Toxic Anterior Segment Syndrome
Nick Mamalis
Henry F. Edelhauser
Zachary M. Bodnar
Toxic anterior segment syndrome (TASS) is an acute, sterile postoperative anterior segment inflammation following any anterior segment surgery. By definition, TASS is sterile or noninfectious. This entity was initially described as sterile postoperative endophthalmitis, but in 1992, Monson et al.1 accurately termed this condition “toxic anterior segment syndrome.” In addition, cases of TASS, which are characterized by localized corneal endothelial damage, have been termed “toxic endothelial cell destruction syndrome (TECDS).”2,3,4,5,6 TASS has been thoroughly discussed in a review/update paper and its accompanying editorial, as well as a clinical module for ophthalmologists.7,8,9
TASS most commonly occurs acutely following anterior segment surgery, but in rare instances, can have a delayed onset. The postoperative inflammation is sterile or noninfectious and is felt to be secondary to a toxic substance of some kind that enters the anterior segment either during or immediately after anterior segment surgery, causing inflammation. A recent retrospective case series from the Aravind Eye Hospital in India reported an incidence of 0.22% (60 eyes out of 26,408 cataract surgeries).10
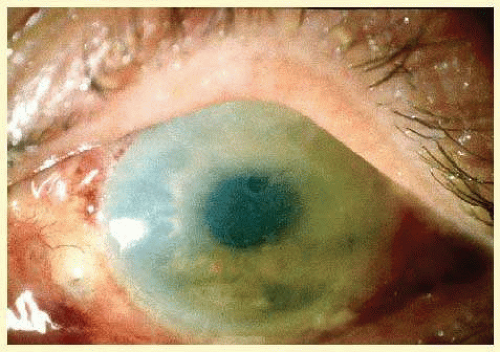
The most common symptom of TASS is blurry vision. Pain is usually absent from patients with TASS in distinction to those with postoperative infectious endophthalmitis, most of whom will experience pain. The hallmark of TASS is that the inflammation usually has a relatively immediate onset, certainly within 12 to 48 hours of surgery. The most common clinical finding is a diffuse corneal edema that has been described as “limbus-to-limbus” corneal edema (Fig. 4.1). This diffuse edema results from the widespread damage of corneal endothelial cells. This pattern differs significantly from the focal corneal edema that is often seen following cataract surgery.
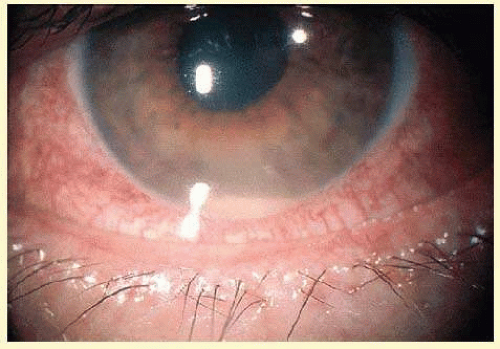
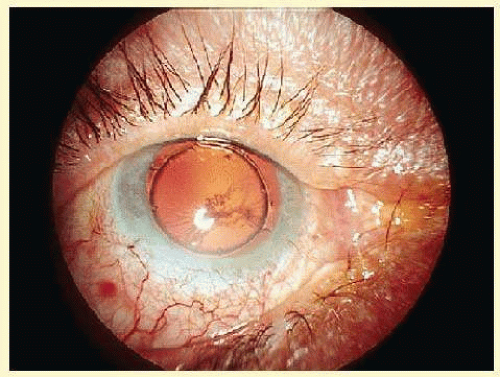
Another signature feature of TASS is marked anterior segment inflammation (Fig. 4.2). This is characterized by a diffuse breakdown of the blood-aqueous barrier with increased inflammatory cells in the anterior chamber. Many cases will develop a hypopyon. In addition, fibrin may form across the pupil, iris, and surface of the intraocular lens (IOL), and inflammatory keratitic precipitates may be present. This syndrome can result in damage to the iris, which can cause a permanently dilated, irregular, and/or atrophic pupil. If the inflammation is severe, damage to the trabecular meshwork and formation of peripheral anterior synechia may occur, leading to a difficult-to-control glaucoma (Fig. 4.3).
It is important to differentiate the sterile inflammation seen in TASS from an infectious postoperative endophthalmitis. One of the features that is most helpful in differentiating these two entities is that TASS almost always presents within the first 24 to 48 hours, whereas the typical signs of bacterial endophthalmitis generally appear between 4 and 7 days, postoperatively, although a recent study by Moshirfar et al.11 suggests that the time to presentation may often be longer, with an average of 9.3 days between the day of cataract surgery and the diagnosis of endophthalmitis. There are also differences in symptomatology. Greater than 75% of patients who have an infectious endophthalmitis will have pain, but most cases of TASS are pain free. The anterior segment inflammatory changes in both of these entities are often very similar, with significant inflammation and hypopyon formation, but vitreous involvement is much more typical of endophthalmitis. When the vitreous is involved in TASS, it is usually in the form of a moderate spillover from the anterior chamber. Also, the diffuse corneal edema, which is typically seen in TASS, is not often present in an infectious endophthalmitis. These clinical differences are not absolute, however, and when there is any suspicion of an infectious etiology, anterior chamber and vitreous samples should be taken for staining, culture, and PCR.
ETIOLOGY OF TASS
Any substance used during or immediately after cataract surgery that can obtain access to the anterior segment of the eye can cause TASS. This includes medications, anesthetics, antibiotics, and solutions that are used, in general. TASS is characterized by a toxic reaction that causes damage to the anterior segment of the eye. The corneal endothelium is especially sensitive to any toxins.
The etiology of TASS is broad and may include problems with the irrigating solutions such as balanced saline solution (BSS).12,13,14,15,16 Any ophthalmic solutions that contain preservative or stabilizing agents of any kind can be toxic to the corneal endothelium and may cause TASS.16,17,18 Intraocular medications, such as antibiotics and anesthetics, are a potential source of TASS. In addition, residues of ophthalmic viscosurgical devices (OVD) or retained cortical material can cause significant postoperative inflammation.19 TASS may also be caused by contaminants introduced during surgery or the instrument cleaning process such as bacterial endotoxin, talc, or the chemical releasing agent from surgical gloves, heavy metals, or water contaminants.20 Lastly, it is important to remember that any enzymes or detergents that are used in the sterilization of instruments used in anterior segment surgery can leave a residue that could cause TASS.21,22,23
Intraocular Irrigating Solutions
Intraocular irrigating solutions, such as BSS, have the potential to cause TASS if problems exist with their composition such as incorrect ionic concentrations, overall osmolarity, or pH.12,13,14,15,16 The pH of BSS, ocular solutions, and medications should be in the range: 6.5≤ pH ≤ 8.5. The acceptable range for osmolarity is ≥270 to ≤340 mOsm. An outbreak of TASS in the fall of 2005 was found to be secondary to endotoxin contamination of BSS. A thorough investigation of the 112 cases from this outbreak by investigators from the Intermountain Ocular Research Center at the University of Utah as well as investigators from the U.S. Centers for Disease Control and Prevention (CDC) found that most patients were exposed to one particular brand of BSS used during cataract surgery.
Several lots of this brand of BSS were found to have levels of endotoxin that exceeded the allowable limit of 0.5 EU per mL. The BSS was withdrawn from the market, which resulted in termination of the outbreak.24
TASS may also be caused by epinephrine, antibiotics, or other solutions that are added to the BSS. Epinephrine that is added to the BSS should be both free of preservatives and stabilizing agents, as these agents are known to be toxic and have been implicated in outbreaks of TASS. Antibiotics that are added to the BSS have the potential to cause TASS if improperly prepared. For this reason, in addition to unproven efficacy at preventing endophthalmitis, mixing antibiotics into the BSS solution is not recommended.
Preservatives And Stabilizing Agents
The corneal endothelium is extremely sensitive to preservatives used in many of the topical ophthalmic drops or solutions. One of the most commonly used preservatives is benzalkonium chloride (BAK). There have been multiple reports of patients with significant corneal edema or endothelial cell damage resulting from solutions preserved with BAK.5 In addition, BAK has been found to cause significant corneal edema when used as a preservative within an OVD.6 Low levels of BAK are safe to use on the surface of the eye, but should be avoided in medications that gain access to the eye during the anterior segment surgery.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree