The Facial Nerve
Steven L. Galetta
Mark May
The facial nerve, by virtue of its unique neuroanatomy and physiology and its complex course across the skull base and face, is often involved in neuro-ophthalmologic problems. Abnormalities of lid position and defective tearing are regularly symptomatic, demanding ophthalmologic attention. This chapter provides both an anatomic and an etiologic approach to the spectrum of facial nerve disorders. The current management of facial nerve paresis and facial hyperkinetic syndromes is emphasized.
EMBRYOLOGY
Normal and abnormal functions of the facial nerve can be best understood through an awareness of its embryonic development. The complexity of the nerve’s course, its branching patterns, and its anatomic relationships are established during the first 3 months of prenatal life.1 During this period, the muscles of facial expression also differentiate, become functional, and actively contract.2 Critical phases in facial nerve development occur throughout gestation, and the nerve is not fully developed until about 4 months after birth (Table 1).
TABLE 1. Time During Gestation When Anatomic Structures Appear | ||||||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
|
INTRAMEDULLARY SEGMENT
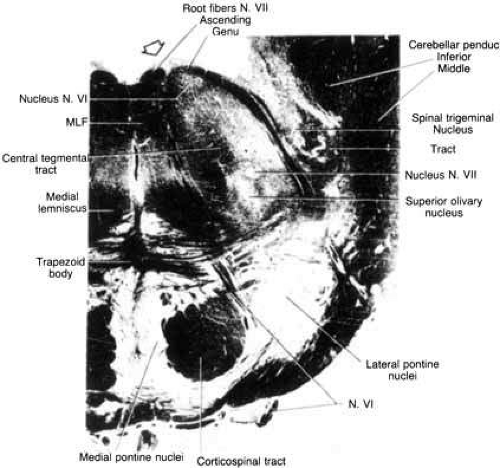
The motor nuclei of the sixth and seventh cranial nerves are initially in close proximity in the pontine subdivision of the metencephalon. As the metencephalon elongates and expands, the facial nucleus migrates ventrolaterally in relation to the abducens nucleus, displacing facial motor axons that loop dorsally in the floor of the fourth ventricle to form the facial colliculus (Fig. 1). This intimate relationship between the abducens and facial motor nuclei is the anatomic substrate for the clinical findings in congenital Möbius’ syndrome and in acquired inflammatory, vascular, and neoplastic lesions that involve the intramedullary segment of the facial nerve.
EXTRAMEDULLARY SEGMENT
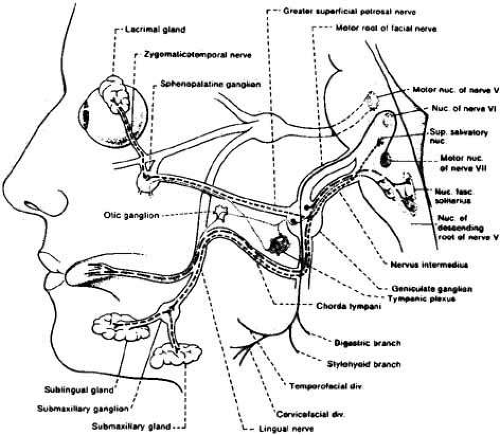
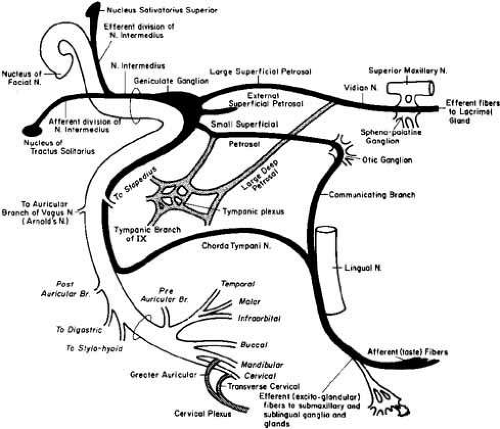
The facial nerve rootlets become distinguishable near the end of the seventh week of gestation, when the geniculate ganglion becomes well defined.1 The nervus intermedius, which contains afferent and general visceral efferent fibers, exits the brain stem between the facial motor root and the vestibular nerve. The afferent fibers arise from the geniculate ganglion, whereas the preganglionic parasympathetic fibers originate in the superior salivatory nucleus in the brain stem (Fig. 2). The fact that the geniculate ganglion and the parasympathetic fibers form independent of the motor pathways allows patients with congenital facial paralysis to enjoy intact tearing and taste, but with selective impairment of the motor neurons innervating the facial muscles.
INTRATEMPORAL SEGMENT
Small but important ganglia are scattered along the course of the facial nerve through the temporal bone.3 These ganglia are likely composed of aberrant sensory neurons from the tympanic plexus that enter the facial nerve near the stapedial branch. Because most viruses have an affinity for afferent nerve fibers, such sensory fibers may play an important role in the development of viral-immune facial nerve palsies.
Of all the cranial nerves, the facial nerve has the largest number of communications with other nerves.4 This situation may account for the variety of neurologic signs sometimes seen with herpes zoster cephalicus. The cutaneous branches of the second and third cervical ganglia (part of the cervical plexus of spinal nerves) are the initial nerves that establish connections with the facial nerve at its emergence from the stylomastoid foramen. In the facial palsy of herpes zoster cephalicus, these communications predict the distribution of the cutaneous eruption that involves the angle of the jaw, the back of, the head, and the neck, thus following the pattern of the C2–C3 dermatome (see later).
ANOMALIES
The facial nerve develops within the second branchial arch during the same period that closely adjacent derivatives of the first arch, the first internal pouch and external groove, are forming the external and middle ear regions. Therefore, anomalies of the facial nerve within the temporal bone should be anticipated whenever there are associated malformations of the external or middle ear. In these cases, displacement of the facial nerve and complete absence of the bony facial canal are the most common anomalies observed. Typically, the facial nerve can be seen sagging inferiorly against the stapes bone.5
ANATOMY
Familiarity with the general anatomy of the neural pathways for facial function is essential for accurate diagnosis and appropriate management of the spectrum of facial neuropathies. Specific diagnostic possibilities can be implied by precise regional localization of typical lesions (Table 2).
TABLE 2. Topical Diagnoses of Lesions of the Facial Nerve at Various Levels | ||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| ||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
CORTEX AND SUPRANUCLEAR PATHWAY
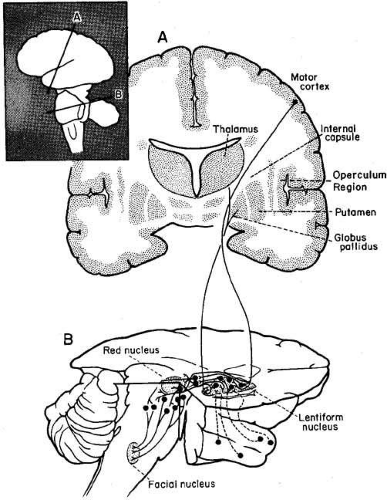
The voluntary responses of facial muscles, such as smiling or grimacing on command, are dependent on discharges from the facial motor area situated in the precentral gyrus of the frontal cerebral cortex. The facial motor areas are represented with the forehead uppermost and the eyelids, midface, nose, and lips located sequentially below (Fig. 3). Supranuclear motor neurons from the cortical face area are carried as fascicles of the corticobulbar tract to the genu of the internal capsule, then via the cerebral peduncles to the lower pons or upper medulla. The portion of the facial nucleus that supplies the muscles of the upper face (frontalis, orbicularis oculi, and corrugator muscles) receives corticobulbar fibers from both right and left precentral motor cortices, but the supranuclear tracts innervating the lower face are crossed only. For this reason, the muscles that raise and wrinkle the forehead and close both eyes are bilaterally innervated. Thus, a unilateral lesion in the cortex or supranuclear pathways spares eyelid closure and forehead movement but results in paralysis of the contralateral lower face. This dissociation is characteristic of supranuclear lesions. Because the supranuclear pathways may descend to the ventromedial medulla before decussating to innervate the facial nucleus, low brainstem lesions may produce contralateral lower facial weakness.6 However, it is also possible to show upper facial sparing with lesions of the pontine facial nucleus, with selective defects within the temporal bone, or even with an injury to nerve rootlets within the parotid gland or facial musculature. This phenomenon is related to the general tendency for facial nerve function to be spatially dispersed, not only in its cortical distribution but also within the pontine nucleus and in the peripheral nerve.
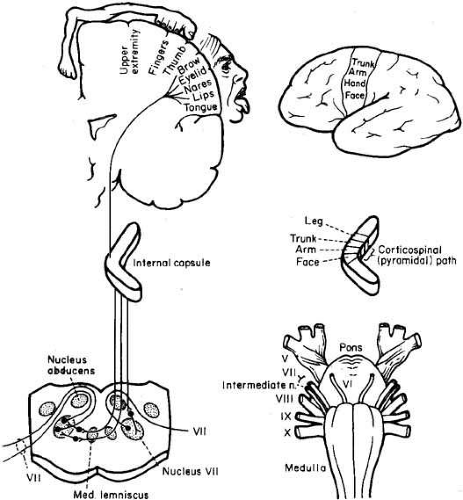 Fig. 3 Organization of facial motor function. Note cortical distribution, pontine nuclear connections, and relationships to other cranial nerves on ventral view of brain stem. |
Because preservation of forehead function is insufficient evidence of a cortical lesion, other neurologic signs should be sought. A cortical lesion that produces a contralateral lower facial palsy is usually associated with a motor deficit of the tongue and with weakness of the thumb, fingers, and hand on the same side as the hemifacial weakness, with lesser involvement of the leg. The cortical motor areas of the face, tongue, thumb, fingers, hand, and upper extremities lie near each other in the precentral territory nourished by the rolandic branch of the middle cerebral artery. Patients with such cortical lesions are unable to voluntarily smile, but facial expression is appropriate in response to an amusing story. Similar clinical findings may occur with lesions that involve the descending corticobulbar and corticospinal tracts.7
Although facial muscle tone is not significantly impaired with a supranuclear lesion, slight flattening of the nasolabial fold and drooping in the corner of the mouth may be detected contralateral to the cortical lesion.
EXTRAPYRAMIDAL SYSTEM
The extrapyramidal system (Fig. 4) consists of the basal ganglia and the descending motor projections other than the fibers of the corticospinal (pyramidal) tract. Anatomically, this system appears to be a diffuse, multisynaptic network that interconnects extensively with centrencephalic and brain stem structures. These pathways are not as well clarified as those of the primary (pyramidal) motor tracts. The extrapyramidal system is concerned with automatic and emotional facial language. The dull, expressionless face of parkinsonism is a well-known result of extrapyramidal pathway disease, whereas the spontaneous facial dystonia of Meige’s syndrome is characterized by unilateral or, more often, bilateral blepharospasm associated with dystonic movements of the mouth and other lower facial muscles. Progression of this latter disorder may lead to chaotic contractions of the tongue and cervical muscles.
PONS
The facial motor nucleus contains about 7,000 motor nuclei 8 and is located in the ventrolateral angle of the lower pontine tegmentum (see Fig. 1). The facial nucleus can be divided into four separate cell groups that supply specific muscle groups: (1) dorsomedial (auricular and occipital muscles), (2) intermediate (frontalis, corrugator, and orbicularis oculi muscles), (3) ventromedial (platysma), and (4) lateral (buccinator and buccolabial).9 The motor axons exit the nucleus dorsally, loop around the abducens (VI) nucleus, and form the facial genu before emerging from the lateral aspect of the pons. The superior salivatory nucleus, which is located just rostral to the facial motor nucleus, is the origin of the parasympathetic fibers that supply the sublingual, submandibular, and lacrimal glands. These salivary and lacrimal fibers join the facial nerve as the nervus intermedius in the cerebellopontine angle.
Because the facial nucleus is located ventromedial to the cochlear nuclei and the spinal tract and nucleus of the trigeminal nerve, a lesion of the lateral pons may result in ipsilateral facial paresis, ipsilateral facial analgesia, ipsilateral Horner’s syndrome, and ipsilateral deafness (Foville’s syndrome). If the lesion extends further dorsally, an ipsilateral gaze paresis would result from involvement of the sixth nerve nucleus. The combination of a unilateral sixth nerve palsy, an ipsilateral seventh nerve palsy, and a contralateral hemiparesis is known as the Millard–Gubler syndrome. Intrinsic lesions of the brain stem are usually the result of infarction, hemorrhage, tumor, or demyelination.
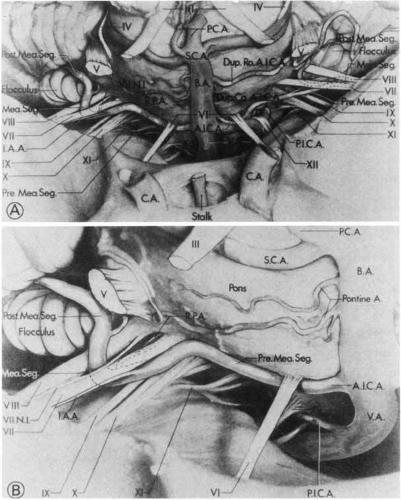
CEREBELLOPONTINE ANGLE
The facial nerve, the nervus intermedius, and the eighth (vestibuloacoustic) cranial nerve exit together from the ventrolateral aspect of the pons, surrounded by a leptomeningeal covering. In the lateral pontine cistern, the anteroinferior cerebellar artery may loop between the seventh and eighth cranial nerves as the artery courses posteriorly to supply the dorsolateral pons and cerebellum.10 As the nervus intermedius approaches the internal auditory meatus, it joins the facial nerve. Because of the association of the facial nerve with the nervus intermedius and the vestibuloacoustic nerves at the level of the cerebellopontine angle and in the internal auditory canal, tearing, taste, submandibular saliva flow, hearing, and balance are disturbed with mass lesions at this level (Fig. 5).
From the brain stem to the internal auditory canal, the facial nerve is covered only by a thin layer of glia, which makes it quite vulnerable to any type of surgical manipulation but quite resistant to a slow process of stretching or compression, as might occur with an acoustic schwannoma. Large tumors that fill the cerebellopontine angle compress neighboring cranial nerves and cause defects of the 5th and, later, the 9th, 10th, and 11th cranial nerves. Lesions that occur in this area include temporal bone fractures, acoustic neuromas (schwannomas), meningiomas, and primary cholesteatomas. Hyperkinetic disorders are attributed to vascular compression of the root of the facial nerve.
TEMPORAL BONE
The motor portion of the facial nerve and the nervus intermedius are loosely joined together as they enter the internal auditory meatus with the acoustic nerve. In this region, the facial nerve and nervus intermedius course superiorly to the vestibuloacoustic nerve. As the facial nerve emerges from the internal auditory meatus, it departs from the vestibuloacoustic nerve to enter the fallopian (facial) canal.
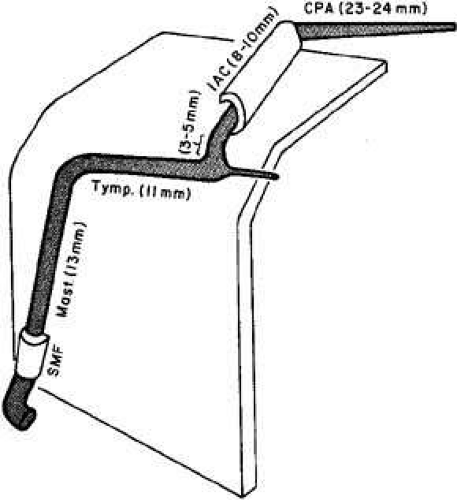
The course of the facial nerve through the fallopian (facial) canal is unique; no other nerve traverses so long a distance through a canal (28 to 30 mm). The nerve follows a remarkable Z-shaped course in its intratemporal portion (Fig. 6).11 Furthermore, it incorporates a sensory ganglion, the geniculate. In the fallopian canal, the nerve trunk can be divided into labyrinthine, tympanic, and mastoid segments. The labyrinthine segment includes the geniculate ganglion, and it is at this level that the first branch of the facial nerve arises, the greater superficial petrosal nerve. This nerve traverses the dura of the floor of the middle cranial fossa, synapsing in the sphenopalatine ganglion; postganglionic secretory nerve fibers travel with the zygomaticotemporal nerve of the fifth nerve (V-2) and eventually join the lacrimal nerve of V-1 to innervate the lacrimal gland. Involvement of the greater superficial nerve in the middle fossa (e.g., from neoplastic invasion, inflammatory processes, and trauma) impairs reflex tear secretion. When defective tearing accompanies abducens or trigeminal nerve palsy, a lesion in the middle cranial fossa is indicated. Although lacrimal fibers are classically carried by the nervus intermedius, parasympathetic neurons variably reach their destination by way of branches of the fifth or ninth cranial nerves, because there are ample opportunities for intermingling among these nerves (Fig. 7).
At the geniculate ganglion, the facial nerve makes a sharply angled turn posteriorly, forming a knee (genu) to enter the tympanic, or horizontal, portion of the fallopian canal. The distal tympanic segment emerges from the middle ear between the posterior wall of the auditory canal and the horizontal semicircular canal, just beneath the short process of the incus. At this point, the fallopian aqueduct makes another turn downward, forming the second genu. This marks the beginning of the mastoid segment. The nerve continues vertically downward on the anterior wall of the mastoid process to the stylomastoid foramen. The chorda tympani is the terminal branch of the nervus intermedius and usually arises from the distal third of the mastoid segment of the facial nerve. The chorda tympani nerve contains secretory motor fibers to the submaxillary and sublingual salivary glands. It also carries special sensory afferents from the anterior two-thirds of the tongue (taste) and somatic sensory fibers from the posterior wall of the external auditory meatus (pain and temperature). The afferent fibers for taste synapse in the rostral nucleus solitarius of the medulla, whereas those somatic sensory fibers from the periauricular region terminate in the nucleus of the spinal tract of the fifth nerve.
EXTRACRANIAL SEGMENT
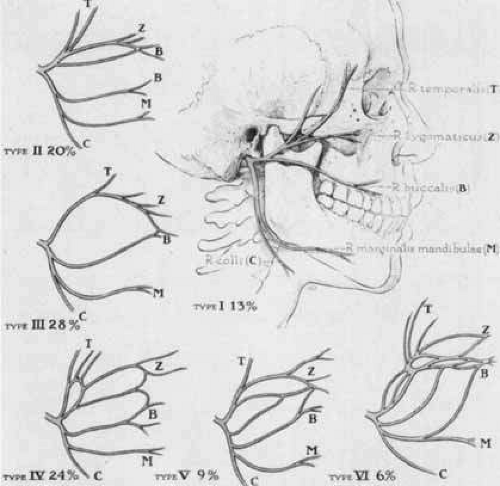
As the nerve exits the stylomastoid foramen behind the mandibular angle, and before it bifurcates, motor branches are given off to the posterior belly of the digastric, stylohyoid, and posterior auricular muscles. The main trunk of the facial nerve enters the substance of the parotid gland and then bifurcates into an upper and lower division (Fig. 8). These divisions can be further subdivided into the temporal, zygomatic, buccal, mandibular, and cervical branches. After emerging from the parotid gland, the facial nerve passes over the fascia of the masseter muscle. Although the course in this region is variable, there are some relationships that are relatively constant. There are communications between the upper and lower divisions that form a variety of patterns.12 This rich plexus of nerve filaments in the peripheral zone, just before entering the undersurface of the facial muscles, permits extensive intermingling between peripheral branches of the upper and lower divisions. These anastomoses provide the substrate for misdirected peripheral regeneration that may follow a facial nerve palsy. Such inappropriate axonal sprouting accounts for spontaneous lower facial movement upon blinking or an eye closure provoked by smiling (facial synkinesis). Considering the number of possible routes available to each interrupted neuron, it is truly remarkable that any patients are able to voluntarily control appropriate individual muscle movement. Similarly, “crocodile tears” (see later discussion) are the result of faulty regeneration of parasympathetic fibers that mistakenly innervate the lacrimal gland instead of the salivary glands. Thus, increased ipsilateral lacrimation associated with eating may occur after a denervating lesion of the facial nerve appears at or above the site of the geniculate ganglion or along the course of the greater superficial petrosal nerve.
BLOOD SUPPLY
The cortical motor area of the face is nourished by the rolandic branch of the middle cerebral artery. Within the pons, the facial nucleus and its motor axons receive their blood supply primarily from a combination of the anteroinferior cerebellar artery and the short and long circumferential arteries.
The extramedullary blood supply to the facial nerve as described by Nager and Nager13 is derived from three sources: the anteroinferior cerebellar artery, which enters the internal auditory meatus in close association with the seventh and eighth cranial nerves; the petrosal branch of the middle meningeal artery, which accompanies the greater petrosal nerve; and the stylomastoid branch of the posterior auricular artery, which enters the facial canal at the stylomastoid foramen. The territories supplied by the three arteries tend to overlap at any given level. Despite the richness of the blood supply to most segments of the facial nerve, vascular compromise is likely a factor in the pathogenesis of facial palsies. The area proximal to the geniculate ganglion is especially vulnerable to ischemic compression, not only because this is the narrowest part of the fallopian canal but also because there are no anastomoses between the arterial systems immediately proximal to the geniculate ganglion.14,15
FACIAL NERVE FUNCTION AND ASSESSMENT
MOTOR EVALUATION
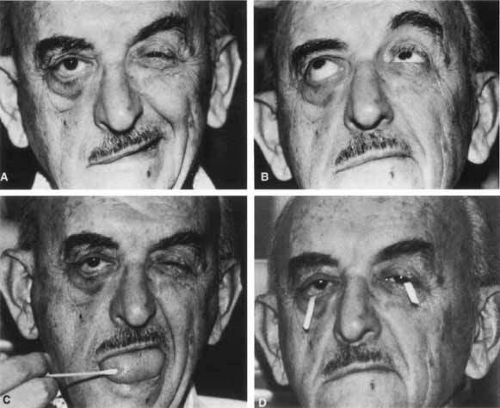
Assessment of facial nerve motor function begins by observing the patient at rest and noting any asymmetries of the face or of blink pattern. Most supranuclear and infranuclear facial nerve palsies are associated with a flattened nasolabial fold and a slightly widened palpebral fissure on the paretic side. Facial movement in response to emotional stimuli and voluntary command should also be assessed. A dissociation in response of spontaneous and voluntary movements is suggestive of supranuclear defects. Disease of the corticobulbar tracts tends to spare emotional facial responses, whereas disease of the basal ganglia preserves voluntary movements. Preservation of forehead wrinkling, seen best in attempted upward gaze, is also characteristic of supranuclear lesions (Fig. 9). Forced eyelid closure should be performed, and asymmetries in eyelash burying or lagophthalmos (i.e., partial or total inability to close the lids) should be noted.
TASTE
Taste receptors are distributed over the tongue and pharynx. Axons with cell bodies in the geniculate ganglion receive stimuli from receptors and project postganglionic afferents back to the nucleus tractus solitarius in the medulla. The seventh nerve carries taste fibers from the anterior two-thirds of the tongue; taste from the posterior third of the tongue is supplied by the ninth nerve. Taste is best tested with a cotton swab dipped in a sour, sweet, or bitter solution (see Fig. 9). Unilateral ageusia (loss of taste) may be useful in identifying a facial lesion as peripheral, but it should be noted that bedside tests of taste are crude and often unreliable.
TEAR FUNCTION
Evaluation of tear function by observation alone, without actual testing, may lead to erroneous impressions (e.g., that a patient with a facial palsy is tearing excessively).
Testing for tearing is of limited diagnostic and prognostic value, unless tear production is drastically reduced or absent on the involved side. In addition, the results of actual tear testing may be similarly misleading. Increased tear flow (epiphora) noted by history can be due to exposure irritation, paralytic ectropion, or failure of the lacrimal pump apparatus of the lower lid; it is not likely to be related to an irritative lesion of the greater superficial petrosal nerve. Similarly, decreased tearing, rather than suggesting a destructive process involving, for example, the greater superficial petrosal nerve, may be due to corneal hypesthesia.
Tear testing usually involves Schirmer paper strips placed in the inferior conjunctival cul-de-sacs. To avoid erroneous results from pooled tears, the conjunctival tear lake is dried before insertion of the paper strips (see Fig. 9). A Schirmer strip is inserted into the conjunctival sac of the uninvolved eye, and moments later a strip is placed in the involved eye. By following this sequence, the reflex blepharospasm and tearing provoked by stimulating the normal eye do not influence results in the contralateral eye.
About 10% of patients with Bell’s palsy have decreased or absent corneal sensation, usually from exposure hypesthesia or as a form of adaptation.16 In such cases, a topical anesthetic is instilled into both eyes before the Schirmer strips are placed, to eliminate the problem of selectively stimulating the eye with normal corneal sensation. The length of moistened paper is compared on the two sides after a period of 5 minutes. In the event that one of the filter strips becomes completely moistened before 5 minutes, both strips are removed and compared for results. Less than 5 mm of wetting is highly suggestive of a tear deficiency, but this finding should be viewed in the context of the patient’s clinical history and the results of the slit lamp examination.
BLINK REFLEX
Stimulation of either cornea with a cotton wisp or tissue corner will cause a bilateral blink. The ophthalmic division of the fifth nerve (V-1) is the afferent limb of the blink reflex, with first-order neurons synapsing primarily in the chief sensory nucleus within the pontine tegmentum. Second-order neurons project from the chief sensory nucleus to both facial nerve nuclei. Thus, if the left ophthalmic division is defective, neither eye will blink to left corneal stimulation. If the right cornea is stimulated in this setting, both eyes will blink. This scenario must be contrasted with the case of a left facial nerve palsy in which only the right eye will blink fully, regardless of which cornea is stimulated.
PHYSIOLOGIC FACIAL SYNKINESIS
Classically, Bell’s phenomenon results in the upward and outward deviation of each eye during lid closure against resistance. This palpebral–oculogyric reflex is particularly obvious in patients with lower motor neuron facial paresis and lagophthalmos (i.e., incomplete eye closure). Although the precise neural pathway is unknown, connections between the seventh- and third-nerve nuclei are implicated by this phenomenon. Francis and Loughhead19 have found a wide variability in the character of Bell’s phenomenon in normal subjects. In their series, many patients showed responses that did not conform to the typical “up and out” eye movement pattern. In addition, on repeated testing, subjects showed variable responses. Clinically, Bell’s phenomenon is most useful in distinguishing infranuclear and supranuclear ocular palsies. Typically, upward deviation of the eyes with forced eyelid closure is preserved in supranuclear lesions.
In some normal persons, the external ear retracts and flattens against the mastoid with conjugate lateral gaze. This is known as the oculogyric auricular reflex and is usually greater in the ear opposite the direction of lateral gaze. The presumed neural mechanism involves proprioceptive input from the extraocular muscles to the facial nuclear complex.
In the nasolacrimal reflex, the secretion of tears may be induced by chemically stimulating the nasal mucosa by sniffing dilute solutions of ammonia or formaldehyde. The neural pathway for this reflex results from connections of the trigeminal nerve (V1) to the greater superficial petrosal nerve. There are numerous other facial reflexes, including blinking during the sudden introduction of a bright light or loud noise, but a full description of these phenomena is beyond the scope of this text.
IDIOPATHIC (BELL’S) FACIAL PALSY
Peripheral facial paralysis is a diagnostic challenge. Every effort must be made to uncover the cause, because often a treatable lesion can be found. The causes of facial paralysis diagnosed and managed over a 24-year period are listed in Table 3. Of 2,406 patients seen during this time, no specific cause for the paralysis could be found in 53%. Although it is tempting to label all acute facial palsies as “idiopathic” (i.e., Bell’s palsy), 10% of the patients referred with a diagnosis of Bell’s palsy were found to have a treatable, progressive, or life-threatening lesion. It must be emphasized that Bell’s palsy is a diagnosis of exclusion, reserved for cases in which all other causes of acute acquired, isolated peripheral facial paralysis have been considered and investigated if necessary.
TABLE 3. Causes of Facial Nerve Disorders in 2406 Patients Seen Over 24 Years by One Clinician | ||||||||||||||||||||||||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| ||||||||||||||||||||||||||||||||||||
Although Bell’s palsy is a term reserved to designate an acute peripheral facial palsy of unknown cause, accumulating evidence supports a viral inflammatory–immune mechanism. In about 60% of cases, Bell’s palsy is associated with a viral prodrome. The disorder is self-limiting, is nonprogressive, is not life threatening, and spontaneously recovers; at this time it can be neither prevented nor cured. Incidence varies between 15% and 40% per 100,000 population annually.20,21,22,23
Subjective complaints include pain around the ear (50%), facial numbness (40%), changes in taste (50%), and numbness of the tongue (20%).16 A family history of facial palsies is noted in 14% of patients, and the syndrome is recurrent in 12%. Of those with a history of recurrence, the same side is involved in 36%. Disturbances of the stapes reflex (dysacusis; failure to dampen the vibrating ear ossicles, as determined by middle ear function studies), loss of taste of the anterior two-thirds of the tongue, and decreased sublingual and submandibular salivary secretion are most suggestive of a lesion in the tympanomastoid portion of the facial nerve.16
The onset of facial palsy is not in itself diagnostic. Tumors, like Bell’s palsy, may present with incomplete, complete, sudden, slowly progressive, or recurrent ipsilateral peripheral facial palsy. However, when a facial nerve palsy progresses for more than 3 weeks, a tumor must be excluded. In some cases of otherwise uncomplicated Bell’s palsy, examination of the spinal fluid reveals a pleocytosis and an increase in protein, without a microorganism being disclosed. Nonetheless, the presence of a CSF pleocytosis should prompt consideration of HIV infection, Lyme disease, sarcoidosis, and herpes infection24,25
In a case-control study,26 24.8% of patients with Bell’s palsy had diabetes, compared with an age-matched control group who had a 13.1% incidence of diabetes. This difference is highly significant and implies a direct relationship between diabetes and Bell’s palsy. Preservation of taste was significantly more common in patients with diabetes than in nondiabetics with Bell’s palsy. This finding in diabetic patients is in accordance with previously reported studies27 and suggests a lesion distal to the chorda tympani branch of the facial nerve.
Bell’s palsy appears to have a higher incidence during pregnancy. In one study,28 the calculated frequency in pregnant women was 45.1/100,000 births, compared with 17.4/100,000 per year in nonpregnant women of the same age group. Over 75% of the palsies occurred in the third trimester of pregnancy, and there was no apparent relationship between toxemia, primiparity, and hypertension.
Finally, there appears to be a genetic predisposition to Bell’s palsy. The incidence of a positive family history for Bell’s palsy in our patients was 14%. The reported frequency of a positive family history for idiopathic palsy has ranged from 2.4% to 28.6%.29,30
When one considers the degree of palsy and uses electromyographic data, the prognosis for recovery of facial function can be predicted with a high degree of accuracy. Ninety percent of patients will have a satisfactory recovery if the palsy is incomplete and the response to evoked electromyography (performed with supramaximal stimulation of the facial nerve at the stylomastoid foramen) remains greater than 10% of normal beyond the first 14 days after onset. Patients who do not fulfill these criteria nonetheless have at least a 50% chance of satisfactory recovery31 (i.e., complete or near complete return of facial function) (Table 4).32
TABLE 4. Classification System for Reporting Results of Recovery* | |||||||||||||||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| |||||||||||||||||||||||||||
Peitersen22 studied the natural history of over 1,000 patients with Bell’s palsy, seen over a 15-year period, and found that in 84% recovery was satisfactory; 71% recovered without sequelae, and 13% had defects that were barely noticeable. In the remaining 16% of patients with unsatisfactory recovery of facial function, the sequelae were “crippling” in only 4% (House grade IV or worse; see Table 4). There was not a single patient without some recovery, and 85% began to recover facial function within 3 weeks of onset of the palsy. Peitersen concluded that the sooner recovery is noted, the better the prognosis for satisfactory function.
A variety of viral agents have been associated with idiopathic facial palsy, but the herpes group of viruses has been the one most often implicated.33 On this basis, some authors have recommended the routine use of acyclovir in Bell’s palsy patients.34 A review of the literature on this issue found seroconversion rates of just 9.3% for varicella zoster virus and 3.7% for herpes simplex virus in patients with Bell’s palsy.33 A Swedish study of 147 patients with acute facial palsy found elevated viral titers in 9% of patients and elevated titers to Borrelia burgdorferi in another 11%. Despite extensive serologic testing, 67% of isolated facial palsy cases remained unexplained.35 However, a recent study of Bell’s palsy and herpes simplex virus supports a stronger viral relationship.36 By utilizing polymerase chain reaction techniques on endoneurial fluid and posterior auricular muscle tissue, Murakami and colleagues found herpes simplex type genomic material in 79% of patients tested.
The diagnostic evaluation of patients with acute facial palsy requires consideration of entities such as Lyme disease, HIV infection, sarcoid, herpes infection, syphilis, and a variety of meningeal processes. Magnetic resonance imaging (MRI) is not routinely performed in the evaluation of patients with Bell’s palsy. However, nonspecific gadolinium enhancement of the facial nerve is often observed. The severity of the facial palsy has no relationship to the findings on MRI, and the unaffected facial nerve may also show pathologic enhancement.37 Imaging should be performed in patients with associated vestibular symptoms, hearing loss, or if the palsy fails to improve after 6 months of observation.38
Treatment for Bell’s palsy is supportive, involving heat, massage, and facial exercises. Decompressive surgery has not been shown to alter the natural history of Bell’s palsy, and the use of steroids is controversial. For instance, there is no large, well-controlled study that unequivocally establishes the efficacy of steroids.39,40,41 At present, the decision regarding the use of steroids should be individualized. Considerations should include the patient’s age, the patient’s general medical condition, the duration and the completeness of the palsy, and the presence of pain. We do not use corticosteroids if it is possible that the facial palsy is caused by Lyme disease, because their administration may render this condition refractory to future antibiotic treatment. Although data is limited, the routine use of acyclovir in the treatment of Bell’s palsy is becoming more widely accepted. A recent small double-blind study of Bell’s palsy supports the combination of acyclovir and prednisone over prednisone alone.42 At this time, many experts favor the use of corticosteroids and acyclovir for the treatment of Bell’s palsy, however, further study is necessary to determine the optimal treatment.
INFECTIOUS AND IMMUNE-MEDIATED NEUROPATHIES
HERPES ZOSTER CEPHALICUS (RAMSAY HUNT SYNDROME)
Hunt first described the syndrome of herpes zoster cephalicus, which is characterized by a viral prodrome followed by severe pain in and around the ear, with vesicles involving the external canal and pinna.43,44 Vesiculation may involve the ear, face, neck, tongue, larynx, or buccal mucosa. The distribution of the vesicles depends on which sensory fibers are infected. Any of the nerve branches that communicate with the facial nerve may be involved, including cranial nerves V, VIII, IX, and X, and cervical nerves II through IV (Fig. 10). In the mildest form, neurologic signs are absent, whereas in severe cases there may be accompanying sensorineural hearing loss, disturbed vestibular function, and even viral encephalitis. Herpes zoster cephalicus is characterized by vesicles, a high incidence of eighth cranial nerve involvement, postherpetic pain, and a poorer prognosis for recovery of the facial palsy. The presence of hearing loss in a patient with suspected idiopathic facial palsy should strongly suggest varicella zoster virus infection.
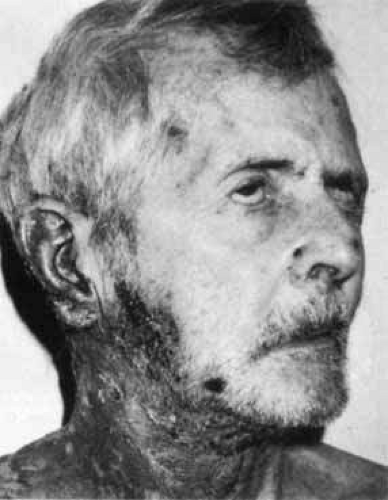 Fig. 10 Herpes zoster cephalicus, with Ramsay Hunt syndrome and cutaneous eruption in distribution of second, third, and fourth cervical nerves. |
The natural history of herpes zoster differs from that of Bell’s palsy in several ways, perhaps reflecting the difference in behavior between herpes simplex type I and the varicella-zoster viruses. Bell’s palsy recurs in some 12% of cases, but herpes zoster cephalicus rarely recurs. In addition, the acute phase of the infection, as measured by electrical response and progression of facial weakness, peaks at 5 to 10 days with Bell’s palsy, but at 10 to 14 days with herpes zoster cephalicus. Lastly, 84% of persons suffering from Bell’s palsy have a satisfactory recovery of facial function, in contrast to 60% of those with herpes zoster cephalicus.
Treatment of herpes zoster is similar to that of Bell’s palsy, but with the addition of therapeutics to control pain and vesicular eruption. Often, narcotics are required. Several studies have supported the efficacy of acyclovir in the treatment of herpes zoster cephalicus.45,46,47 One study also suggested that the combination of acyclovir and corticosteroids was superior to a regimen of corticosteroids alone.48
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree