Traumatic and Toxic Retinopathies
J. Luigi Borrillo
Carl D. Regillo
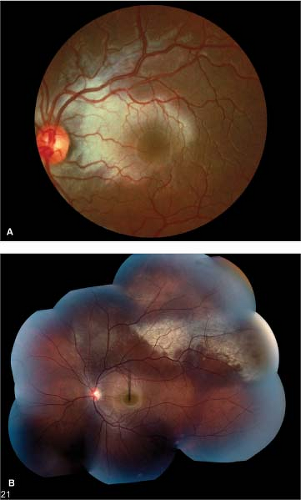
Commotio Retinae
Commotio retinae is retinal whitening that occurs after blunt ocular trauma. This transient condition affects the outer retina. Often the damage incurred to the photoreceptors is reversible.
Epidemiology
Statistically the condition is most common in young males.
History
Patients have a history of blunt ocular trauma.
Clinical Signs
The condition is usually asymptomatic. Decreased vision may occur with macular involvement. The retina appears whitened, while the retinal vasculature remains unaffected. The retina regains its normal appearance within weeks (Fig. 8-1). Occasionally, changes to the retinal pigment epithelium (RPE), such as stippling or clumping, may be seen after the retinal whitening resolves.
Be mindful of other findings seen in trauma such as hyphema or microhyphema, choroidal rupture, retinal hemorrhage, retinal dialysis, avulsed vitreous base, and vitreous hemorrhage.
Differential Diagnosis
Other entities that may mimic commotio retinae include branch retinal artery occlusion, white-without-pressure, and shallow retinal detachment.
Diagnostic Evaluation
Diagnosis is based on clinical examination.
Optical coherence tomography (OCT) may demonstrate increased reflectivity in areas of damaged photoreceptor outer segments.
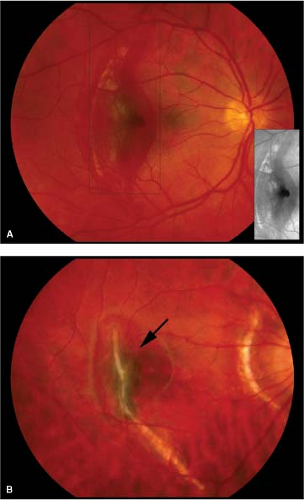
Choroidal Rupture
In this injury, disruption of the choriocapillaris and Bruch’s membrane occurs secondary to traumatic ocular compression. Ruptures located in the posterior pole are concentric to the optic disc. These breaks are often associated with subretinal and subretinal pigment epithelial hemorrhage.
Epidemiology and Etiology
Choroidal rupture occurs as a result of trauma, most commonly in young males.
History
Patients have a history of blunt ocular trauma.
Clinical Signs
The characteristic finding is subretinal hemorrhage, with whitish, crescent-shaped lesions around the optic disc (Fig. 8-2A). In the acute setting, choroidal ruptures may be associated with other findings from blunt ocular trauma such as hyphema, iris sphincter ruptures, commotio retinae, vitreous hemorrhage, retinal tears, retinal dialysis, and orbital fractures.
Later, choroidal neovascularization (CNV) may occur at the edge of the rupture site (Fig. 8-2B).
Differential Diagnosis
Myopic lacquer cracks and angioid streaks may have a similar appearance.
Other causes of subretinal hemorrhage include CNV, retinal arterial macroaneurysm, Valsalva retinopathy, and anemia.
Diagnostic Evaluation
Diagnosis is based on clinical examination.
Avulsed Vitreous Base
This entity describes separation of the vitreous base at the ora serrata that occurs secondary to trauma. Sometimes the avulsed vitreous base can be seen floating in the periphery.
Epidemiology and Etiology
The injury occurs as a result of trauma, usually in young males.
History
Patients have a history of blunt ocular trauma.
Clinical Signs
A semitransparent, sometimes pigmented, curvilinear ribbon-like structure may or may not be completely separated from the retinal periphery (Fig. 8-3).
The presence of an avulsed vitreous base is pathognomonic for ocular trauma.
An avulsed vitreous base may be associated with hyphema, iris sphincter tears, commotio retinae, vitreous hemorrhage, retinal tears, retinal dialysis, or orbital fractures.
Differential Diagnosis
Avulsed vitreous base should be distinguished from retinal dialysis.
Other entities that may mimic this condition include old vitreous hemorrhage.
Diagnostic Evaluation
Diagnosis is based on binocular indirect ophthalmoscopy with scleral depression.
Prognosis and Management
No treatment is necessary. Patients should be observed for the subsequent development of trauma-related ocular problems such as retinal breaks and angle-recession glaucoma.
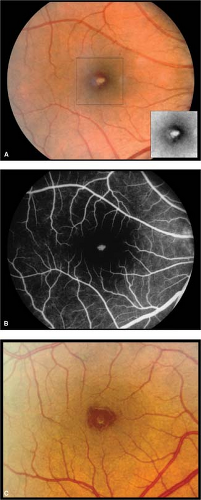
Solar Maculopathy
Solar maculopathy is the visual loss resulting from foveal photoreceptor and retinal pigment epithelial damage as a consequence of sungazing or direct observation of a solar eclipse.
Epidemiology
There is a trend for higher incidence in areas where a solar eclipse was directly observable. Solar maculopathy is more common among individuals involved in sun-worshiping religious groups. Loss of the ozone layer has been associated with solar retinopathy among sunbathers in the United States.
History
Patients have a history of sungazing.
Clinical Signs
There is an abnormal foveal reflex.
Often, a sharply demarcated yellow or reddish spot is visible in the fovea (Fig. 8-4).
Retinal pigment epithelial changes (focal hyperpigmentation) may be evident in the foveal or parafoveal area at later stages.
Differential Diagnosis
Pseudomacular hole, photic maculopathy, and macular dystrophy or degeneration may have a similar appearance.
Diagnostic Evaluation
Diagnosis is based on clinical examination.
Fluorescein angiography will reveal nonspecific retinal pigment epithelial window defects centered on the fovea.
OCT may demonstrate disruption of foveal inner and outer photoreceptor segments.
Prognosis and Management
Good visual recovery occurs in most patients, but it may take weeks or months for vision to improve.
No treatment is needed.
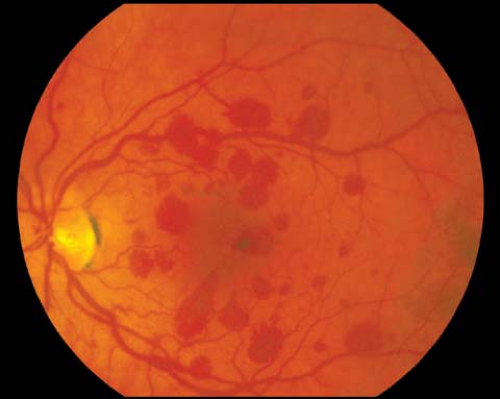
Valsalva Retinopathy
In Valsalva retinopathy, unilateral or bilateral retinal or preretinal hemorrhage occurs as a result of an acute episode of increased intrathoracic pressure. Superficial capillaries rupture secondary to a sharp rise in ocular intravenous pressure.
Epidemiology
The condition can occur in persons of any age.
History
Patients usually have a history of recent strenuous physical exertion, coughing, vomiting, or straining (e.g., with constipation).
Clinical Signs
Single or multiple intraretinal hemorrhages (often underneath the internal limiting membrane) are noted in the posterior pole (Fig. 8-5). There may be a decrease in visual acuity when the hemorrhage is localized in or over the foveal region.
Subconjunctival hemorrhage may be associated with this condition. Significant vitreous hemorrhage is rare.
Differential Diagnosis
Retinal macroaneurysm, diabetic retinopathy, venous occlusion, anemia, anticoagulant therapy, retinal tear, or posterior vitreous detachment with associated hemorrhage may mimic the findings of Valsalva retinopathy.
Diagnostic Evaluation
Diagnosis is based on clinical examination.
B-scan ultrasonography is performed to evaluate for underlying retinal detachment or retinal tear in the setting of dense vitreous hemorrhage.
OCT may demonstrate hemorrhage underneath reflective signal of the internal limiting membrane.
Shaken Baby Syndrome
This condition refers to intraocular hemorrhages in infants or young children secondary to child abuse. The findings are associated with decreased visual acuity and increased mortality.
Epidemiology
The condition is most common in infants and toddlers.
History
Recently, often multiple episodes of violent shaking of the infant precede findings, although it is often difficult to obtain a history of abuse from the caretaker. Caretakers may refuse diagnostic evaluation.
Clinical Signs
Subretinal, intraretinal, or preretinal hemorrhages are noted in one or (more commonly) both eyes (Fig. 8-6A). The preretinal hemorrhages are typically globular as opposed to flat (Fig. 8-6B). Other signs include poor visual or pupillary response. No single ocular finding is pathognomonic.
Ecchymosis, long bone and rib fractures, lethargy, or developmental delay are common associated findings. Often the child has physical findings that do not match the reported mechanism of the injuries.
Differential Diagnosis
Birth trauma: Intraretinal hemorrhages may be seen in newborns, especially with the use of forceps in the delivery. These hemorrhages resolve over the course of weeks and are often not associated with neurologic sequelae.
Leukemia and intraocular infections may also mimic the ocular findings of shaken baby syndrome.
Diagnostic Evaluation
Clinical examination: Evaluation for delayed neurologic development and systemic signs of child abuse
Head CT to evaluate for intracranial hemorrhage
Bone scan is more sensitive in detecting fractures and exposes the child to less radiation while providing a whole body skeletal survey. Bone scan findings may tailor subsequent x-ray studies.
X-ray studies: Fractures at different stages of healing, leg fractures prior to bipedal ambulation (prior to 12 months of age), and posterior rib fractures are highly suspicious for child abuse.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree