extent of disease spread in this area either preoperatively or intraoperatively. These factors make conventional approach of clearance with 1 cm margin technically difficult. Removal of the entire soft tissue en bloc irrespective of the extent of spread solves many of these problems, and bleeding is minimal as dissection is around the compartment in facial planes. Initial experience with this approach was published with very satisfactory results for this group [3].
It is not ideal to group all these tumors in one as only tumors with potential to involve intracranial contents do badly. All the specimens of patients who underwent compartment surgery were studied extensively to understand the pattern of disease spread in masticator space [4]. The study correlated findings of clinical examination with findings of radiological and pathological examination to propose a classification system to form a treatment strategy.
Classification: (Fig. 13.3)
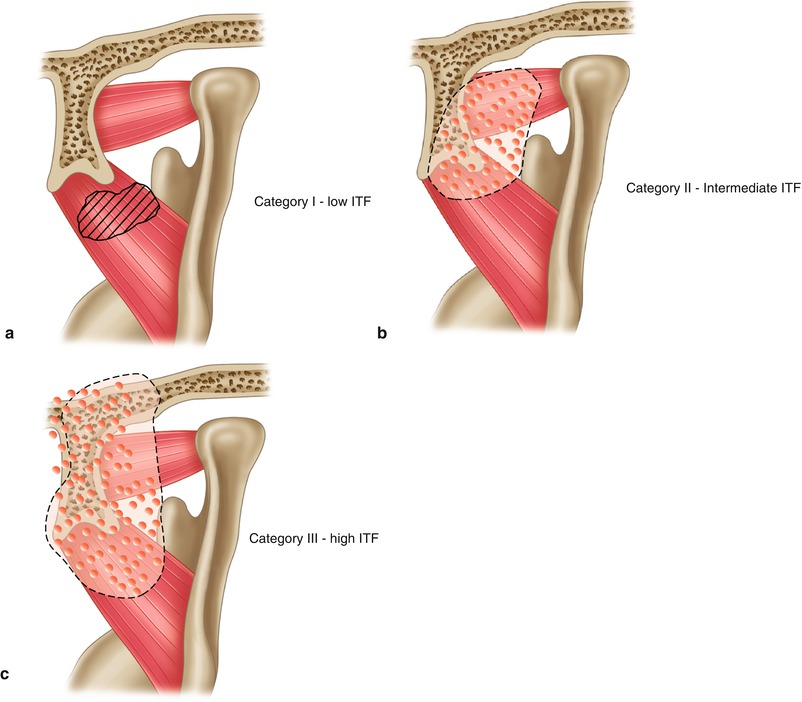
Fig. 13.3
Classification for oral cancer involving masticator space (T4b)
Category I: Low ITF – involvement of medial pterygoid and masseter muscle
Category II: Intermediate ITF – involvement of both pterygoid muscles, temporalis muscle, and pterygoid plates
Category III: High ITF – (A) involvement of pterygomaxillary fissure and (B) involvement of intracranial compartment
Categories I and II are considered operable and show good clinical outcome. The category III is considered to have high ITF involvement and generally has variable outcome. Involvement of pterygomaxillary fissure in the lower half can have good outcome with below described procedure for high ITF clearance, and we consider it in borderline operable category. The disease extending to intracranial compartment is considered inoperable and needs further studies. The study revealed that compartment surgical approach was helpful in achieving three-dimensional negative margins in all the cases of categories I and II. When the tumor reaches beyond the compartment (probably through pterygomaxillary fissure or through cranial foramina), then there is a chance of leaving behind the residual disease. This was also reflected in very good local control rate in published studies [3, 4]. The functional outcome remains similar to conventional approach as only the extra nonfunctioning tissue in depth is removed.
The surgical procedure is described in the subsequent section.
Compartment Surgery for Low ITF
We perform classical compartment surgery for category I and few category II cases. It is essential to remove the entire compartment also for category I lesions as that serves as an additional margin in depth. This is described in this section.

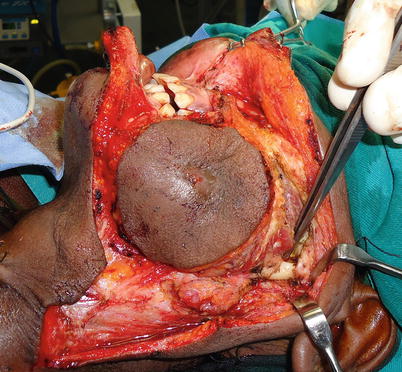
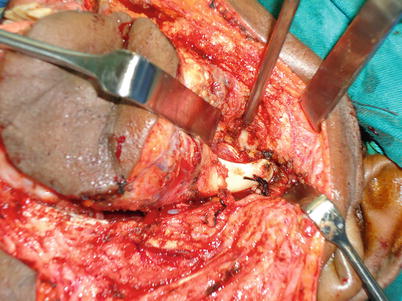
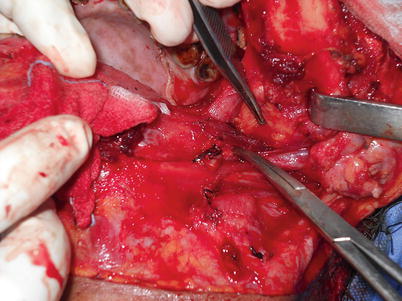

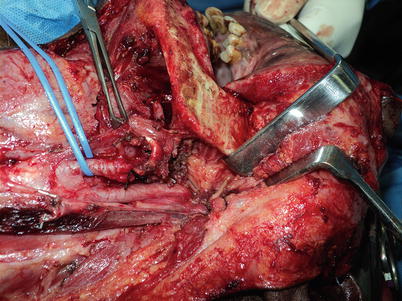
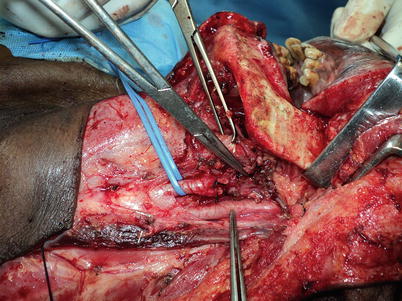
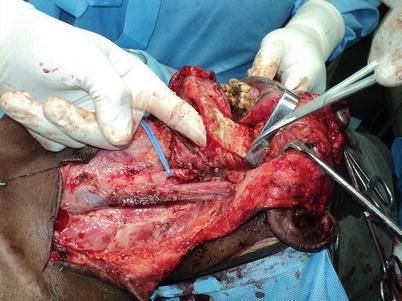
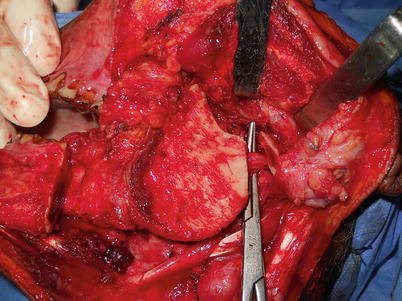
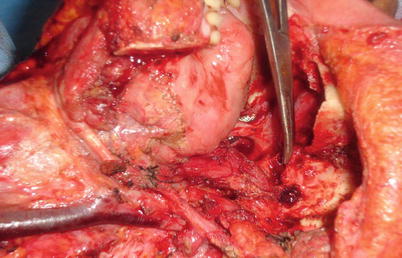





Fig. 13.4
Patient having recurrent buccal cancer involving masticator space. The lesion involves medial pterygoid muscle (category I) and causes complete trismus. The incision is planned with adequate skin margins. It is advisable to palpate for induration and edema and include all in resection margins
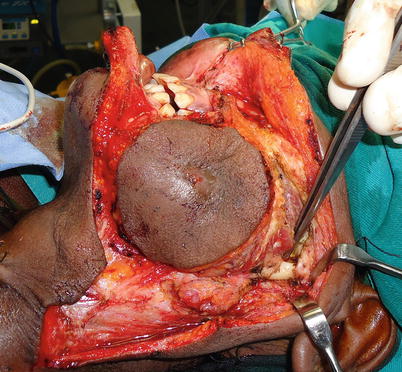
Fig. 13.5
Flaps are raised in conventional way exposing the zygoma and maxilla above and mandible below. The sigmoid notch is exposed posteriorly
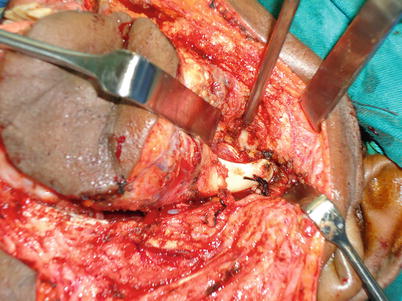
Fig. 13.6
The masseter and temporalis muscles are transacted to expose the skull base. The photograph shows exposed sphenoid wing of the skull base, lateral pterygoid muscle, and condyle
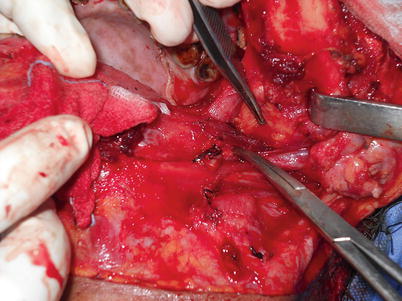
Fig. 13.7
The other steps to address buccal component are similar to conventional composite resection. This photo shows anatomy of pre-styloid parapharyngeal space. The muscles attached to styloid process serve as entry place for parapharyngeal space and fat pad is clearly evident in this photograph

Fig. 13.8
In case where lesion is going posteriorly to involve oropharynx and lateral pharynx, one needs to enter the space and expose the internal carotid artery in the entire length. The posterior belly of digastric muscle is identified, divided along with styloid muscles for that purpose. This step is not needed when dealing only with masticator space
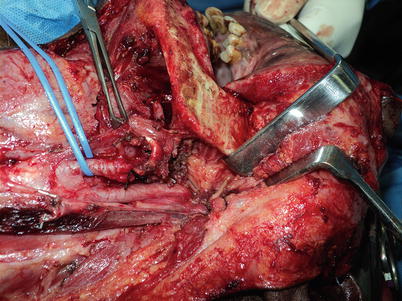
Fig. 13.9
The relation of medial pterygoid muscle to parapharyngeal fat plane is visible in this photograph
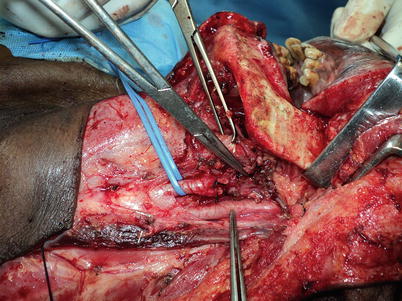
Fig. 13.10
The mandible is mobilized anteriorly by dividing stylomandibular ligament. The internal and external carotid arteries are exposed to demonstrate anatomy
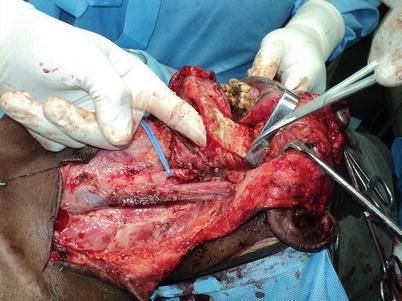
Fig. 13.11
The medial pterygoid muscle is lifted from parapharyngeal space just by inserting finger. This is an avascular plane from where skull base and lateral pterygoid plate can be palpated. This process mobilizes the entire masticator compartment posteriorly. The internal carotid artery is safe below the deep fascia
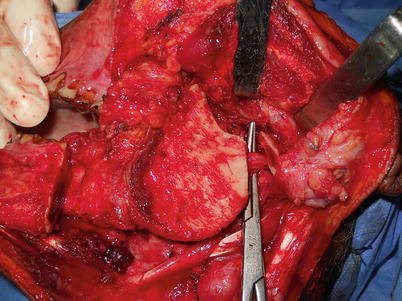
Fig. 13.12
The bone cuts are placed appropriately. The posterior mandible cut is made at sigmoid notch level preserving condyle to expose internal maxillary artery that can be ligated
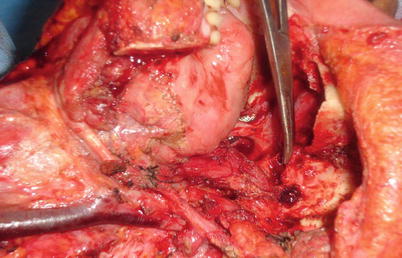
Fig. 13.13
The lateral pterygoid muscle and temporalis muscle are resected from skull base bone. This dissection is done by hugging the skull base bone and this is the single most important step in this process. The dissection is carried out from posterior to anterior direction. There are two areas that bleed heavily. The one is foramen ovale and the other is pterygomaxillary fissure. It is advisable to keep the blood pressure low (80 mmHg) while doing this process, and this really helps in reducing blood loss. We also use bone wax and gelform appropriately to control the bleeding. The bleeding stops immediately once the specimen is removed completely. The bone cuts on maxilla are placed to include both pterygoid plates from its root in the specimen. The photograph shows complete infratemporal fossa clearance with exposed skull bone, pterygomaxillary fissure, and root of pterygoid plates. The carotid artery is rarely at risk as the masticator compartment is mobilized from parapharyngeal space and the artery is safe behind the fascia all the time
< div class='tao-gold-member'>
Only gold members can continue reading. Log In or Register to continue
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


