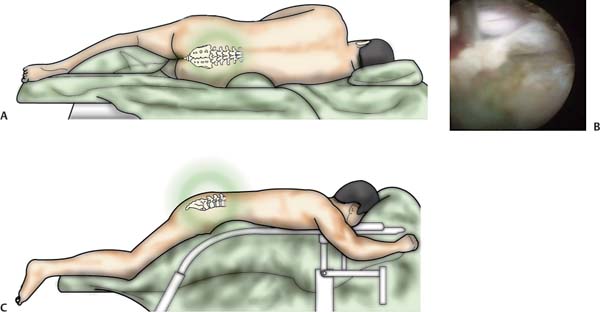
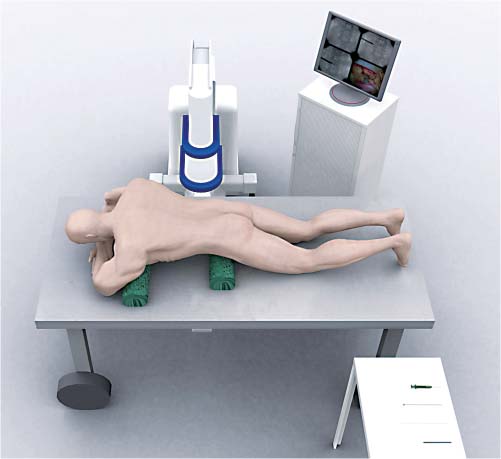
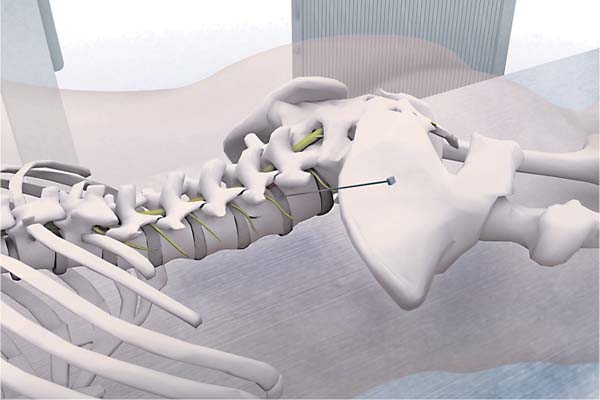
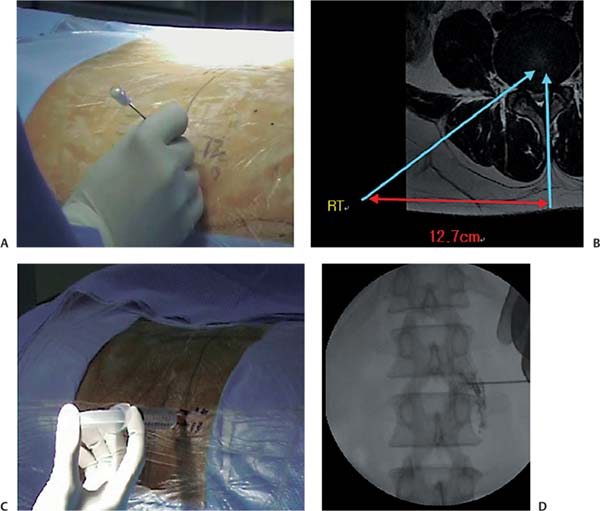
14 Transforaminal Surgical Approach • Percutaneous endoscopic lumbar diskectomy (PELD) is performed under local anesthesia with the patient in the prone position on a radiolucent table under guidance of C-arm fluoroscopy (Figs. 14.1 and 14.2). Conscious sedation with midazolam and fentanyl allows continuous feedback from the patient during the entire procedure to avoid causing damage to neural structures. • Midazolam is administered in the dose of 0.05 mg/kg intramuscularly a half hour before surgery followed by another dose intravenously during surgery if required. F entanyl dosage is 0.8 μg/kg intravenously 10 minutes before surgery followed by additional doses intraoperatively. • Axial magnetic resonance (MR) or computed tomographic (CT) images are used to calculate the distance of the skin entry point of the needle from the midline, the needle trajectory aimed to target the ruptured fragment while avoiding the contents of the peritoneal sac. • Inclination of the needle trajectory: The needle is directed 10 degrees downward and inclined to make an angle of ~10 degrees with the lower or upper end plate, respectively (Fig. 14.3). • In cases where a minor directional adjustment is necessary, the use of the plane of the needle bevel is needed (if the needle bevel is facing dorsal, the needle will tend to move ventral when being advanced). • The first bony resistance encountered is the lateral facet. The end of the needle should be elevated so that the tip of the needle can go deeper, passing under the ventral side of the facet, and the approach should be continued toward the foraminal annular window (Kambin’s triangle). Turning the needle bevel to face dorsal helps the needle tip skives off the undersurface of the facet. The C-arm guidance is mandatory during this step. Fig. 14.1 (A–C) Position of patient. Fig. 14.2 Position of patient, C-arm, and endoscopic instrument. • It is imperative to achieve proper placement of the needle, which is facilitated by complying with the following guidelines. Local anesthesia (1% lidocaine) is used in the needle skin entry point. Liberal use of local anesthesia at the site of the skin entry as well as the tract of the intended trajectory is very useful in carrying out the procedure. In addition, epidural infiltration of 6 to 8 mL of the local anesthetic can also be done. The epidurography is performed by injecting 1 to 2 mL of a radiopaque dye (Telebrix, Guerbet, Aulnay-Sous-Bois, France) to check the exiting nerve root and the dural sac in the fluoroscopy (Fig. 14.4). • The site of annular puncture by the needle tip should be the medial pedicular line in the anteroposterior view and the posterior vertebral line in the lateral view of the fluoroscopic imaging. This corresponds to the Kambin safe triangle in the axillary area between exiting and traversing nerve roots. The midpedicular line should be considered for upper lumbar disk herniations (L3–L4 and above) to avoid neural injury because the dural sac is bigger with more nerve tissue, lying more laterally due to the narrow width of the pedicles at the upper levels (Fig. 14.5). • Diskography is performed by injecting 2 to 3 mL of a mixture of radiopaque dye (Telebrix), indigo carmine (Carmine, Korean United Pharma, Seoul, South Korea) and normal saline mixed in 2:1:2 ratios. The dye leaks through the tear in the annulus into the epidural space with the direction being concordant with the anatomical location of the ruptured fragment. Indigo carmine, being a base, selectively stains the degenerated acidic nucleus blue, and it helps for identification of the herniated fragment during endoscopic visualization (Fig. 14.6). Fig. 14.3 Needle insertion technique Fig. 14.4 (A–D) Needle insertion and epidurography. (A) Trajectory of needle insertion is decided with MRI. (B) The needle is inserted 12.7 cm from midline. The epidurography is performed by injecting 1 to 2 mL of a radiopaque dye (C.
Step One: Position and Anesthesia
Step Two: Skin Entry Point
Step Three: Needle Insertion T echnique and Epidurography
Step Four: Diskography
![]()
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree