Purpose
To determine whether an association exists between sleep apnea and open-angle glaucoma, normal-tension glaucoma, nonarteritic ischemic optic neuropathy (NAION), papilledema, or idiopathic intracranial hypertension (IIH) and whether treatment with continuous positive airway pressure affects the development of these conditions.
Design
Retrospective, longitudinal cohort study.
Methods
Billing records for beneficiaries 40 years of age and older enrolled in a large United States managed care network from 2001 through 2007 were reviewed. Incidence of open-angle glaucoma, normal-tension glaucoma, NAION, papilledema, and IIH were determined for the beneficiaries and were stratified by sleep apnea status. Cox regression analyses determined the hazard of each of these conditions developing among individuals with and without sleep apnea, with adjustment for sociodemographic, ocular, and medical conditions.
Results
Among the 2 259 061 individuals in the study, 156 336 (6.9%) had 1 or more sleep apnea diagnoses. The hazard of open-angle glaucoma was no different among persons with sleep apnea either treated (adjusted hazard ratio [HR], 0.99; 95% confidence interval [CI], 0.82 to 1.18) or untreated with continuous positive airway pressure (HR, 1.01; 95% CI, 0.98 to 1.05) and individuals without sleep apnea. Similar findings were observed when assessing the hazard of normal-tension glaucoma developing ( P > .05 for both comparisons). A significantly increased hazard of NAION developing (HR, 1.16; 95% CI, 1.01 to 1.33) and IIH (HR, 2.03; 95% CI, 1.65 to 2.49) was observed among individuals with sleep apnea who were not receiving continuous positive airway pressure therapy as compared with individuals without sleep apnea, although similar increased risks could not be demonstrated among continuous positive airway pressure-treated sleep apnea patients for these conditions ( P > .05 for both comparisons).
Conclusions
Patients with untreated sleep apnea are at increased risk for IIH and NAION. Clinicians should consider appropriate screening for these conditions in sleep apnea patients.
There has been conflicting evidence in the literature as to whether an association exists between sleep apnea and glaucomatous or other forms of optic neuropathy. Several studies have demonstrated a link between sleep apnea and open-angle glaucoma (OAG), normal-tension glaucoma (NTG), nonarteritic ischemic optic neuropathy (NAION), papilledema, and idiopathic intracranial hypertension (IIH). However, other studies have shown no relationship between glaucoma and sleep apnea. Use of continuous positive airway pressure as a treatment for sleep apnea also has been implicated as a cause of elevated intraocular pressure and has been questioned as an effective means of preventing optic neuropathy, whereas others studies recommend using continuous positive airway pressure to prevent glaucomatous or ischemic optic neuropathy.
Should such an association exist between sleep apnea and glaucoma or other optic neuropathies, it may provide clues to the pathophysiologic mechanisms by which the optic nerve can become damaged from hypoxia associated with episodes of apnea. Furthermore, if sleep apnea (or its treatment with continuous positive airway pressure) is associated with any of these sight-threatening conditions, this knowledge may help to inform guidelines for monitoring the health of the optic nerves among patients with sleep apnea or screening for sleep apnea among patients with disease of the optic nerves. This study used a large, national cohort to compare the incidence of glaucomatous and other forms of optic neuropathy among individuals with and without sleep apnea and to assess whether the hazard for these conditions is associated with sleep apnea or its treatment, continuous positive airway pressure.
Methods
Data Source
The i3 InVision Data Mart database (Ingenix, Eden Prairie, Minnesota, USA) contains detailed fully deidentified records of all beneficiaries in a large managed care network in the United States. We had access to data for beneficiaries in the Data Mart database who had any form of eye care from January 1, 2001, through December 31, 2007. This subset consisted of beneficiaries who had 1 or more International Classification of Diseases, 9th Revision, Clinical Modification (ICD-9-CM) code for any eye-related diagnosis (360 through 379.9), or Current Procedural Terminology (CPT-4) code for any eye-related visits, diagnostic or therapeutic procedures (65091 through 68899 or 92002 through 92499), or any other ICD-9-CM or CPT-4 codes adjudicated by an ophthalmologist or optometrist during their time in the medical plan. We had access to all beneficiaries’ medical claims (inpatient, outpatient, skilled nursing facility) for ocular and nonocular medical conditions. The database also contains detailed records of demographic (age, sex, race, or ethnicity) and socioeconomic (education, household net worth) information for each beneficiary.
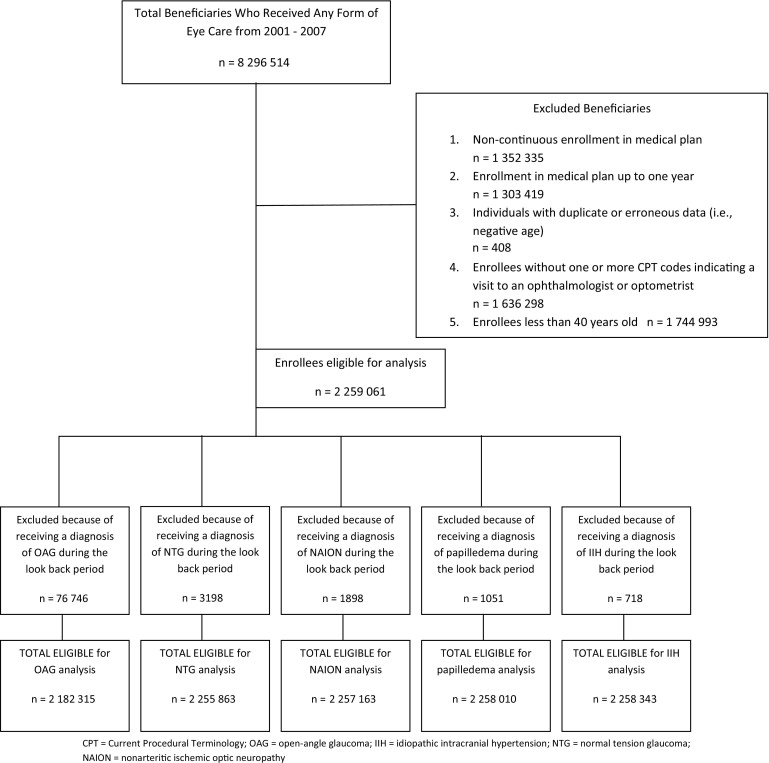
Patients
We identified all persons 40 years of age or older in the i3 InVision Data Mart database for more than 1 consecutive year and with at least 1 visit to an eye-care provider during their time in the medical plan ( Figure ). Patients were identified as having sleep apnea if they received 1 of more of these ICD-9-CM diagnostic codes at any point during their time in the medical plan: 327.2, 327.20, 327.21, 327.23, 327.27, 327.29, 780.53, 780.57, or 780.51. These codes reflect forms of obstructive and central sleep apnea, distinguished further by cause (e.g., organic, primary, or secondary) or accompanying symptoms, such as hypersomnia or insomnia. Obstructive sleep apnea resulting from repeated closure or near closure of the upper airway during sleep affects at least 3% of adult Americans and is much more common than central sleep apnea, in which decreased drive to breathe causes pauses in breathing. Treatment with continuous positive airway pressure was identified by 1 or more records of CPT-4 code 94660. Supplemental Table 1 (available at AJO.com ) shows the ICD-9-CM codes used to identify persons with each of these ocular conditions: OAG, NTG, NAION, papilledema, and IIH. A patient who received a diagnosis of suspected glaucoma but did not progress to OAG or NTG was not counted as experiencing either of these glaucoma types. The database does not contain information to determine whether persons diagnosed with 2 different ocular conditions listed above had them in the same eye. Therefore, individuals could be diagnosed with more than 1 of these ocular conditions. Sensitivity analyses were performed to assess whether the findings differed significantly by requiring a second, confirmatory diagnosis of the ocular condition of interest to address concerns about misclassification of enrollees.
Incidence rates of ocular conditions were calculated by dividing the number of newly diagnosed beneficiaries with the ocular condition of interest by their time in the plan at risk. Diagnoses were considered incident cases if the enrollee did not have any record of the ocular condition of interest during their first year in the medical plan. A test of rate ratios was performed to compare the incidence rates of each condition among beneficiaries who did and did not have sleep apnea and among those with sleep apnea who were receiving and did not receive continuous positive airway pressure.
Statistical Analyses
All analyses were performed using SAS software version 9.2 (SAS Institute, Cary, North Carolina, USA). Participant characteristics were summarized for the entire sample by using means and standard deviations for continuous variables and frequencies and percentages for categorical variables. Incidence estimates, stratified according to sleep apnea status, were generated for the following ocular conditions: OAG, NTG, NAION, papilledema, and IIH.
Next, Cox regression models were developed to determine the hazard of developing each ocular condition of interest. For the model, we used the first year that each beneficiary was enrolled in the medical plan as a look-back period. The purpose of the look-back period was to identify and exclude nonincident cases of each ocular condition of interest from the models. The models captured incident cases because individuals diagnosed with the ocular condition during the look-back period were excluded from the analysis. To avoid selection bias, follow-up of all enrollees started at 1 year after enrollment in the medical plan. Persons were followed up until the event (OAG, NTG, NAION, papilledema, IIH) developed or they were censored (either when they left the medical plan or the last day for which we had data, December 31, 2007). For each beneficiary, the age to event or the age to censoring was determined. The model was structured in a manner so that individuals must have received their sleep apnea diagnosis before experiencing the event (eg, an OAG diagnosis), because they are censored from the model at the time they experience the event. Using age as the time axis and sleep apnea status as the key predictor of interest, the Cox model was left-truncated at the age of index (1 year after entry into the medical plan). Adjustments were made for age (the time axis), sex, race, region of residence within the United States, education level, household net worth, and the following medical and ocular conditions: diabetes mellitus, systemic arterial hypertension, hyperlipidemia, obesity, systemic hypotension, migraine headache, cataract, pseudophakia or aphakia, diabetic retinopathy, macular degeneration, and Charlson Comorbidity Index, an overall measure of health ( Supplemental Table 1 , available at AJO.com ). A P value < .05 was considered statistically significant. The University of Michigan Institutional Review Board determined this study was exempt from requiring institutional review board approval.
Results
Of the 2 259 061 individuals in the medical plan who met the inclusion criteria, 156 336 individuals (6.9%) had received at least 1 diagnosis of sleep apnea during the study period. The mean age at entry into the plan for those without sleep apnea was 54.8 ± 10.5 years; among those with sleep apnea, the mean age at plan entry was 54.2 ± 9.2 years ( P < .0001). There were more males with sleep apnea and fewer Asian Americans with sleep apnea relative to other races ( P < .0001 for both comparisons; Table 1 ).
| Enrollees without SA | Enrollees with SA | Total No. | |||
|---|---|---|---|---|---|
| No. | % | No. | % | ||
| Female | 1 216 582 | 57.8 | 62 639 | 40.1 | 1 279 221 |
| Male | 885 934 | 42.1 | 93 678 | 59.9 | 979 612 |
| White | 1 421 023 | 86.5 | 113 985 | 88.2 | 1 535 008 |
| Black | 72 552 | 4.4 | 5763 | 4.4 | 78 315 |
| Latino | 92 696 | 5.6 | 6822 | 5.3 | 99 518 |
| Asian | 42 424 | 2.6 | 1679 | 1.3 | 44 103 |
| Other race | 14 995 | 0.9 | 1023 | 0.8 | 16 018 |
| < HS | 23 176 | 1.3 | 1599 | 1.2 | 24 775 |
| HS diploma | 582 087 | 33.3 | 47 796 | 35.1 | 629 883 |
| Some college | 669 154 | 38.3 | 54 292 | 39.9 | 723 446 |
| College diploma | 467 159 | 26.7 | 32 227 | 23.7 | 499 386 |
| Advanced degree | 4938 | 0.3 | 274 | 0.2 | 5212 |
To help validate whether the enrollees who had been diagnosed with sleep apnea indeed had this condition, we reviewed the records to determine the types of medical providers who provided care to these enrollees. Medical providers who frequently care for patients with sleep apnea include pulmonologists, neurologists, sleep specialists, and otolaryngologists. During their time in the plan, 128 050 (82%) of the enrollees who had been diagnosed with sleep apnea had at least 1 visit to 1 of these medical providers, and among those with sleep apnea who received treatment with continuous positive airway pressure, 4894 (92%) had seen 1 of these types of medical providers. Furthermore, 60% had at least 1 CPT-4 code for a polysomnogram or some other formal sleep study (CPT-4 codes 95800, 95801, and 95806 through 95810). Likewise, among those enrollees who were diagnosed with 1 of the 5 ocular conditions of interest for this analysis, more than 99% of these individuals had records indicating they were under the care of an ophthalmologist or optometrist. Among those who were diagnosed with OAG, 107 095 (81%) had undergone at least 1 visual field test during their time in the plan, and 75 564 (57%) had at least 1 record of undergoing ocular imaging (optical coherence tomography, confocal scanning laser ophthalmoscopy, or scanning laser polarimetry). Of note, not all of the providers caring for these patients may have had access to equipment to be able to perform some of these tests, and some patients may have been unable to undergo these tests because of ocular or systemic comorbidities.
Differences in Incidence of Optic Neuropathies in Persons with and without Sleep Apnea
In a total of 55 090 individuals, OAG developed over the course of 5 935 107 person-years of follow-up (while at risk), for an OAG incidence rate of 0.93%. There were no significant differences in the incidence of OAG among those with sleep apnea not receiving continuous positive airway pressure (0.94%), those with sleep apnea receiving continuous positive airway pressure (0.83%), and those without sleep apnea (0.93%). The overall incidence of NTG among those in the plan was 0.08%. Those without sleep apnea had an incidence rate of developing NTG of 0.08%, which was higher than those with sleep apnea who were not receiving continuous positive airway pressure (0.07%). Individuals with sleep apnea not treated with continuous positive airway pressure had higher incidence of NAION (0.07% vs 0.05%), papilledema (0.05% vs 0.03%), and IIH (0.04% vs 0.01%) relative to those without sleep apnea. Similarly, persons with sleep apnea receiving treatment with continuous positive airway pressure had higher incidence rates of NAION (0.09% vs 0.05%) and papilledema (0.07% vs 0.03%) compared with those without sleep apnea. The incidence of each ocular condition for sleep apnea patients with and without continuous positive airway pressure treatment did not differ significantly ( Table 2 ). It is important to note that these incidence rates are not adjusted for potential confounding factors.
| Characteristic | Patients with OAG | Glaucoma Suspects |
|---|---|---|
| Sex, n (%) | ||
| Male | 78 830 (46.4) | 167 663 (42.4) |
| Female | 91 087 (53.6) | 228 058 (57.6) |
| Race/ethnicity, n (%) | ||
| White | 115 378 (79.4) | 277 286 (81.8) |
| Black | 15 601 (10.7) | 24 371 (7.2) |
| Latino | 8970 (6.2) | 22 507 (6.6) |
| Asian | 4064 (2.8) | 11 376 (3.4) |
| Other | 1262 (0.9) | 3319 (1.0) |
| Estimated net worth, n (%) | ||
| < $25 000 | 12 599 (8.6) | 26 236 (7.6) |
| $25 000–75 000 | 10 011 (6.8) | 21 627 (6.3) |
| $75 000–150 000 | 19 292 (13.2) | 42 316 (12.3) |
| $150 000–500 000 | 65 603 (44.8) | 154 312 (44.9) |
| > $500 000 | 38 828 (26.5) | 99 244 (28.9) |
| U.S. region of residence, n (%) | ||
| Northeast | 28 959 (17.1) | 75 953 (19.2) |
| Southeast | 72 323 (42.6) | 156 979 (39.7) |
| Midwest | 48 949 (28.8) | 116 770 (29.5) |
| West | 19 476 (11.5) | 45 566 (11.5) |
| Other | 181 (0.1) | 406 (0.1) |
| Comorbid ocular conditions, n (%) | ||
| Other nerve a | 57 026 (33.6) | 72 190 (18.2) |
| Wet AMD | 3288 (1.9) | 3823 (1.0) |
| Macular edema | 4308 (2.5) | 6098 (1.5) |
| NPDR | 10 778 (6.3) | 18 343 (4.6) |
| PDR | 3924 (2.3) | 4504 (1.1) |
| Other retina b | 36 163 (21.3) | 66 866 (16.9) |
| Total, n | 169 917 | 395 721 |
a Other conditions that can affect the optic nerve, such as other types of glaucoma or optic neuropathy.
b Conditions other than diabetic retinopathy and macular edema that can affect the retina.
Univariate and Multivariable Analyses
Open-angle glaucoma
Before adjustment for confounding factors, persons diagnosed with sleep apnea who were not receiving treatment with continuous positive airway pressure had a 7% increased hazard of developing OAG (unadjusted hazard ratio [HR], 1.07; 95% confidence interval [CI], 1.03 to 1.10]). By comparison, in the unadjusted model, those with sleep apnea treated with continuous positive airway pressure (unadjusted HR, 1.01; 95% CI, 0.86 to 1.18) did not differ in their hazard of developing OAG relative to individuals without sleep apnea. After adjustment for confounding factors, neither sleep apnea patients with continuous positive airway pressure therapy (adjusted HR, 0.99; 95% CI, 0.82 to 1.18) nor those without it (adjusted HR, 1.01; 95% CI, 0.98 to 1.05) had increased hazards of developing OAG relative to persons without sleep apnea ( Table 3 ).
| OAG | NTG | NAION | Papilledema | IIH | ||||||
|---|---|---|---|---|---|---|---|---|---|---|
| Univariate HR | Multivariable HR | Univariate HR | Multivariable HR | Univariate HR | Multivariable HR | Univariate HR | Multivariable HR | Univariate HR | Multivariable HR | |
| Untreated SA | 1.07 (1.03 to 1.10) | 1.01 (0.98 to 1.05) | 0.95 (0.85 to 1.07) | 0.98 (0.86 to 1.12) | 1.41 (1.26 to 1.58) | 1.16 (1.01 to 1.33) | 1.70 (1.49 to 1.93) | 1.29 (1.10 to 1.50) | 3.25 (2.74 to 3.86) | 2.03 (1.65 to 2.49) |
| CPAP-treated SA | 1.01 (0.86 to 1.18) | 0.99 (0.82 to 1.18) | 0.85 (0.47 to 1.53) | 0.79 (0.38 to 1.67) | 1.96 (1.20 to 3.21) | 1.38 (0.76 to 2.50) | 2.32 (1.37 to 3.92) | 2.05 (1.19 to 3.56) | 1.95 (0.73 to 5.22) | 1.50 (0.56 to 4.03) |
Normal-tension glaucoma
Unadjusted and adjusted models showed no differences in hazard ratios of developing NTG for sleep apnea patients untreated with continuous positive airway pressure (adjusted HR, 0.98; 95% CI, 0.86 to 1.12) relative to persons without sleep apnea. Furthermore, the unadjusted and adjusted models demonstrated no differences in the hazard of developing NTG between continuous positive airway pressure-treated sleep apnea patients (adjusted HR, 0.79; 95% CI, 0.38 to 1.67) and persons without sleep apnea ( Table 3 ).
Nonarteritic ischemic optic neuropathy
In the unadjusted models, persons with sleep apnea not receiving treatment with continuous positive airway pressure had a 41% increased hazard of experiencing NAION (unadjusted HR, 1.41; 95% CI, 1.26 to 1.58) relative to individuals without sleep apnea. Those with sleep apnea receiving continuous positive airway pressure had a 96% increased hazard of developing NAION (unadjusted HR, 1.96; 95% CI, 1.20 to 3.21) relative to persons without sleep apnea. After adjustment for confounding influences, individuals with sleep apnea not treated with continuous positive airway pressure had a 16% increased hazard of experiencing NAION (adjusted HR, 1.16; 95% CI, 1.01 to 1.33) as compared with individuals without sleep apnea. By comparison, the adjusted hazard of experiencing NAION was no different between individuals with sleep apnea receiving continuous positive airway pressure and those without sleep apnea (adjusted HR, 1.38; 95% CI, 0.76 to 2.50; Table 3 ).
Papilledema
In the unadjusted models, individuals with sleep apnea not treated with continuous positive airway pressure had a 70% increased hazard of developing papilledema (unadjusted HR, 1.70; 95% CI, 1.49 to 1.93) relative to individuals without sleep apnea. Those with sleep apnea who were treated with continuous positive airway pressure had a 132% increased unadjusted hazard of papilledema developing (unadjusted HR, 2.32; 95% CI, 1.37 to 3.92). After adjustment for confounding factors, persons with sleep apnea not receiving continuous positive airway pressure had a 29% increased hazard of papilledema as compared with individuals without sleep apnea (adjusted HR, 1.29; 95% CI, 1.10 to 1.50). Those with sleep apnea receiving continuous positive airway pressure therapy had a 105% increased hazard of experiencing papilledema (adjusted HR, 2.05; 95% CI, 1.19 to 3.56) relative to individuals without sleep apnea ( Table 3 ).
Idiopathic intracranial hypertension
In the unadjusted models, sleep apnea patients not receiving continuous positive airway pressure had a 225% increased hazard of developing IIH (unadjusted HR, 3.25; 95% CI, 2.74 to 3.86) relative to persons without sleep apnea. For sleep apnea patients receiving continuous positive airway pressure, the unadjusted hazard of experiencing IIH was similar to that of persons without sleep apnea (unadjusted HR, 1.95; 95% CI, 0.73 to 5.22). After adjustment for confounders, sleep apnea patients not receiving continuous positive airway pressure had a 103% increased hazard of IIH (adjusted HR, 2.03; 95% CI, 1.65 to 2.49) as compared with individuals without sleep apnea. In the adjusted model, no differences were noted in the hazard of developing IIH for persons with sleep apnea receiving continuous positive airway pressure and individuals without sleep apnea (adjusted HR, 1.50; 95% CI, 0.56 to 4.03; Table 3 ).
In sensitivity analysis, the findings from each of the Cox regression models did not change significantly when requiring a confirmatory diagnosis of each ocular condition (results not shown).
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


