Purpose
To seek evidence of neurovascular compression of motor cranial nerves (CNs) in otherwise idiopathic neuropathic strabismus using high-resolution magnetic resonance imaging (MRI).
Design
Prospective, observational case series.
Methods
High-resolution, surface coil orbital MRI was performed in 10 strabismic patients with idiopathic oculomotor (CN III) or abducens (CN VI) palsy. Relationships between CNs and intracranial arteries were demonstrated by 0.8-mm thick, 162-μm resolution, heavily T2-weighted MRI in fast imaging using steady-state acquisition sequences. Images were analyzed digitally to evaluate cross-sectional areas of extraocular muscles.
Results
In one patient with CN III palsy, an ectatic posterior communicating artery markedly flattened and thinned the ipsilateral subarachnoid CN III. Cross-sections of the affected medial, superior, and inferior rectus muscles 10 mm posterior to the globe–optic nerve junction were 17.2 ± 2. 5 mm 2 , 15.5 ± 1.3 mm 2 , and 9.9 ± 0.8 mm 2 , significantly smaller than the values of 23.6 ± 1.9 mm 2 , 30.4 ± 4.1 mm 2 , and 28.8 ± 4.6 mm 2 , respectively, of the unaffected side ( P < .001). In 2 patients with otherwise unexplained CN VI palsy, ectatic basilar arteries contacted CN VI. Mean cross-sections of affected lateral rectus muscles were 24.0 ± 2.3 mm 2 and 29.8 ± 3.1 mm 2 , significantly smaller than the values of 33.5 ± 4.1 mm 2 and 36.9 ± 1.6 mm 2 , respectively, in unaffected contralateral eyes ( P < .05).
Conclusions
Nonaneurysmal motor CN compression should be considered as a cause of CN III and CN VI paresis with neurogenic muscle atrophy when MRI demonstrates vascular distortion of the involved CN. Demonstration of a benign vascular cause can terminate continuing diagnostic investigations and can expedite rational management of the strabismus.
When investigating the cause of strabismus caused by cranial nerve (CN) palsy, imaging studies often are necessary to rule out life-threatening intracranial lesions such as aneurysm and neoplasm. However, despite the availability of computed tomography and magnetic resonance imaging (MRI), the cause of neuropathic strabismus in 23% to 35% of patients still remains undetermined.
Ectasia of arteries is diagnosed when the diameter of the vessels exceeds normal along all or part of their course and when they are also abnormally tortuous. Previous study with cerebral angiography found that ectasia is associated with a variety of neurologic symptoms. Clinical syndromes may be caused by compression by sagging vessels against the cranial nerve root entry zones at brainstem. After Jannetta proposed this concept for hemifacial spasm, it was suggested that at least some cases of superior oblique myokymia, trigeminal neuralgia, hemifacial spasm, and vestibular paroxysmia are caused by vessels compressing the trochlear (CN IV), trigeminal, facial, and vestibulocochlear CNs. Theoretically, if CN III, CN IV, or CN VI were compressed by dolichoectatic vessels, associated ocular motility would be hindered and subsequent denervation atrophy of the involved extraocular muscle atrophy would be expected to develop within as little as 5 weeks based on findings in monkeys after experimental CN IV section. There have been few reports of neuropathic strabismus caused by presumed neurovascular compression in the literature review, mostly described cases with abducens nerve paresis. However, neurovascular compression rarely has been considered as a cause of neuropathic strabismus in clinical differential diagnoses. This may be because the pathologic anatomic features have not been demonstrable readily by conventional imaging studies.
With continuing advances of imaging technology, high-resolution MRI now can display the CNs and their innervation to extraocular muscles. CN anatomic relationships with intracranial vessels also can be demonstrated with refocus gradient-echo MRI sequence that is flow compensated. Using high-resolution MRI, we prospectively imaged patients with idiopathic CN III and CN VI palsy in whom routine clinical MRI and medical testing had been nondiagnostic, seeking evidence for nonaneurysmal neurovascular compression as a cause of neuropathic strabismus.
Methods
Subjects were identified from consecutive cases in an ongoing, prospective study of strabismus using high-resolution MRI. We included patients with CN III and CN VI palsy who had high-resolution imaging of the orbits and subarachnoid motor nerves innervating the extraocular muscles. All of these patients were referred for diagnosis of unexplained extraocular muscle weakness, consistent with CN palsy, after elsewhere having undergone conventional neuroimaging and typical clinical laboratory evaluation to exclude commonly recognized causes of cranial neuropathy. None of the patients exhibited fluctuation of strabismus or eyelid position, remission with recurrence of strabismus, connective tissue disease, or features suggestive of variable extraocular muscle weakness resulting from myasthenia gravis. Records of prior MRI and computed tomography studies were reviewed in all cases, and images were rereviewed when available.
We excluded patients with well-characterized alternative causes of strabismus, including history of trauma, neoplasm, intracranial surgery, diabetes, local infection, demyelination, myasthenia gravis, thyroid disease, and autoimmune disorders. In the sense that conventional causes could not be established after thorough evaluation, these patients were considered by the investigators to have idiopathic CN VI or CN III palsies.
Clinical Examination
All the strabismic patients underwent complete ophthalmic examinations by one of the authors (J.L.D.) who is a strabismus specialist. Examinations included assessment of visual acuity, stereopsis, orthoptic examination, Hess screen testing, slit-lamp and funduscopic examination, refraction, and photography in diagnostic gaze positions.
Imaging
Imaging of the orbits was performed using a 1.5-Tesla General Electric Signa scanner (Milwaukee, Wisconsin, USA), as previously described. Imaging of CNs at the brainstem was performed using the heavily T2-weighted fast imaging employing steady-state acquisition (FIESTA) sequence, which provides good contrast of the CNs against the surrounding cerebrospinal fluid. Detailed imaging techniques are summarized in the Appendix .
Images were analyzed digitally with the program OsiriX Medical Image software version 3.3.2 (Pixmeo, Geneva, Switzerland) on Macintosh computers (Apple Computer, Cupertino, California, USA). For measurement of cross-sectional areas of rectus muscles, the globe–optic nerve junction was identified first on each quasicoronal image. Muscle cross-sections then were identified in each of the 5 continuous image planes posterior to the globe–optic nerve junction. The borders of each extraocular muscle were outlined manually with a digital cursor, and its cross-sectional area was computed by the region of interest (ROI) function of the OsiriX software. Means and standard deviations were computed for the cross-section values for the 5 sampled planes. The maximum inferior oblique muscle cross-section was determined at the most temporal part of the straight path found in the quasisagittal image plane, passing through the center of the inferior rectus muscle that travels in this plane. The cross-sectional area of inferior oblique muscle in these images was selected for comparison with that of the unaffected side.
Statistical Analysis
Ipsilateral and contralateral cross-sectional areas of extraocular muscles were compared by the use of the 2-tailed t test. Statistical analyses were performed by SigmaStat software version 2.0 (SPSS Science, Inc, Chicago, Illinois, USA). P levels of .05 level were considered significant.
Results
Ten (28%) of the 36 total patients who underwent high-resolution MRI in the study who had CN VI or CN III palsies were considered idiopathic. There were 6 men and 4 women. The average age in the study group was 23.7 years (range, 3 to 55 years). Patients were all followed up for at least 6 months. Each of these exhibited palsy of a single CN innervating 1 or more extraocular muscles (EOMs), the clinical presentation and course of which could not be explained plausibly by ischemic mononeuropathy, mass lesion, vasculitis, or neuromuscular disease. High-resolution MRI demonstrated CN III hypoplasia in 3 patients, and schwannoma in the orbital portion of CN III in 1 patient. High-resolution MRI demonstrated unremarkable results in 3 patients. Abnormal neurovascular compression was found in 3 patients, whose cases are described here in detail.
Case Reports
Case 1
A 55-year-old woman had history of binocular diplopia beginning sometime after age 20 years. On 4 prior occasions over an extended interval, MRI of the head performed elsewhere had been interpreted as showing normal results. Although electromyographic and antibody evaluations for myasthenia gravis showed negative results, the diagnosis was nevertheless presumed, and she had undergone thymectomy at 23 years of age without benefit. She had undergone multiple strabismus surgeries, including right superior rectus recession, right lateral rectus recession, left inferior rectus recession, and left lateral rectus recession on the same occasion. A later surgery consisted of rerecession of the lateral rectus muscles and resection of both medial and the right inferior rectus muscles. Corrected visual acuity was 20/25 in the right eye and 20/30 in the left eye. The pupils were 6 mm in diameter, round, and appropriately reactive to light and accommodation without afferent pupillary defect. There was marked limitation of right eye supraduction and moderate limitation of left eye supraduction. There was profound limitation to adduction and infraduction of the right eye. At distance without correction, there was 55 Δ right exotropia. Slit-lamp examination results, intraocular pressure, and funduscopy results were normal. Hess screen testing demonstrated a central gaze exotropia exceeding 45 degrees with superimposed 26-degree right hypertropia.
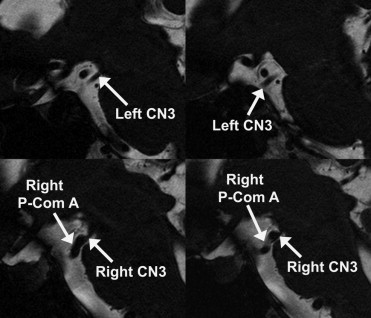
High-resolution MRI showed profound hypoplasia of the deep portion of the right inferior rectus, the right medial rectus, and the right superior rectus, as well as the right inferior and superior oblique muscles. Intraorbital motor branches of the right CN III were quite small. The subarachnoid portion of the right CN III was compressed by the prominent, hairpin contour right posterior communicating artery and posterior cerebral artery ( Figure 1 ). The right CN III was compressed markedly by the tortuous vessel, reducing its diameter to only 0.27 mm. The left oculomotor nerve in the same view had a normal diameter of 1.65 mm ( Figure 2 ).
Cross-sections of the affected medial, superior, and inferior rectus muscles 10 mm posterior to the globe–optic nerve junction were 17.2 ± 2.5 mm 2 , 15.5 ± 1.3 mm 2 , and 9.9 ± 0.8 mm 2 , respectively, significantly smaller than the values of 23.6 ± 1.9 mm 2 , 30.4 ± 4.1 mm 2 , and 28.8 ± 4.6 mm 2 , respectively, of the unaffected side ( P = .00059, P = .00049, P = .00010, respectively; Figure 3 ). The cross-sectional area of the right inferior oblique muscle was 17.0 ± 1.1 mm 2 , not significantly different from that of the left inferior oblique (18.8 ± 3.4 mm 2 ; P = .452). The average cross-sectional area of the lateral rectus was 30.2 ± 8.1 mm 2 on the right, not significantly different from the value of 28.4 ± 1.0 mm 2 on the left ( P = .768). The average cross-sectional area of the superior oblique muscle was, 8.0 ± 2.7 mm 2 on the right, not significantly different from the value of 8.5 ± 2.6 mm 2 on the left ( P = .750).
Case 2
An 11 year-old-boy was referred for acute onset of horizontal, binocular diplopia in levoversion for 3 months. Routine computed x-ray tomographic and MRI scans had been obtained elsewhere that showed unremarkable results. He had had no recent illnesses or trauma, no systemic weakness, and no personal history of migraine. Uncorrected visual acuity was 20/20 in each eye. There was no preauricular lymphadenopathy or blepharoptosis. The pupils reacted normally. There was a moderated deficiency of full abduction of the left eye that was associated with terminal slowing of the abducting saccade. At distance without correction, there was 6 Δ esotropia that increased to 30 Δ in levoversion and was eliminated in dextroversion. The patient was orthotropic at near. Hess screen testing showed approximately 20 degrees of esotropia in levoversion. Slit-lamp and funduscopic examinations demonstrated unremarkable results. Serologic testing showed negative results for myasthenia gravis, including acetylcholine binding antibody, blocking antibody, and antistriated antibody.
High-resolution MRI demonstrated no evidence of an intraorbital lesion involving CN VI. High-resolution imaging with FIESTA sequence readily demonstrated the right subarachnoid CN VI, but an ectatic basilar artery was seen in the location where the left CN VI should have been visible ( Figure 4 , Top). Magnetic resonance angiography confirmed the tortuous, ectatic basilar artery extending to the left side of the brainstem in the position normally occupied by CN VI ( Figure 4 , Bottom). The cross-sectional area of the left lateral rectus muscle was 24.0 ± 2.3 mm 2 , significantly smaller than the value of 33.5 ± 4.1 mm 2 on the right ( P = .00189; Figure 3 ). The average cross-sectional area of the right medial rectus muscle was 27.0 ± 5.2 mm 2 , not significantly different from the value for the left medial rectus muscle of 23.3 ± 1.6 mm 2 ( P = .189). The mean cross-sectional area of the superior rectus muscle was 24.5 ± 2.8 mm 2 on the right and 22.5 ± 3.6 mm 2 on the left ( P = .359). The mean cross-sectional area of the inferior rectus muscle was, 21.7 ± 6.8 mm 2 on the right, not significantly different from the value of 21.3 ± 2.6 mm 2 the left ( P = .907).
Case 3
A 52-year-old man reported gradually progressive horizontal, binocular diplopia in dextroversion for 4 years. He had undergone prior neurologic evaluation regarding his chronic migraine headaches without specific findings. Previous MRI and magnetic resonance angiography of the intracranial vessels had shown negative results. Corrected visual acuity was 20/16 in the right eye and 20/20 in the left eye. Pupil reactions and slit-lamp and funduscopic examination results in both eyes were unremarkable. The prism cover test at distance showed orthotropia in primary position, but 10 Δ esotropia in dextroversion. He was orthotropic at near vision. There was mild to moderate deficiency of full abduction of the right eye associated with abducting nystagmus. Abduction saccades were slowed in the right eye. The Hess screen testing demonstrated approximately 15 degrees of esotropia in dextroversion.
The right lateral rectus muscle was atrophic compared with the left lateral rectus muscle on axial MRI ( Figure 5 ). MRI of the brainstem and motor CNs demonstrated a normal left CN VI and a right-deviated basilar artery that closely contacted the right CN VI ( Figure 6 ). The cross-sectional area of the right lateral rectus muscle was 29.8 ± 3.1 mm 2 , significantly smaller than the value of 36.9 ± 1.6 mm 2 on the left side ( P = .0229; Figure 3 ). The average cross-sectional area of the right medial rectus muscle was 28.9 ± 3.6 mm 2 , not significantly different from the value of 28.3 ± 3.1 mm 2 on the left ( P = .785). The mean cross-sectional area of the right superior rectus muscle was 28.8 ± 7.6 mm 2 , not significantly different from that of the left at 25.6 ± 4.8 ( P = .447). The mean cross-sectional area of the right inferior rectus muscles was 26.6 ± 3.2 mm 2 , not significantly different from the left side value of 26.8 ± 2.4 mm 2 ( P = .881).




