Peripheral Retinal Disease
James F. Vander
Retinal Break or Tear
Retinal break or tear describes a full-thickness defect in the retina, generally in the retinal periphery, although the break may occur anywhere. Breaks occurring as the result of vitreous traction are known as retinal tears.
Epidemiology and Etiology
Retinal breaks are common. They are more frequent in myopia, pseudophakia, and after trauma.
Many cases are bilateral and multiple.
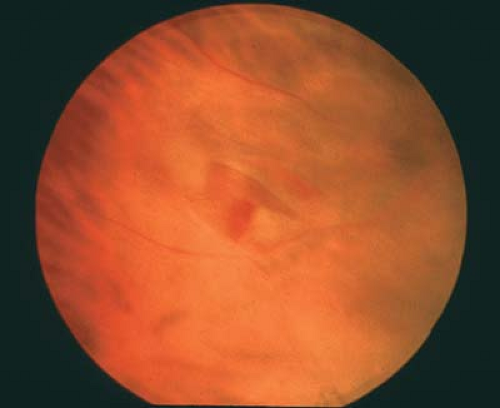
Retinal tears are caused by vitreous traction, most commonly found with degenerative vitreous liquefaction and posterior vitreous detachment (Fig. 9-1). Other retinal breaks (see later discussion) result from developmental or degenerative abnormalities or trauma.
History
Retinal tears are often associated with floaters and flashing lights (photopsia).
Many breaks are asymptomatic.
If associated with retinal detachment (RD), then progressive visual field loss occurs.
Important Clinical Signs
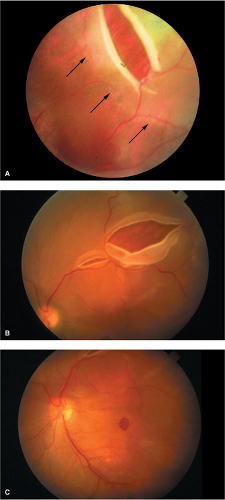
Types of retinal breaks
Horseshoe (flap) tears: The horseshoe is open anteriorly. Vitreoretinal traction often persists (Fig. 9-2).
Operculated tears: A fragment of retina is torn completely free of the retina and floats above it. The vitreous traction is relieved (Fig. 9-3).
Atrophic retinal break: Usually round, often small, holes; not associated with traction (Fig. 9-4).
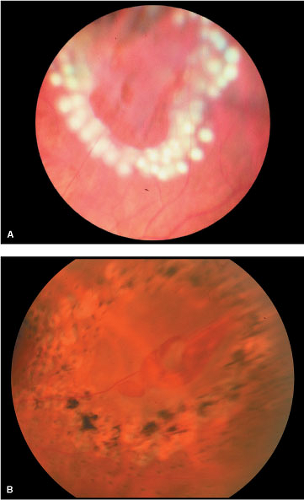
Retinal dialysis: Disinsertion of the retina from the pars plana at the ora serrata; most often inferotemporal; superonasal is virtually pathognomonic for trauma (Fig. 9-5).
Giant tear: A tear greater than 90 degrees, spontaneous or posttraumatic (Fig. 9-6).
Stretch/necrotic tears: Traumatic tears of variable size, often irregular in orientation with jagged edges; hemorrhage or other signs of trauma (Fig. 9-7).
Associated Clinical Signs
Look for predisposing conditions (see earlier discussion)
Pigment cells in the vitreous (“tobacco dust”)
70% with hemorrhagic posterior vitreous detachment (PVD)
Vitreous hemorrhage [tears are found in 70% of patients with hemorrhagic proliferative vitreoretinopathy (PVR)]
Subretinal fluid accumulating around the tear
Pigment around the base of the retinal break (indicates chronicity)
Differential Diagnosis
Vitreoretinal tuft
Meridional fold or complex
Outer wall hole in retinoschisis
Cobblestone degeneration
Lattice degeneration
Diagnostic Evaluation
Indirect ophthalmoscopy with scleral depression is critical.
Contact lens examination of the periphery may help confirm the presence and nature of the break.
Prognosis and Management
The risk of developing RD (and, therefore, indication for prophylactic treatment) depends on the type of break present. Symptomatic tears with persistent traction (horseshoe tears, giant tears) have a high risk of subsequent RD and are treated when recognized. Asymptomatic flap tears have a lower risk but are often prophylactically treated. Symptomatic operculated tears also have a much lower risk of subsequent RD.
Treatment is more controversial. Dialysis and other posttraumatic tears are generally treated when recognized. Treatment for atrophic breaks, asymptomatic operculated tears, and breaks with pigment around them almost never require prophylactic treatment. Exceptions might include patients with a history of RD of the fellow eye, anticipated cataract surgery, or a strong family history of retinal tears or RD.
Treatment options include cryotherapy or laser photocoagulation (Figs. 9-8–9-10). Development of the indirect ophthalmoscopic laser delivery system has facilitated the use of laser treatment and reduced the need for cryotherapy, which generally produces more pain during treatment. Patients with cloudy media or significant subretinal fluid may be better treated with cryotherapy.
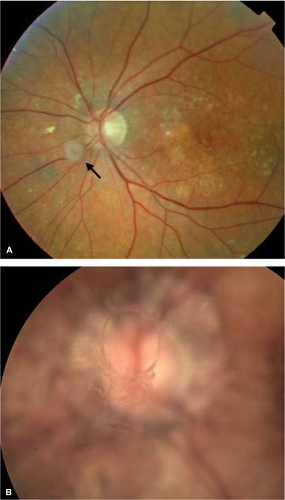 Figure 9-1. Posterior vitreous detachment (PVD). A. Annulus of condensed vitreous (Weiss ring) (arrow) floating in front of the optic disc after PVD. B. Photograph focused on Weiss ring. |
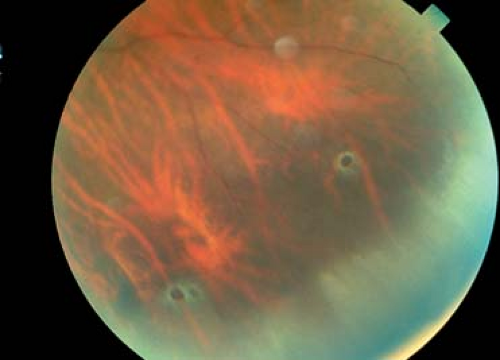 Figure 9-4. Peripheral cystoid degeneration. Peripheral cystoid degeneration with associated atrophic retinal holes. |
 Figure 9-5. Retinal dialysis. Wide-angle view of inferotemporal dialysis with associated retinal detachment. |
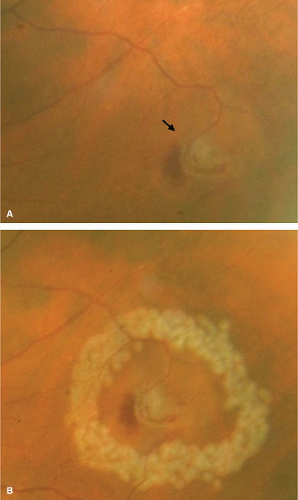 Figure 9-8. Retinal tear, pretreatment and posttreatment. A. Small horseshoe tear (arrow). B. Immediately after laser photocoagulation. |
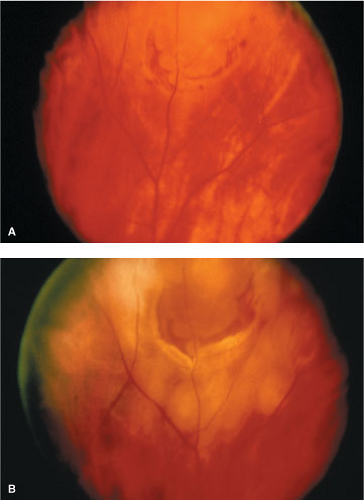 Figure 9-9. Retinal tear, pretreatment and posttreatment. A. Horseshoe tear with bridging vessel. B. Immediately after laser photocoagulation. |
Rhegmatogenous Retinal Detachment
Rhegmatogenous RD is a separation of the retina from the underlying retinal pigment epithelium (RPE) by fluid that gains access to the subretinal space via one or more full-thickness retinal breaks.
Epidemiology and Etiology
Epidemiology is the same as that for retinal breaks since, by definition, a retinal break is present and the cause of the RD.
Retinal breaks develop into rhegmatogenous RD by a combination of vitreoretinal traction and fluid currents that cause vitreous fluid to move through the retinal break(s) and overcome the normal attractive forces between the photoreceptors and the RPE.
History
There is a progressive loss of the visual field (often described as a curtain or shadow blocking the vision), frequently accompanied or preceded by floaters and flashing lights.
Patients with peripheral RDs may be asymptomatic or simply have flashes and floaters.
Important Clinical Signs
In addition to identifying the retinal break(s), the retina is seen to be elevated by subretinal fluid (Fig. 9-11). The retina loses its transparency to a variable degree, often becoming translucent with a corrugated appearance. There is undulation with eye movement. Chronic rhegmatogenous RD may appear transparent and not undulate.
Identifying the retinal break (often small and difficult to find) is the key. Pseudophakic RDs are often caused by small, pinpoint retinal holes at the vitreous base and may be difficult to detect.
Associated Clinical Signs
Pigment: Granules in the vitreous are almost always seen. Hyperpigmentation or loss of pigment at the RPE is common, especially in chronic RD. Linear pigment (“demarcation line”) suggests chronicity and may be multiple (Fig. 9-12).
Hypotony: Relative to the fellow eye. This is not invariably present. In chronic rhegmatogenous RD, pressure may be normal or even high.
Other features of chronic RD: Retinal neovascularization, cataract, anterior uveitis, rubeosis iridis, and retinal cysts (Fig. 9-13).
Differential Diagnosis
Retinoschisis
Exudative RD
Tractional RD
Choroidal detachment
Diagnostic Evaluation
Indirect ophthalmoscopy with scleral depression is the key. Contact lens examination may help find small peripheral retinal breaks.
Slit-lamp examination of the anterior vitreous confirms vitreous pigment.
B-scan ultrasonography confirms retinal elevation in cases with media opacities.
Examine the fellow eye to look for retinoschisis.
Prognosis
Chronic, asymptomatic RD may remain stationary and not require treatment.
Spontaneous regression of RD can occur but is rare (Fig. 9-14).
Most RDs and virtually all symptomatic detachments will progress, causing severe permanent visual loss if untreated. Visual potential is directly related to the presence and duration of macular involvement (Fig. 9-15).
RDs not involving the macula often recover vision fully.
“Macula-off” RDs usually lead to permanent reduction of central vision even when repaired properly. Recovery often takes months, and the degree of recovery diminishes with longer periods of macular detachment.
Management
Laser photocoagulation: Used alone it has a limited role in management of RD. Usually it cannot seal a retinal break closed in the presence of subretinal fluid. Laser treatment may be used to create a barrier (“wall off the detachment”) to prevent progression of the detachment. It is especially useful in chronic inferior RD or in cases where systemic illness prevents more definitive repair.
Cryotherapy (see preceding discussion of Laser Photocoagulation): Occasionally RDs with very shallow fluid around the retinal break can be cured by treating the break with cryotherapy alone.
Pneumatic retinopexy: An intravitreal gas bubble is used to tamponade the retinal break closed temporarily. The subretinal fluid will resolve and either laser photocoagulation or cryotherapy is used to permanently close the retinal break(s). The success rate is high and varies with patient selection. Patients with phakic RDs with a single, superior retinal break without vitreous hemorrhage, extensive lattice degeneration, or early PVR do best. This relatively noninvasive, low-cost, quick-recovery office procedure is gaining in acceptance.
Temporary balloon: This treatment consists of an external device applied via small conjunctival incisions. The balloon temporarily indents the sclera to allow cryotherapy or a laser-induced chorioretinal adhesion to form. This treatment option is especially useful for inferior RD when pneumatic retinopexy is not an option; however, it is not a widely used technique.
Scleral buckle: This widely applied technique consists of indentation of the sclera using a flexible silicone sponge or strip that is permanently sutured on or within the sclera to relieve vitreoretinal traction on the retinal break(s). Cryotherapy is generally used to create permanent adhesion although postoperative laser therapy can be applied. Drainage of subretinal fluid or injection of intravitreal gas, or both, are also sometimes performed to assist in reattachment. Success rates of over 95% have been reported for repair of primary RD. Side effects and complications of the scleral buckle include:
Pain
Infection
Hemorrhage (especially with drainage of subretinal fluid; Fig. 9-16)
Retinal incarceration at drainage site (Fig. 9-17)
Induced myopia
Diplopia
Extrusion or intrusion (Fig. 9-18)
Anterior segment ischemia
Ptosis
Vitrectomy: This technique is increasingly used in managing primary RD with or
without a scleral buckle. It allows for direct release of vitreoretinal traction. Intravitreal gas or silicone oil is used to tamponade the retina while retinopexy with laser or cryotherapy takes effect. Vitrectomy is especially useful for RDs with posterior breaks, PVR, vitreous hemorrhage, or a tight orbit preventing scleral buckle. Side effects and complications of vitrectomy include:
Elevated intraocular pressure
Cataract
Dislocation of intraocular lens
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree