The Immunologic Components of Tears
Peter C. Donshik
William H. Ehlers
Virginia Calder
Tears comprise the fluid found in the precorneal tear film and the conjunctival fornices. The fluid volume of the tears is 5 to 10 mL.1 The lacrimal glands produce most of the tear fluid; the goblet cells and the accessory lacrimal glands of the conjunctiva have a secondary role in tear production.2,3,4 This complex fluid is composed of many different substances, such as proteins, enzymes, lipids, metabolites, and electrolytes.
The protein level in the tears of normal, healthy persons has been reported to vary between 3 and 20 g/L, depending on the secretion rate and methods of collection.3 Vascular permeability also plays a role, and it is known that these protein levels can double during inflammatory conditions. The following proteins have been isolated in the tear fluid: albumin, lysozyme, lactoferrin, transferrin, ceruloplasmin, IgA, IgG, IgM, IgE, complement, glycoprotein, and antiproteinases.4 In addition, interleukin cytokines including IL-1α, IL-1β, IL-8, and lipid mediators, such as leukotriene B4 and platelet activating factor (PAF) have been measured in normal tears.5 Certain components of the complement system often have been found in normal and diseased states. Histamine, tryptase, and plasmin are other important mediators that have been found in the tears of allergic persons.
Immunoglobulins
Tear immunoglobulins have been measured in normal and some diseased states. In the noninflamed eye, IgA, IgG, and IgE have been measured (Table 37.1).6 In the inflamed eye, these tear immunoglobulins are elevated and, on occasion, IgM is found to be present.
TABLE 37.1. The immunoglobulin level in normal tears. | ||||||||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| ||||||||||||||||||||
The IgA class of serum immunoglobulins was first described in 1959, and was soon shown to be the major immunoglobulin present in external secretions.7,8 Further studies by McClellan et al.9 and Donshik and Ballow10 have shown that IgA is the predominant immunoglobulin in the tear film, with an average value of 16.6 mg/dL (range, 7 to 85 mg/dL).
Tear IgA is an 11S immunoglobulin dimer with certain structural differences from serum IgA, which is a 7S immunoglobulin.11 The IgA consists of two heavy chains and two light chains, either of the k or l type, but not both. Tear IgA has a molecular weight of 380,000 daltons and is composed of two 7S IgA molecules held in the dimer configuration by the J chain. Upon secretion by the submucosal plasma cells, this IgA dimer binds to secretory component (SC) cells of the lacrimal gland. Bound SC facilitates the transport of the IgA dimer and protects it from proteolytic digestion in the tear secretions.12 The tear secretory IgA probably is produced also by the accessory lacrimal gland, the only other gland in which the SC component has been identified.
Sullivan and Allansmith provided further evidence that tear IgA is locally produced and does not originate in the serum.13 They were able to produce a sustained 20-fold increase in the serum IgA of rats, with no increase in the tear IgA. They also reported that incubation of the rats’ exorbital gland in vitro led to the accumulation of IgA. It had been shown that this gland, like the human lacrimal gland, has a high density of IgA-containing plasma cells and produces significant amounts of SC. It is also possible that, in addition to the local stimulation and production of IgA, a mechanism of remote stimulation results in the local production of tear immunoglobulins. For example, the oral administration of Streptococcus mutans (a nonocular bacterium) results in the formation of secretory IgA antibody in human tears and saliva. The tear IgA was not a transudate from the serum, but was locally produced.1 The IgA in tears is believed to protect the mucosal surfaces of the eye by acting as an immunologic barrier to the adherence, colonization, and cellular entry of microbial organisms and antigenic macromolecules.
IgG, the most abundant immunoglobulin in the serum, is present in only small amounts in normal tears.6,2 Donshik and Ballow10 found that an average of 1.0 mg/dL of IgG is present in the tears of normal persons. This immunoglobulin is composed of two heavy chains and two light chains. The four subclasses of IgG (IgG1, IgG2, IgG3, and IgG4) are classified on the basis of changes in the structure of the heavy chain. These subclasses have slightly different biologic, physical, and chemical properties. The exact function of IgG in tears is not known. In serum, it plays an important role in immune defense reactions against microbial organisms and toxins. Except for subclass IgG4, the IgG subclasses fix complement. IgG4 is thought to be important because it can act as a blocking antibody: When combined with allergens, it prevents the allergens from interacting with the IgE bound to mast cells.
IgM is found in smaller concentrations in the serum (60 to 200 mg/dL) and is undetected in normal tears.10,15 It has a sediment coefficient of 19S and a molecular weight of 900,000 d. It is composed of five 7S subunits. In serum, it is the most efficient immunoglobulin with regard to agglutinating particular antigens and fixing complement. It appears to be involved in the primary immune reaction, especially in combating bacterial infection. IgM forms the antibodies against polysaccharide antigens, and is the antibody to natural-forming blood groups and cold agglutinants.
IgE is present in the serum in small amounts and can be detected in minute amounts in the tears of normal subjects. McClellan and coworkers have reported a value of 200 ng/mL.9 Nomura and Takamura reported a value of 52.1 ± 9.7 ng/mL3, and Donshik and Ballow have reported a mean a value of 1.1 IU/mL.10 Serum IgE has a molecular weight of 200,000 d, and it does not fix complement. One of its important characteristics is its ability to sensitize cells, especially mast cells, resulting in degranulation of these cells and the release of their vasoactive amines. IgE antibodies are known as reagins. They play an important role in the atopic allergic patient.
Complement
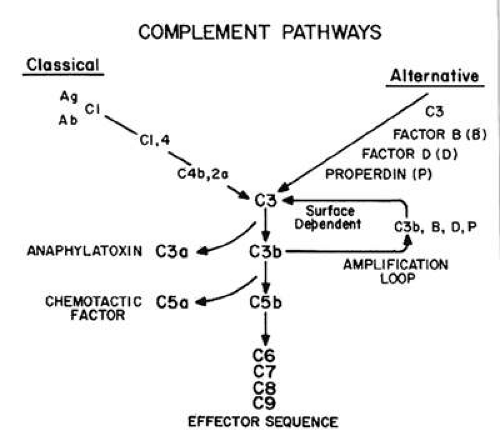
The complement (C) system is a complex network of proteins, enzymes, and inhibitors. The biologic activities of this network are important in both host defense and host reaction to inflammatory conditions (Fig. 37.1). The tears of normal persons have been shown to contain C3,9,15,4 hemolytic C4,5 hemolytic C,6 C5,7 and factor B.17,19 The complement system is present in the tears of normal persons, and may have an important role in protecting the external eye against infection, or participating in inflammatory reactions that could lead to ocular damage. In addition, decay-accelerating factor (DAF), a membrane-bound protein that helps regulate the amplification of the complement cascade, also has been found in normal tears (a mean concentration of 325 ± 289 ng/mL) and on the ocular surface. DAF retards the cascade through inhibition of central C3 amplification convertase. Another regulatory protein, CD59, is present in normal tears (mean concentration of 222 ± 28 ng/mL). This protein is active in inhibiting C5b-9, a complement component responsible for hemolytic activity.8
Tear Mediators in Ocular Allergy
Plasmin activity has been found in the tears of normal persons. Elevated levels have been found in patients with allergic conjunctivitis following topical exposure to specific allergens.9 Elevated levels also have been reported in contact lens wearers.10 However, Vannas and coworkers11 found elevated plasmin levels only in wearers of soft and rigid extended-wear contact lenses, not in wearers of daily-wear contact lenses. They also found elevated plasmin activity levels after both short-term (1-hour) and long-term (8-hour) eye closure, with or without contact lens wear. Thus, they believed that the increased tear plasmin in their study was a factor of eye closure, rather than contact lens wear.
Mast cells (MC), a heterogeneous group of cells, are the main effector cells in allergic disease. They contain formed and preformed mediators that are responsible for the pathologic course of allergic diseases. Mast cells contain neutroproteases, and two types of mast cells with different neutroprotease composition have been reported. The MCt cells contain tryptase, and the MCtc cells contain both tryptase and chymase. The former has been shown to be a marker for T lymphocyte–dependent mast cells, but the latter are not dependent on T lymphocytes for normal growth.12 Irani and coworkers13 showed that normal conjunctival epithelium is devoid of mast cells, whereas the substantia propria contains an average of 11,054/mm3. Of these cells, 95% were classified as MCtc; thus, the predominant mast cells in the conjunctiva are those containing both tryptase and chymase. In patients with vernal conjunctivitis (VC) and giant papillary conjunctivitis (GPC), mast cells were found in both the epithelium and the substantia propria. Patients with allergic conjunctivitis, however, were found to have mast cells in the substantia propria, but not in the epithelium. The MCt subtype was present in the substantia propria in patients with VC, but in patients with GPC and allergic conjunctivitis, the subtype was MCtc. Histamine, leukotriene C, and cytokines IL-4 and IL-13—cytokines known to drive TH2-like allergic responses—were found preferentially associated with the MCtc mast cells, whereas IL-5 and IL-6 were associated with the MCt cells. This would suggest that different mast cells may have different roles in the allergic reaction.14
In ocular allergy, one of the most widely studied mediators is histamine. Histamine is present in the granules of mast cells and basophiles. When mast cells are activated, histamine is released. It is present in the tears of normal individuals in very low concentrations.15 Elevated levels have been found, however, in patients with allergic conjunctivitis, and especially in patients with VC, in whom it can reach levels of 100 ng/mL.16,17 Histamine can cause capillary dilatation, increased vascular permeability, and smooth-muscle contraction, which clinically results in conjunctival redness, increased tearing, and ocular itching.
A range of other cytokines and chemokines have been found to be present in the tears of normal controls; these agents are elevated in allergic conjunctivitis and VC. Using enzyme-linked immunosorbent assay (ELISA), high levels of eotaxin-1 and eotaxin-2 were found in the mucus of VC patients, whereas only eotaxin-2 was found to have increased significantly in the tears of VC patients compared with those of normal patients.18 This mucus contained higher levels of chemokines than did tears. Both tear eotaxin-1 and eotaxin-2 were correlated significantly with the percent of eosinophils in tear fluid.
One of the technical difficulties in cytokine detection in tears has been the limited volume available—only one or two cytokines can be measured by ELISA. The advent of multiplex bead arrays for detecting mediators has allowed several cytokines and chemokines to be assayed from single tear samples. Using this highly sensitive technique, it was initially demonstrated that 6 cytokines (interferon-γ [IFNg], tumor necrosis factor-α [TNF-α], IL-2, -4, -5, -10) could be detected in all tears, but significantly less IL-10 was present in the tears from patients with allergic conjunctivitis.19 In another study of 14 mediators, it was found that IL-1b, IL-2, IL-5, IL-6, IL-12, IL-13, membrane cofactor protein-1 (MCP-1) were increased in all allergic conjunctivitis tears groups compared with controls.20 Moreover IL-4, IFNg, IL-10, and TNFa were increased in VC, with IL-5, regulated on activation, normal T expressed and secreted (RANTES), and eotaxin-1 levels significantly higher than in allergic conjunctivitis (P <0.05).
The source of the mediators present in tears remains unclear. Several candidate cells have been proposed, including the activated inflammatory cells such as eosinophils, mast cells and T cells, when present in the more chronic forms of conjunctivitis. In addition, conjunctival resident cells, such as epithelial cells and fibroblasts, are potential sources. By immunohistochemical staining, increased expression of IL-4, IL-5, and IL-6 was found to colocalize to mast cells in mucosal allergic inflammatory sites.21 Eosinophils also have been demonstrated to have the capacity to secrete a wide range of mediators, and various cytokines have been localized to conjunctival eosinophils including IL-3, -4, -5, -6, -8, with IL-5 being prominent in GPC.22 In a mouse model of allergic conjunctivitis, IL-4 immunization was an effective cytokine for inducing eosinophilia.23 Thus, in the conjunctiva, it is likely that mast cell–derived cytokines such as IL-4 can influence the eosinophil response. Furthermore, using in situ hybridization, the infiltrating T cells in tarsal biopsy specimens from patients with VC were found to stain positively for IL-2 and IL-4, whereas in atopic keratoconjunctivitis, a significant increase occurred in the T-cell expression of IFN-γ.24 In tear samples, it was demonstrated by intracellular cytokine staining that, in VC, a raised expression of IL-4 in T cells occurred, suggesting that these cells are a potential source of this cytokine.25 Recent unpublished data from our group have indicated that conjunctival fibroblasts produce IL-6, IL-8, MCP-1, and RANTES, all of which were up-regulated by TNF-a, whereas eotaxin was up-regulated by IL-4.26 These studies suggest that a complex network of cells and cytokines exist at the ocular surface. This network can be reflected in tear specimens and tends to be differentially up-regulated, depending on the severity of conjunctival inflammation.
Tear Immunoglobulins and Mediators in Disease States
In the closed eye state, total tear protein increases, with increases noted in secretory IgA, serum albumin, and C3 activation. However, the concentrations of lysozyme, lactoferrin, and tear-specific prealbumin remains unchanged. This suggests that, in the closed eye, a subclinical inflammatory condition exists.27
The role of tear immunoglobulins in disease states is poorly understood. Investigators have not been entirely in agreement as to whether the changes in the tear immunoglobulins are due to local production or to transudation from the blood plasma.
No question exists that tears are important in preventing and fighting external ocular infections. The presence of antimicrobial substances, such as lysozyme, lactoferrin, and β-lysin, is well accepted.28 Secretory IgA, the predominant immunoglobulin in tears, prevents bacterial adherence to mucosal surfaces and can neutralize viruses.29 Patients with IgA deficiency have an increased incidence of recurrent and chronic conjunctivitis.30 Sen and Sarin found elevated IgA levels in patients with acute bacterial conjunctivitis, blepharoconjunctivitis, and keratoconjunctivitis.31 In patients with VC, phlyctenular conjunctivitis, and corneal ulcers, the values were similar to those in control subjects. However, the authors did not state whether the increased immunoglobulin levels were due to local production or to leakage from the serum, secondary to the active inflammation.
During the first months of wear, rigid gas-permeable contact lenses can cause a decrease in the tear levels of secretory IgA, accompanied by elevated levels of lysozyme, which then return to normal levels. Individuals, however, can show marked decreases in tear secretory IgA even after 1 year of using these lenses. It has not been determined if these persons are at a higher risk for ocular complications secondary to contact lens wear.32 Tear IgG is significantly elevated in patients with acute adenoviral conjunctivitis, whereas the IgM in these patients was only slightly elevated and no significant change was noted in the tear IgA.33 It was interesting to note that, in these patients, the serum IgA level was unchanged; but instead of an increase, there was a decrease in serum IgG and IgM as compared with control patients. The abnormalities of the immunoglobulins in both tears and serum returned to normal levels as the disease process abated.
Tear immunoglobulin levels have been studied extensively in patients with VC. VC is a bilateral, recurrent, often severe inflammatory condition of the conjunctiva. It is characterized by itching, tearing, mucoid discharge, and photophobia. Papillary hypertrophy of the upper tarsal conjunctiva and the presence of eosinophils in the tear secretions are pathognomonic of this condition. IgE has been shown to be elevated in the tears of these patients.34 Samra and coworkers35 reported significantly elevated levels of IgE in the tears of patients with VC, and demonstrated that the IgE was locally produced by the external eye. Nomura and Takamura have reported IgE levels of approximately 322 ng/mL in these patients.16 Ballow and Mendelson reported that specific IgE antibodies are present in the tears of patients with VC and noted elevated IgG and IgM levels in the tears of these patients.36,37 They used transferrin as a marker for the transudation of plasma proteins into tear secretions and found that IgG and IgM, as well as IgE, were mostly locally produced by the external eye. Furthermore, they reported the presence of pollen-specific IgG antibodies to rye grass and ragweed antigen E in the tears of patients with VC. These specific tear IgG antibodies were not found in the tears of normal persons or in those with nonspecific conjunctivitis. As with the other tear immunoglobulins, these specific IgG antibodies were locally produced by the eye. Not all the patients with VC had elevated tear IgG and IgE levels: Apparent subsets of patients with VC exist, with regard to abnormalities in their tear immunoglobulins. Specifically, only 69% of patients who had elevated IgE had elevated specific IgG antibodies, whereas of those patients with VC who had undetectable levels of IgE, 82% had specific IgG antibodies. These results suggest that both IgE- and IgG-mediated immune mechanisms may be important in the pathogenesis of VC.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree