14

The Frontal Sinus:
The Endoscopic Approach
This chapter is dedicated to the treatment of frontal sinusitis. Although separate chapters in this book have been devoted to embryology, radiology, and anatomy, some brief discussion of these with specific reference to the frontal sinus seems obligatory. The frontal sinus remains the most difficult of the dependent sinuses for the endoscopic surgeon. It is the most difficult sinus to treat in a functional way by clearing the natural outflow tract without causing iatrogenic stenosis of the ostium, and it is the sinus that requires the greatest surgical expertise and level of intervention once ostium stenosis has occurred. Within this chapter, I will stress my own philosophy of treating the frontal sinus while attempting to avoid this most unwanted complication.
 Embryology
Embryology
Kasper1 described four frontal sinus pits or furrows. These are the ethmoidal pneumatization into the frontal bone, which will become the frontal sinus, and the out-flow tract structures. The first pit generally becomes the agger nasi cell, the second, the frontal sinus, and the third and fourth, the anterior or supraorbital ethmoid cells (if these are present). At about age 2 years the pneumatization enters the vertical portion of the frontal bone and progressively enlarges over the next 15 to 18 years.
 Anatomy
Anatomy
Understanding frontal sinus anatomy for an endoscopic surgeon requires a detailed understanding of the frontal recess. The term internal frontal ostium will be used for the bony orifice leading into the frontal sinus, and the term frontal recess will be used for that anatomy comprising the outflow tract of the frontal sinus, between the internal frontal ostium and the middle meatus. Most authors have tried to get away from the older term nasofrontal duct that suggested a more tubular bony structure that rarely exists.
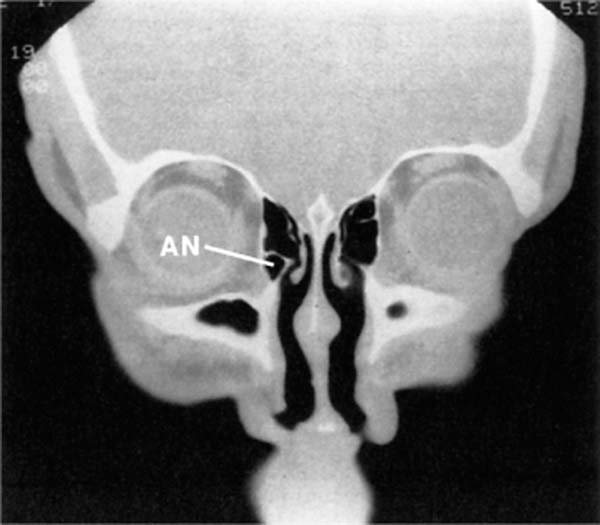
If one thinks of the level of the ostium as the central part of an hourglass, as suggested by Stammberger and Hawke,2 it is visually helpful. From the central portion down we find the frontal recess, most notable for the agger nasi. The agger nasi cell, a highly reliable landmark present in over 90% of patients (Fig. 14–1), is the key to the frontal recess. The agger nasi cell has as its boundaries laterally the lacrimal sac and orbit, medially the uncinate process, posteriorly the anterior ethmoid artery and skull base, and superiorly the frontal recess. The medial border of the frontal recess is almost always the lateral surface of the anterior portion of the middle turbinate. This, however, is dependent on the type of insertion that the uncinate process takes.
FIGURE 14–1 Coronal CT. The agger nasi (AN) is in front of the anterior attachment of the middle turbinate.
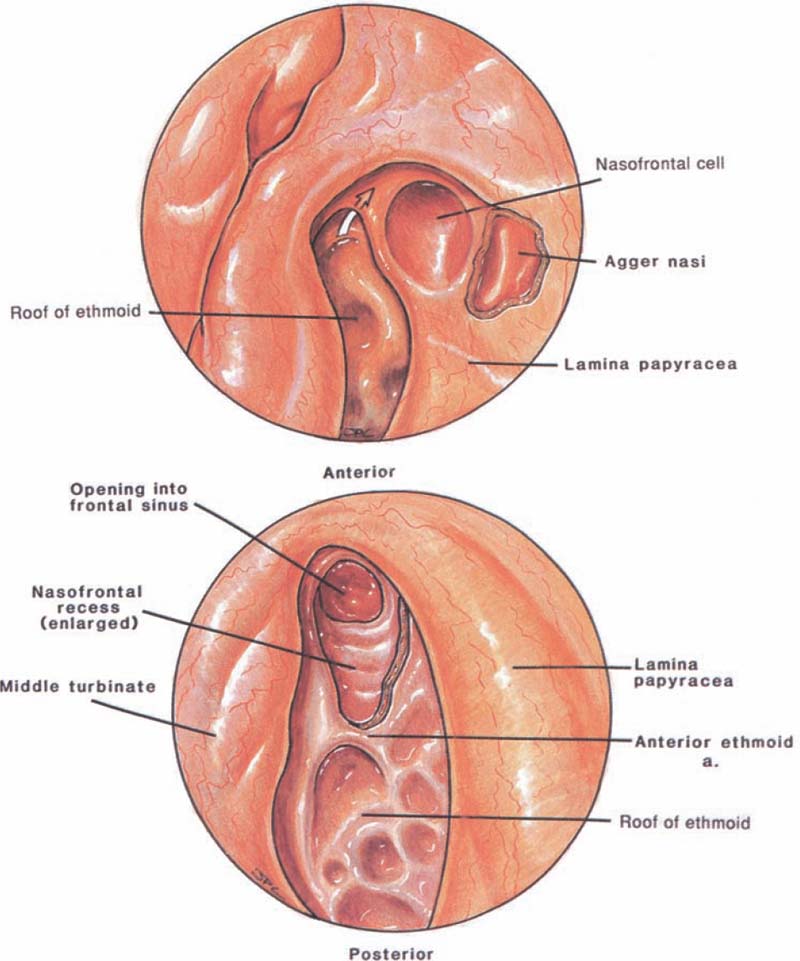
FIGURE 14–2 (A,B) Endoscopic views of the left nasofrontal recess after the agger nasi cell has been opened. In this case, the frontal sinus drains medial to the infundibulum.
In the vast majority of cases (85%) the uncinate process will merge with the medial wall of the agger nasi cell; therefore, the frontal sinus will drain between the uncinate process and the middle turbinate (Fig. 14–2), thus using the middle turbinate lateral surface as the medial border of the frontal recess.1 However, in a small number of cases the uncinate process will attach either to the insertion site of the middle turbinate along the lateral lamella of the cribriform plate or to the skull base. In this small number of cases (less than 15%) the frontal recess will have a direct entry into the infundibulum (Fig. 14–3).
The upper part of the hourglass then starts at the internal frontal ostium. The lateral aspect of the upper hourglass is the curved upper portion of the orbital roof. Anteriorly, the ostium is made up of a thick plate of bone that is the confluence of the nasal bone and the frontal bone. The primary frontal sinus ostium is located within the medial aspect of the frontal sinus floor close to the inner sinus septum. The size of this ostium has been variably reported but is felt to average 3 to 4 mm.
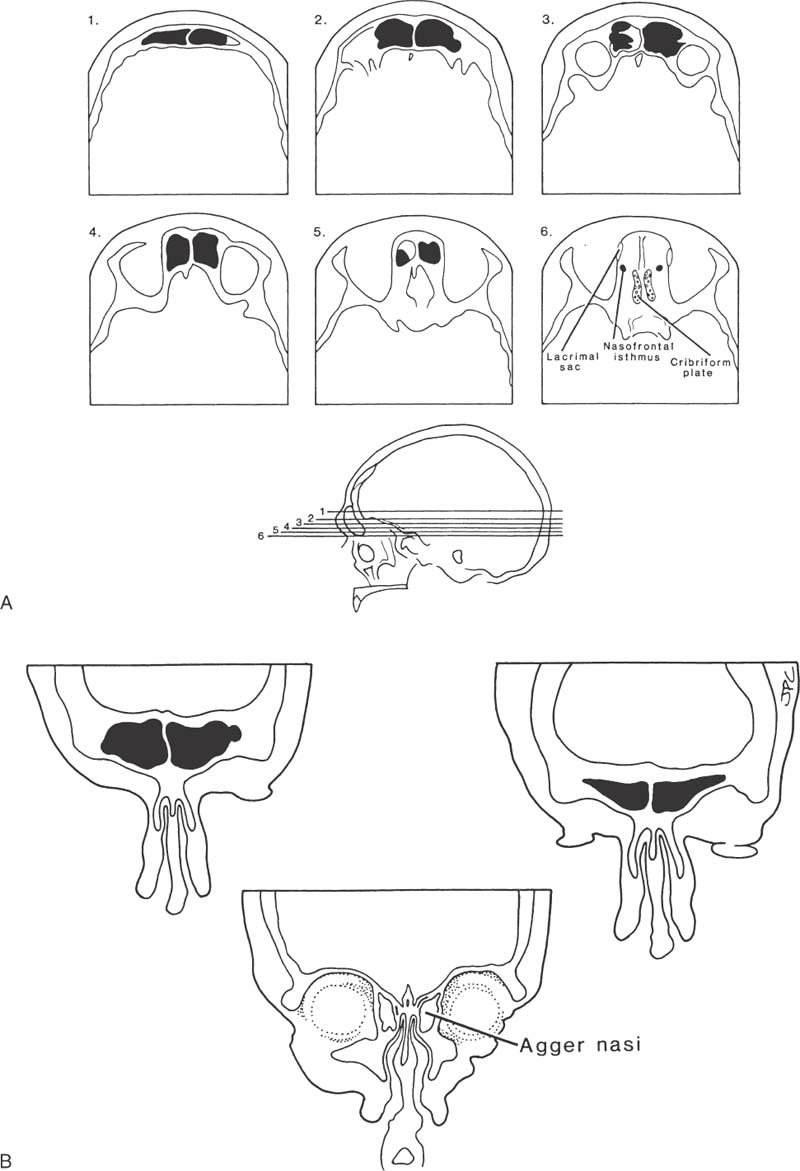
FIGURE 14–3 The uncinate attaches to the skull base. In this case, the frontal sinus drains into the infundibulum.
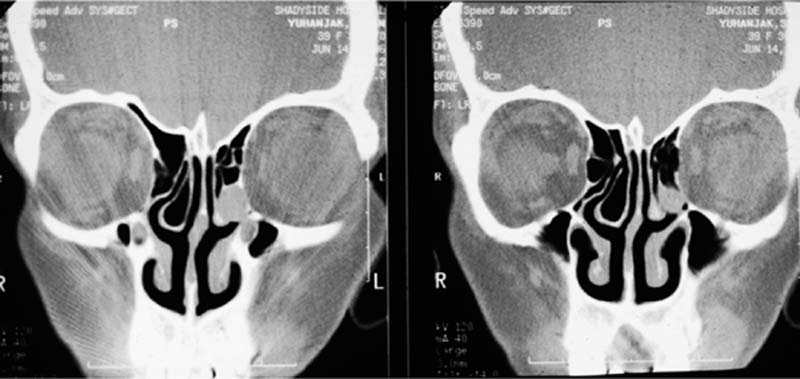
In most cases the frontal sinus consists of two large cells separated by an inner sinus septum. In 15% of patients there may be an absence of one of these cells, and in 5% of patients neither frontal sinus may become pneumatized (Fig. 14–4). The position of these cells in relation to the orbit and anterior cranial fossa is of paramount importance to the frontal sinus surgeon. Figure 14–5 shows the relationship of the frontal sinus to the anterior cranial fossa and orbit at six levels in the axial plane; the most inferior section shows how the frontal sinus narrows to the nasal frontal isthmus, which lies between the cribriform plate posteriorly and the lacrimal sac ante-riorly and laterally. Figure 14–5C is a three-dimensional representation of a right frontal sinus showing the frontal sinus in its relationship to the cribriform plate and anterior cranial fossa. Figure 14–5D shows the frontal sinus in a coronal plane in its relationship to the agger nasi cell and middle turbinate.
 Pathophysiology
Pathophysiology
Like other paranasal sinuses discussed heretofore the frontal sinus relies on the mucociliary clearance. Any procedure done on the frontal sinus must respect this mucociliary clearance if it is to be successful. Any disease process that affects the ability of secretions to enter into the ethmoid from the frontal sinus will cause pathology in this location. Most commonly edema, polyps, and a variety of benign neoplasms are encountered. However, of a more worrisome nature is the increasing frequency with which scarring and adhesions in the nasofrontal region due to iatrogenic trauma are becoming the main indication for surgery. It is the combination of obstruction and infection that causes symptoms for the patient with frontal sinusitis and is the establishment of free drainage into the nose that relieves this condition. The surgeon must understand the pathophysiology of the individual patient’s problem with a keen eye toward the anatomical abnormalities, a firm understanding of the particular pathophysiology at work in the patient, and a highly developed level of surgical expertise. The reader should review the original papers by Kasper,1 Schaffer,3 and Van Alyea,4 as well as the more recent work by Kuhn et al5 to master this anatomical region.
FIGURE 14–4 Unilateral frontal sinus.
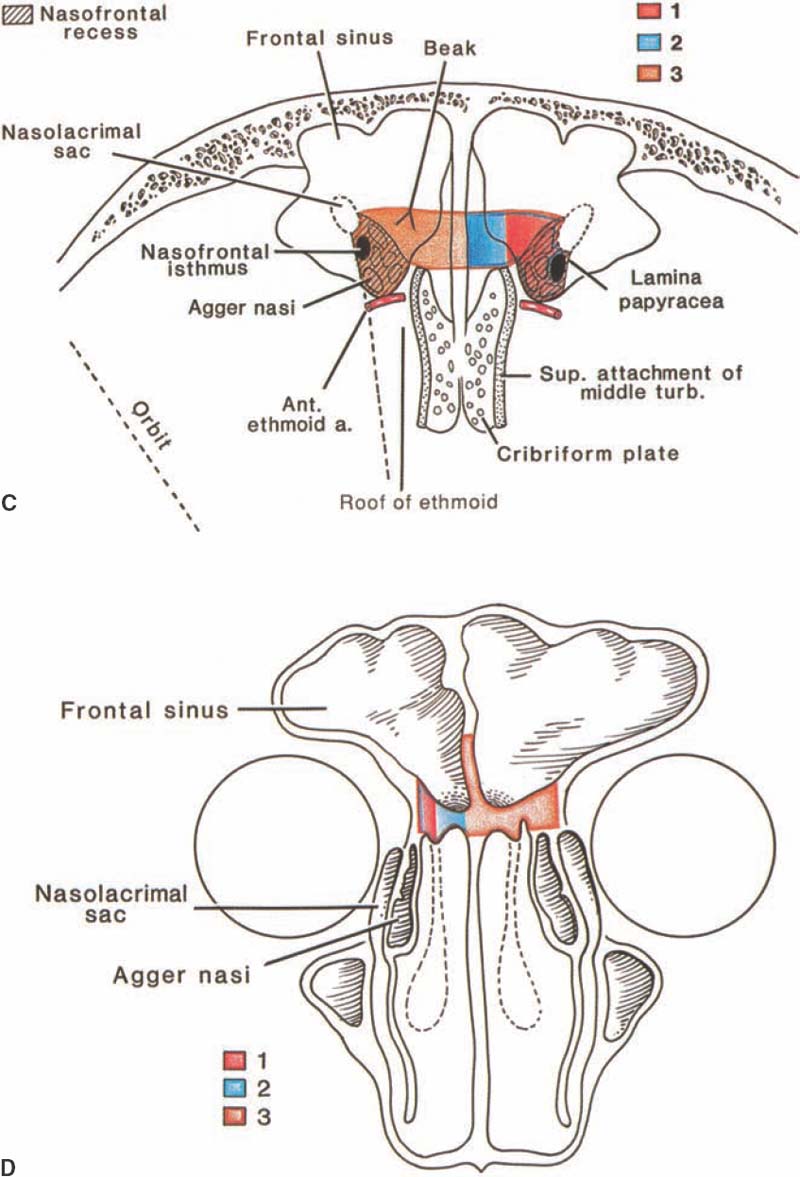
FIGURE 14–5 Survey CT of the frontal sinus used to determine dimensions of the sinus and anatomical relationships to nasofrontal recess. (A) Axial CT, cuts 1 through 6. Frontal sinus narrows to a small isthmus as it drains into the nasofrontal recess. (B) Coronal CT scan shows the relationship of the frontal sinus to the orbit and agger nasi cells (C,D) Demonstration of these relationships and the nasofrontal drillout approach to enlarge the frontal sinus outflow tract.
Adding to the frontal sinus surgeon’s difficulty is the healing burden of chronic inflamed tissue, the potential bone loss from the disease process or previous surgery, and the presence of scar from the previous surgeon’s procedure. The following philosophy is drawn out of my own expertise in treating over 2000 patients surgically for sinusitis with an eye toward preventing iatrogenic frontal sinus problems (Table 14–1).
Surgical Treatment
The endoscopic approach has revolutionized the thinking in regard to diseases of the paranasal sinuses. The work of Messerklinger6 and Stammberger and Hawke2 and all of their disciples has strengthened the belief in the reestablishment of mucociliary clearance as the “gold standard.” To this end, I offer the following treatment philosophy based on individual patient presentation to maximize surgical success and minimize iatrogenic trauma (Tables 14–2 and 14–3).
1. Symptomatic patient 2. Nasal polyps 3. Asthma 4. Aspirin sensitivity 5. Extensive disease 6. Previous surgery 7. Underlying problems—allergy immunodeficiency: • Cystic fibrosis • Cilial dysfunction 8. Anatomy problems—septum • Concha bullosa • Others 9. Wrong diagnosis 10. Inadequate surgery 11. Inappropriate surgery 12. Poor technique 13. Synechia 14. Complications 15. Insufficient/inadequate postoperative surgical therapy 16. Inadequate postoperative medical therapy |
1. Maxillary sinus ostia Stay updated, free articles. Join our Telegram channel
Full access? Get Clinical Tree
 Get Clinical Tree app for offline access
Get Clinical Tree app for offline access

|