CHAPTER 138 Topical Therapies of External Ear Disorders
History
Topical therapies have been used to manage external ear disorders for thousands of years. According to Myer,1,2 mixtures including red lead, tree resin, olive oil, frankincense, goose grease, cream from cow’s milk, crushed soda, vermilion, cumin, ass ear, and hatet oil were used to treat chronic draining ears 3500 years ago. A process known as “ear candling” dates back more than 1000 years and was originally adopted as a method of removing cerumen from the canal. In this process, a hollow candle is lit on one end creating a vacuum at the other end that, when inserted into the ear, draws out debris from the canal. Contemporary studies have shown that ear candling is largely ineffective, and this technique can deposit hot candle wax into the canal, resulting in burns.3 In the 1800s, “rattlesnake oil” (turpentine, camphor, menthol, and sassafras) was marketed as a cure for otorrhea.
By the early 1900s, astringents and alcohols were introduced, and the acidity and high alcohol concentration made these preparations effective if given early in the course of an infection. They had no targeted antimicrobial activity, however. Topical antibiotics and antifungals against the most common pathogens associated with OE and otitis media were not developed until the mid-20th century.1,2 In particular, ototopical aminoglycosides have been available for more than 20 years and are still frequently prescribed; newer fluoroquinolone agents are gaining in popularity because studies have shown potentially less ototoxicity associated with their use.3,4
Mechanism of Action
The external auditory canal is lined with squamous epithelium, providing a natural barrier against the environment. The successful delivery of topical medications requires penetration across this barrier, and the stratum corneum (the most superficial layer of the epidermis) provides the greatest resistance to the permeation of drugs.5 Passive diffusion allows for most of the transport across the stratum corneum, and the degree of absorption is related to the properties of the agent being used.5 Two routes of passive diffusion across the stratum corneum have been proposed: transappendageal and epidermal.6 Because only 0.1% of skin area is composed of appendages such as hair follicles and sebaceous glands, the epidermal route is thought to be the more important route of drug permeation.5,6 Topical medications can diffuse through the epidermis transcellularly or intercellularly.6 Transcellular transport is used by hydrophilic drugs, whereas intercellular diffusion occurs with lipophilic compounds.5,6 The agent or vehicle used in a particular ototopical agent will affect its absorption and diffusion across the epidermis.
Topical Antibiotics
Extremely high local concentrations (3000 µg/mL for a 0.3% otic solution) of ototopical antibiotics can be achieved in the external canal. The minimum inhibitory concentrations (MICs) for antibiotics against common pathogens associated with external ear infections are typically less than 100, but can be in the mid-200’s for resistant Pseudomonas.7,8 The local concentrations associated with ototopicals are significantly higher than MICs for all pathogens that have been isolated from external ear infections, including resistant organisms.7,8 In contrast, the local concentration of antibiotics in the middle ear after oral administration of amoxicillin, erythromycin, azithromycin, or cefixime (given in standard adult doses) may not be more than the MICs for the offending organisms, ranging from 1 to 15 µg/mL, although the concentration can be 35 µg/mL for intravenous ceftriaxone.7,9–11 These levels were observed 4 hours after oral administration in human subjects and were measured in middle ear fluid samples obtained using tympanocentesis. No studies have examined the concentrations of antibiotics given systemically in the external ear; however, it is unlikely that they would be vastly different from the concentrations observed in the middle ear.
Topical Anti-inflammatories
The most commonly used prescription anti-inflammatories for external ear conditions also include an antibiotic or antifungal, although occasionally an otolaryngologist may prescribe a topical steroid alone for chronic pruritus or eczema. Most of the current understanding of how the steroid component of these preparations is absorbed regionally through topical application can be found in the dermatologic literature. The efficacy of a particular steroid preparation is associated with the inherent potency of the compound and its ability to penetrate the epidermis.12 Lipophilic (nonpolar) preparations are transported across the stratum corneum more effectively than hydrophilic (polar) molecules.12 The stratum corneum can also act as a reservoir for topical steroids, allowing for a prolonged regional effect after therapy is stopped.5,12 Vehicles such as ethanol or propylene glycol increase the solubility of a topical agent to enhance permeability.12 The hydration of the stratum corneum can also be enhanced by using occlusive vehicles such as ointments that improve drug penetration.12
Acute Bacterial Otitis Externa
See Chapter 137 for a definition and description of acute bacterial OE.
Topical Therapy Options for Acute Bacterial Otitis Externa
The most common bacterial pathogen is Pseudomonas aeruginosa, followed by Staphylococcus aureus, gram-negative bacteria, and anaerobes.13–15 Treatment of acute OE often involves topical antibiotic preparations, with or without steroids. In mild acute or chronic OE, or as a preventive measure, acidifying agents may be used. Systemic antibiotics are indicated in severe or refractory cases, or in patients who are immunocompromised. Regardless of the therapy chosen to treat acute OE, removal of debris from the external canal and evaluation of the status of the tympanic membrane is crucial before using any ototopicals,14,16–18 and oral analgesics are often needed in moderate or severe cases. Repeat débridement of the canal under binocular microscopy is essential to improve an infection that remains refractory to ototopical therapies.
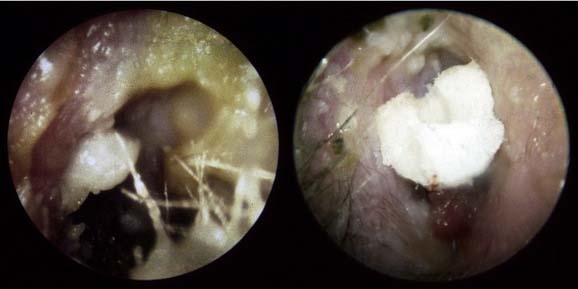
In cases where the canal is extremely edematous, it may be impossible to visualize the tympanic membrane—care should be taken in this instance to avoid the use of ototopicals with potential ototoxic side effects.16 Significant swelling and edema also requires wick placement to ensure proper delivery of ototopical antibiotics medially in the canal (Fig. 138-1). The wick should be changed or removed within 3 to 5 days of its insertion. If the canal is patent, tragal massage helps deliver the medication to the medial external auditory canal, and holding the head in a dependent position for several minutes allows for sufficient filling of the infected cavity.
Ototopical Antibiotics
Ototopical antibiotic preparations, with or without steroids, are the most common agents used to treat acute OE in the otolaryngology office. These preparations achieve local tissue concentrations approximately 1000 times that of systemic antibiotics, have a favorable side-effect profile, and show a lower incidence of bacterial resistance compared with systemic antibiotics.7,14 The American Academy of Otolaryngology–Head and Neck Surgery Foundation (AAO-HNSF) developed a Clinical Practice Guideline in 2006 for the treatment of OE. The group made firm recommendations to use “topical preparations for initial therapy of diffuse, uncomplicated [acute OE]; [systemic] antimicrobial therapy should not be used unless there is extension outside of the ear canal or the presence of specific host factors that would indicate a need for systemic therapy” (e.g., diabetes, prior radiotherapy, or immunocompromise).16
The following are commonly used preparations for the topical management of acute OE:
Evidence-based Data on Ototopical Antibiotics in Acute Otitis Externa
Roland and colleagues28 performed one of the few randomized multicenter studies comparing ototopical antibiotics. The clinical efficacy of 1 week of ciprofloxacin/dexamethasone (Ciprodex) or neomycin/polymyxin B/hydrocortisone (Cortisporin) was studied in 468 adults and children with acute OE and intact tympanic membranes. Ciprofloxacin/dexamethasone showed higher bacterial eradication rates and more rapid symptom improvement compared with neomycin/polymyxin B/hydrocortisone. Rahman and coworkers34 also compared the efficacy of Ciprodex and Cortisporin drops in 1072 adults and children with acute bacterial OE in a multicenter, randomized, prospective, blinded trial. Cortisporin dosed three times daily and Ciprodex dosed twice daily for 7 days resulted in a 98% cure rate at 18 days for Ciprodex and a 97% cure rate for Cortisporin. The time to cure was 0.6 days shorter for Ciprodex.34
van Balen and associates35 performed a randomized clinical trial of ototopical therapies that compared acetic acid alone, acetic acid and corticosteroid, and antibiotic and corticosteroid for acute OE. In 213 adults with acute OE, patients who received preparations that included steroids (either acetic acid or antibiotics) had significantly higher cure rates compared with acetic acid alone.35 The acetic acid–alone group also had higher recurrence rates of OE.35 Schwartz36 performed a randomized multicenter blinded study in which patients with acute OE received either ototopical ofloxacin administered once daily or neomycin/polymyxin/hydrocortisone administered four times daily. In 278 pediatric patients with pseudomonal OE, both agents were equally effective at eradicating disease and had similar safety profiles.36 Given the decreased ototoxic potential of ofloxacin and the easier dosing schedule, the authors concluded that ofloxacin might be a better first-line agent,36 although neomycin/polymyxin/hydrocortisone is significantly less expensive than ofloxacin. The same conclusion was reached by Simpson and Markham24 in a meta-analysis of the literature concerning ofloxacin use for acute OE.
Rosenfeld and colleagues37 found 18 studies concerning ototopical therapy for acute OE that compared any of the following groups: antimicrobial versus placebo, antiseptic versus antimicrobial, fluoroquinolone antibiotic versus antibiotic, steroid/antimicrobial versus antimicrobial, or antimicrobial/steroid versus steroid. Clinical cure rates were 65% to 80% within 10 days of therapy with all of the above-mentioned ototopical antibiotics, and there was no statistical difference in clinical cure rates among any of the treatment groups.37 Fluoroquinolones did have an 8% higher bacteriologic cure rate compared with nonquinolone ototopicals; however, the clinical cure rate and rates of adverse side effects were the same as those of the other preparations.37 The addition of a steroid to fluoroquinolone agents decreases the symptomatic period by approximately 0.8 days1,3 As discussed subsequently, however, steroids do have a small risk of causing a hypersensitivity reaction.
Resistance Associated with Ototopical Antibiotic Therapy
Weber and colleagues38 found that there is overall grade B evidence (at least fair scientific evidence suggests that the benefits of the clinical service outweigh the potential risks) that no significant antibiotic resistance develops from the use of ototopical antibiotic therapy. Cantrell and colleagues19 examined the susceptibility of isolates from acute OE to neomycin/polymyxin and ofloxacin. The MICs of each antimicrobial drug for the major pathogens (Pseudomonas and Staphylococcus aureus), bacterial eradication, and clinical efficacy were studied from 1995-1996 and from 1999-2000.19 The MICs for all pathogens increased above the breakpoint for polymyxin B in the data from 1999-2000, but the MICs of all isolates for ofloxacin remained similar between the two time periods, indicating that resistance developed to neomycin/polymyxin, but not to ofloxacin.19 In 2003, Wai and Tong25 noted that minimal resistance had been documented against ofloxacin since its initial use in the 1980s, and mentioned that only two strains of Pseudomonas have been shown to have slight resistance to ofloxacin. Contrary to these findings, Jang and Park39 examined 88 patients with chronic suppurative otitis media that was refractory to treatment with topical ciprofloxacin and found that Pseudomonas isolates in all cases were resistant to topical ciprofloxacin. There is still ongoing concern and debate over the possibility of bacterial resistance to Cortisporin and ofloxacin drops, and this is an area that needs to be studied further in years to come. At this time, owing to extremely high local concentrations achieved with topical therapies that far exceed even the highest MICs for resistant Pseudomonas, it is unlikely that resistance would be a large factor in the choice of ototopical antibiotics.
Acidifying Agents in Acute Bacterial Otitis Externa
Acidifying agents may be used in mild acute or chronic cases of OE where there is minimal otalgia, but their main usefulness is in the preventive care of patients prone to developing recurrent acute or chronic OE (e.g., swimmers, hearing aid users). Alkaline pH has been shown to be a risk factor for the development of acute and chronic OE40,41; restoring the natural acidity of the external canal can inhibit the growth of bacteria responsible for OE. The acidic pH of these preparations may also limit patient compliance because of pain and local irritation.18 These agents are contraindicated if a tympanic membrane perforation or tympanostomy tube is present because of possible ototoxicity.3,42
 alcohol,
alcohol,  white vinegar, and
white vinegar, and  distilled water. Typically, several drops (4 to 5) are used in the affected ear two to four times daily until symptoms resolve and can be easily delivered with a syringe. This solution is contraindicated in patients with tympanic membrane perforations or ventilation tubes, or if the patient has a hypersensitivity to any of the components.
distilled water. Typically, several drops (4 to 5) are used in the affected ear two to four times daily until symptoms resolve and can be easily delivered with a syringe. This solution is contraindicated in patients with tympanic membrane perforations or ventilation tubes, or if the patient has a hypersensitivity to any of the components.Systemic Therapy for Acute Bacterial Otitis Externa
The AAO-HNSF recommends adding a systemic antibiotic in patients with OE and a history of prior radiation therapy, diabetes, or immunocompromised state.16 Patients with concomitant parotitis or cellulitis extending to the auricle, face, or neck, and patients with concurrent otitis media without tympanic membrane perforation or tympanostomy tube also should receive oral antibiotics. Finally, patients who fail to respond to a full course of ototopicals may benefit from oral antibiotics.7,15,16,18 It may be prudent to obtain a culture in patients with refractory OE before starting oral antibiotics, or before starting topical therapy in patients with underlying immunocompromise.
Special Considerations in Chronic Bacterial Otitis Externa
When initial therapy fails to treat acute OE, the physician should consider not only the possibilities of improper administration or ineffectiveness of the ototopical, but also other possible diagnoses, such as malignant OE, underlying canal cholesteatoma, keratosis obturans, contact dermatitis, and malignancy (Table 138-1).14 Symptoms lasting longer than 3 months may indicate chronic OE. This condition can be the result of inadequately treated infectious OE, but noninfectious causes should also be considered and are discussed subsequently in the section on eczematoid OE.14,44 In chronic OE, topical antibiotic therapies may not be as effective in resolving long-standing inflammation. Daily irrigation with an acidifying or dehydrating agent and use of a hair dryer on a low, cool setting after water exposure help to optimize daily ear hygiene. Dry powder preparations (discussed subsequently) are a reasonable alternative to topical drops because continued moisture from long-term ototopical use can contribute to maceration of the external canal skin and chronic infection. Topical steroid creams have been used with topical antibiotics to improve the efficacy of treatment in chronic OE.
Table 138-1 Considerations if Acute Otitis Externa Fails to Respond to Initial Ototopical Therapy
Ototoxicity Associated with Topical Antibiotics
The possible risk of ototoxicity with the use of topical antibiotics, particularly aminoglycosides (gentamicin, neomycin, streptomycin), continues to be a concern. Free radicals are generated by aminoglycosides in the inner ear that can injure vestibular and cochlear hair cells. Two mutations in the mitochondrial 12S ribosomal RNA gene have been reported to predispose carriers to aminoglycoside-induced ototoxicity.31 The vestibulotoxic and cochleotoxic side effects were initially recognized after systemic use of aminoglycosides, and subsequent research has examined their toxicity when used in topical form. Animal studies performed since the 1950s have consistently confirmed the ototoxic potential of topical aminoglycosides. Wright and Meyerhoff20 showed near-total destruction of all the hair cells in the inner ear of the chinchilla with only a single application of neomycin, polymyxin, or chloramphenicol.
No large randomized controlled trials examine the issue of ototoxicity from topical antibiotic therapy in humans. The data that do exist from human studies are equivocal, and the incidence of topical aminoglycoside–associated ototoxicity may be only approximately 1 in 10,000 patients.4,45 Possible explanations for this difference in ototoxicity between humans and animals are that humans have thicker round window membranes, a deeper round window niche (providing greater protection), and often a pseudomembrane (mucous membrane) overlying the round window that may minimize topical absorption.7 Polymyxin, a component of Cortisporin otic drops, has ototoxic properties in animal studies (even more so than neomycin), and may have ototoxic potential in humans in the presence of tympanic membrane perforations.20,46 In contrast to aminoglycosides and polymyxin, no ototoxicity from fluoroquinolones has been reported in animals or humans.25
In 2007, the Clinical Audit and Practice Advisory Group of the British Association of Otolaryngologists–Head and Neck Surgeons (ENT-UK) reviewed the literature with the goal of establishing a clinical guideline for the use of aminoglycosides in acute OE in humans. They found no convincing data regarding the ototoxicity of topical aminoglycosides, but recommended that these agents should be used only in the presence of obvious infection and for no longer than 2 weeks.47
Linder and associates48 examined 134 patients who were evaluated for possible ototopical antibiotic–related ototoxicity, and found only two patients with significant sensorineural hearing loss attributable to excessive administration of framycetin-containing and polymyxin-containing ear drops in the presence of tympanic membrane perforations. Matz and colleagues49 performed a review of the literature and found 14 articles that dealt directly with the evaluation of either hearing loss or changes in vestibular function after the use of ototopical antibiotic drops. Although most articles were in the level 3 to 3b evidence category (opinions of respected authorities based on clinical experience, descriptive studies, or reports of expert committees), two were in the 1b category (evidence obtained from at least one properly designed randomized controlled trial). Fifty-four cases of gentamicin-induced vestibular toxicity were documented, and cochlear toxicity was noted in 24 of these patients. Eleven cases of cochlear toxicity and 2 cases of vestibular toxicity associated with neomycin-based ototopicals were also observed.49
Berenholz and coworkers50 performed a retrospective review of 500 patients who received Cortisporin drops after ventilation tube placement. They found no cases of new-onset sensorineural hearing loss, and noted that Cortisporin drops were less than half as expensive as topical fluoroquinolones. A Cochrane Database article in 2006 addressed the safety concerns of ototopicals and found no adequate evidence to suggest ototoxicity for either Cortisporin or fluoroquinolone drops.51
A consensus panel of the AAO-HNSF made recommendations in 2004 on the use of topical aminoglycosides in the middle ear or in the presence of tympanic membrane perforation.4
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree