(1)
Department of Ophthalmology and Visual Sciences, University of Iowa Hospitals and Clinics, Iowa City, IA, USA
The orbital venous system is complex, highly variable, and confusing. In the orbit, unlike other parts of the body, there is no direct correspondence between the arteries and veins, except for the superior ophthalmic vein which has some correspondence with the ophthalmic artery. Also, the orbital veins, unlike the orbital arteries, have a highly variable and inconstant pattern and formation of venous networks at several places, resulting in marked uncertainty and controversy as to their number, nomenclature, and pattern. The latest detailed studies on the orbital venous system are those of Henry [1] and Cheung and McNab [2].
The orbital veins can be divided into two categories: (1) main veins and (2) inconstant veins.
1.
Main Orbital Veins
Superior ophthalmic vein: This is the largest orbital vein and is the principal route of orbital venous drainage. Anteriorly at the superomedial corner of the orbital margin, it is usually formed by the union of two veins – the supraorbital and angular – just posterior to the trochlea [2]. It runs posteriorly along with the ophthalmic artery and leaves the orbit through the superior orbital fissure to join the cavernous sinus. Therefore, like the ophthalmic artery, its intraorbital course can be divided into 3 parts (see Chap. 1). Main venous tributaries draining into it include the medial palpebral, superior vortex, anterior ethmoidal, lacrimal, central retinal, muscular, and inferior ophthalmic veins. Brismar [3], on orbital phlebography, has described the anatomy and variations of the superior ophthalmic vein. Its pattern on orbital phlebography has been used for diagnosis of orbital mass lesions; however, Brismar [3] cautions that since the pattern is not symmetrical between the two orbits, care must be taken in the diagnosis of space-occupying orbital lesions from the venous asymmetries.
Inferior ophthalmic vein: This usually originates at the anterior, medial part of the orbital floor, from a venous network draining the lower lid, lacrimal sac region, inferior vortex veins, and inferior rectus and oblique muscles. In most cases, the vein runs posteriorly close to the orbital floor on the surface of the inferior rectus muscle, to join either the superior ophthalmic vein or the cavernous sinus directly [4].
2.
Inconstant Orbital Veins
Middle ophthalmic vein: This vein was first described by Henry [1]. It drains the inferior network and runs posteriorly above the inferior rectus and between the superior and inferior ophthalmic veins. Some consider this as a second inferior ophthalmic vein because it is connected to the latter by collaterals [4]. It joins the superior ophthalmic vein. Cheung and McNab [2], however, did not find this vein.
Medial ophthalmic vein: Brismar [4] described this in 40 % of his orbital phlebograms. According to him, it arises from the angular vein or the anterior part of the superior ophthalmic vein, and runs backward along the orbital roof and medial wall, and enters the cavernous sinus. However, Cheung and McNab [2] reported that this vein has a very short course, running within the muscle cone and draining invariably into the superior ophthalmic vein.
Collateral veins: These essentially connect the superior venous system to the inferior venous system [2]. Sesemann [5] in 1869 was one of the first to describe them; according to him, they connect the superior ophthalmic vein with the inferior ophthalmic vein. In his anatomical studies, Henry [1] classified these into the following four types:
(i)
Anterior Collateral Vein: This runs along the medial wall of the orbit, connecting the anterior medial network at the orbital floor and the angular vein.
(ii)
Medial Collateral Vein: This is situated between the eyeball and medial rectus, connecting the anterior medial network at the orbital floor and the superior ophthalmic vein.
(iii)
Lateral Collateral Vein: This lies on the lateral side of the muscular cone, connecting the inferior venous network and the lacrimal vein.
(iv)
Posterior Collateral Vein: This is located in the posterior part of the orbit, connecting inferiorly located orbital veins and the superior ophthalmic vein.
On orbital phlebography, Brismar [3] found an anterior collateral vein in 91 % of eyes, medial in 97 %, lateral in 72 %, and posterior in 19 %.
Cheung and McNab [2] divided the orbital venous system essentially into superior and inferior orbital venous systems, with superior and inferior ophthalmic veins, respectively, comprising the two, with several variations. They described the presence of only two collateral veins – medial and lateral, connecting the superior and inferior venous systems.
Apart from those, there are orbital venous networks. Among them, the most widespread one is the inferior venous network, which has been further subdivided into an anteroinferior network, located in the muscle cone, and a posteroinferior network [1]. A superior network, located above the superior rectus and levator muscles, has also been described.
Apart from the above, there are named venous tributaries of the main veins; these include the palpebral, vortex, lacrimal, muscular, ethmoidal, and central retinal veins. The central retinal vein, which drains blood from the retina and optic nerve, may join the superior or sometimes the inferior ophthalmic vein, or even the cavernous sinus directly. In my study [6], I found that the central retinal vein, after emerging from the optic nerve, may run for some distance in the substance of the dural sheath. The development of optic nerve sheath meningioma at or near the site of exit of the central retinal vein from the sheath results in a gradual occlusion of the central retinal vein, and that may cause the development of typical retinociliary collaterals on the optic disc – a well-known sign of optic nerve sheath meningioma.
The intraorbital veins have multiple communications with the surrounding extra-orbital veins, e.g., anteriorly with the facial and frontal veins, posteriorly with the cavernous sinus, inferiorly with the pterygoid plexus, and medially with the nasal veins via the ethmoid veins.
Central Retinal Vein
The central retinal vein is the primary vein draining from the retina (Figs. 7.1 and 7.2). The postcapillary venules drain the blood from the capillaries, but occasionally capillaries may join a major branch retinal vein directly. The terminal arterioles and postcapillary venules are situated in an alternating pattern, with the capillary bed in between the two (Fig. 7.3). The postcapillary venules drain into bigger venules and finally into the branch retinal veins. The lumen of the major branch retinal veins, just before they join to form the central retinal vein, is about 200 μ. In the central part of the retina, the branch retinal veins and arteries usually run in close association and at places cross one another (Fig. 7.4). On the other hand, in the peripheral retina, the veins do not follow the course of the arteries. Various retinal arteries and veins in the retina cross each other at arteriovenous crossings (Fig. 7.4).
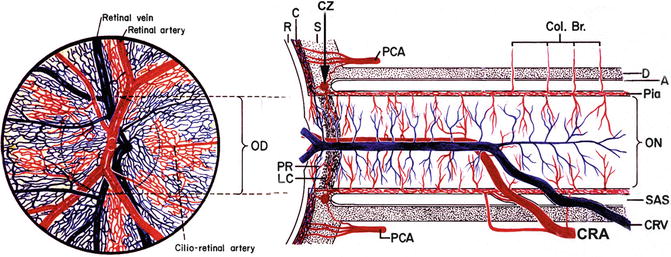
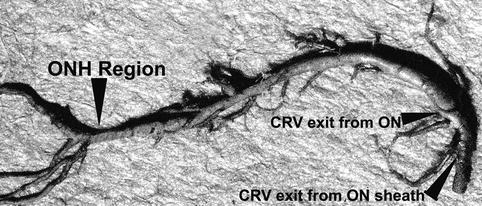
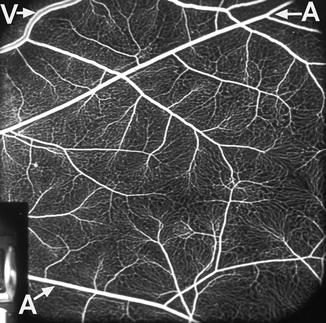
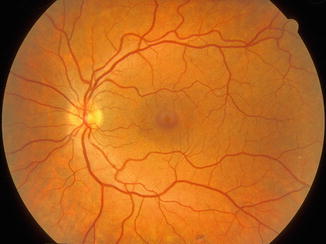
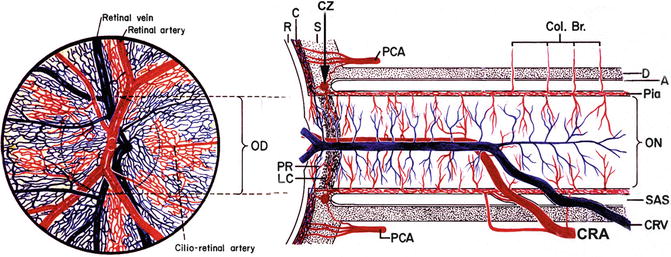
Fig. 7.1
Schematic representation of blood supply of the optic nerve (Modified from Hayreh [7]). Abbreviations: A arachnoid, C choroid, CRA central retinal artery, Col. Br. collateral branches, CRV central retinal vein, CZ Circle of Haller and Zinn, D dura, LC lamina cribrosa, OD optic disc, ON optic nerve, PCA posterior ciliary artery, PR prelaminar region, R retina, S sclera, SAS subarachnoid space
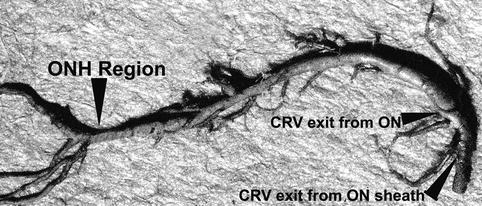
Fig. 7.2
Neoprene cast of the central retinal vein (CRV) in my study shows its entire course from the optic nerve head (ONH) to its exit from the optic nerve (ON) sheath. Note the presence of a large number of prominent venous tributaries within the optic nerve and none in the optic nerve head region in this specimen. At the left end are its retinal branches (Reproduced from Hayreh et al. [8])
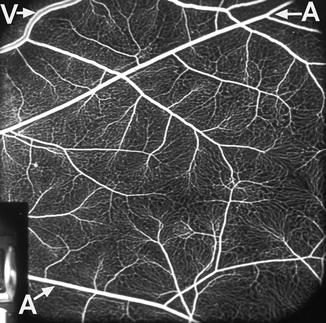
Fig. 7.3
Fluorescein fundus angiogram showing retinal vessels and capillary network. A retinal arteriole, V retinal vein
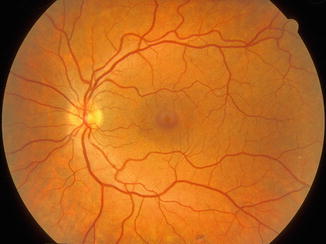
Fig. 7.4
Normal human fundus – left eye
Weinberg et al. [9] studied arteriovenous crossings within three disc diameters of the optic disc in photographs of 292 eyes (including 103 eyes with branch retinal vein occlusion, 90 fellow eyes, and 99 control eyes without branch retinal vein occlusion). The relative positions of the crossing artery and vein could be determined at 1,939 crossings in all eyes. A vein crossed over an artery in 22.3–33.0 % of crossings, but was rare at the crossings where branch retinal vein occlusions were found (2.4 %). An artery crossing over the vein was found in 77.7 % of the eyes with branch retinal vein occlusion, compared to fellow eyes (70.6 %) or control eyes (67.0 %). This indicates that the pattern of arteriovenous crossing may play a role in development of branch retinal vein occlusion. At the site of arteriovenous crossing, the artery and vein share a common fibrous coat and are separated by only a thin endothelial lining and basement membrane.
The superior branch veins usually join to form a superior trunk and the inferior branch veins an inferior trunk. These superior and inferior trunks usually join on the optic disc to form the central retinal vein (Fig. 7.1). The central retinal vein runs back in the center of the optic nerve, lying on the temporal side of the central retinal artery in the optic nerve, enclosed in a fibrous envelope (Fig. 7.5). During its intraneural course, the vein receives many tributaries (Fig. 7.1).
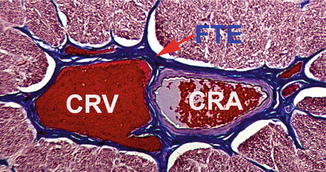
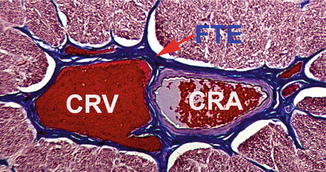
Fig. 7.5
A transverse section through the center of the intraorbital part of the optic nerve showing central retinal artery (CRA) and vein (CRV) lying side by side in close apposition, enclosed by a common fibrous tissue envelope (FTE) (Reproduced from Hayreh et al. [10])
During embryonic life, there are two venous trunks lying on either side of the central retinal artery (Fig. 7.6), which coalesce during the third trimester to form the single trunk of the central retinal vein [11, 12]; however, in 20 % of persons that congenital anomaly may persist during adult life [13]. In my anatomical studies, I found the two trunks of the central retinal vein in some adult eyes – the two lying on either side of the central retinal artery in the anterior part of the optic nerve (Fig. 7.7) [6]. Hughes [14] described two veins passing backward besides the central retinal artery in the nerve, one emerging out of the nerve proximal to the central retinal artery, the other leaving the nerve in the optic canal. Both pierce the sheath of the optic nerve to join the veins of the orbit. When a dual trunk of the central retinal vein is present during adult life, occlusion of one of the two trunks results in the development of hemicentral retinal vein occlusion [11]. Originally, the hyaloid artery is not accompanied by any vein [11]. The pial veins on the optic nerve lie in the pia mater and drain mainly into the central retinal vein at the site where the latter exits the optic nerve.
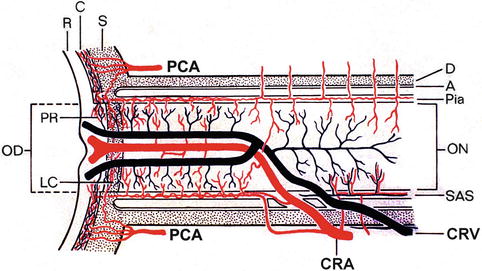
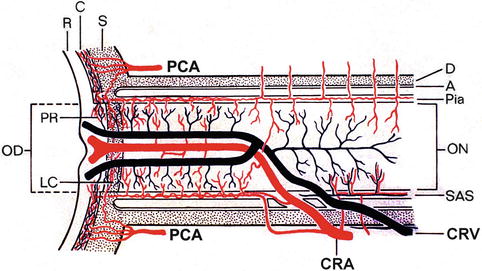
Fig. 7.6




Schematic representation of two trunks of the central retinal vein in the optic nerve (Reproduced from Hayreh et al. [12]). Abbreviations: A arachnoid, C choroid, CRA central retinal artery, Col. Br. collateral branches, CRV central retinal vein, D dura, LC lamina cribrosa, OD optic disc, ON optic nerve, PCA posterior ciliary artery, PR prelaminar region, R retina, S sclera, SAS subarachnoid space
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


