Pathogenesis of Facial Aging
Facelift surgery or rhytidectomy, browlifts, and midface lifts are performed in an effort to redrape and suspend facial soft tissues to gain a more youthful appearance to the face. Facial aging has traditionally been attributed to the force of gravity causing soft tissue ptosis of the face as patient ages. The actual causes of facial aging are incompletely understood at this time, but the pathogenesis of the aging face continues to be a fascinating, hotly debated topic among physicians. In general, facial aging tends to occur in three dimensions and involves all tissue components of the face: skin, muscle and soft tissue, facial fat pads, and the bony facial skeleton.
Facial aging can be thought of occurring from superficial to deep, and tends to begin in the late twenties and thirties in the skin. Photodamage is defined as the functional and structural damage that occurs to skin after chronic exposure to ultraviolet radiation from the sun. The structural changes involve gradual thinning of the epidermis, flattening of the epidermal-dermal border, loss of collagen and thickness in the dermis, decrease in collagen Type I to Type III ratio, and reduction in the skin cellular and protein components. Lax skin with decreased collagen manifests through sagging and increased propensity to be wrinkled and furrowed.
Deeper into the facial soft tissues, muscle laxity and atrophy, as well as bony remodeling and resorption can potentiate the loss of facial, mandibular, and neck definition. These anatomic changes manifest clinically as brow ptosis, deepening of the nasolabial fold, jowling, blunting of the cervicomental angle, and platysmal banding (Figure 73–1). These features of the aging face are particularly amenable to correction with a rhytidectomy, platysmaplasty, midface lift, and/or browlift.
However, there are limitations to these surgical procedures. The surgeon must know that there are options to deal with aspects of the aging face for which a facelift or a browlift is not as effective. Although photodamage from the sun or tanning beds can increase the process of skin thinning, it causes fine skin wrinkling which may be more amenable to a skin treatment such as laser resurfacing or a chemical peel. Also, there is a gradual volume loss in the face which occurs over the time from change in facial fat pads and bony remodeling of the facial skeleton. Fat pads in the temporal and malar area lose volume, and the malar fat pad descends. Although a facelift may elevate the malar fat pad, additional augmentation of facial volume may be necessary with injections of autologous fat, fillers, or even implants.
Anatomy
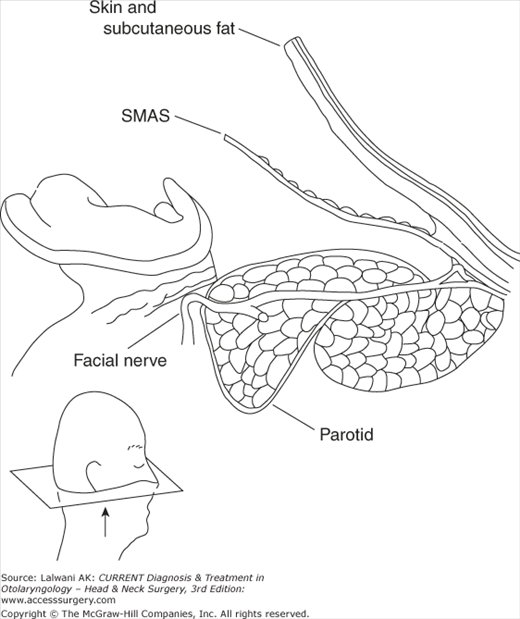
The key to understanding facelift surgery is understanding the anatomy of the superficial muscular aponeurotic system (SMAS) (Figure 73–2). The SMAS is a fibromuscular fascial layer that invests and interlinks the muscles of facial expression. It maintains consistent relationships with the vessels and nerves. The SMAS is contiguous with the platysma inferiorly and the temporoparietal fascia superiorly. In the temporal region, the frontal branch and the superficial temporal artery pierce this layer and become superficial. Inferior to this, the nerves and vessels are all deep to the SMAS, with motor innervations coming from the undersurface. Around the eye, the SMAS interdigitates with the orbicularis oculi. Medially, it has attachments to the zygomaticus major and minor as well as the dermis of the upper lip. The SMAS also has fascial condensations which are adherent to the overlying dermis and underlying muscle and bone. While not true ligaments, they are termed as such and act as support for the soft tissues of the cheek. The major osseocutaneous ligaments include the zygomatic ligament (McGregor’s patch) and mandibular ligament and the fascia–fascia retaining ligaments include the parotid and masseteric ligaments.
The platysma is innervated by the cervical branch of the facial nerve, a branch deep to platysma, and assists the depressor anguli oris in depressing the lower lip. As mentioned previously, the SMAS and platysma are contiguous; however, the location of the superior extent of the platysma is controversial and can be found up to 4 cm above the mandibular line and 3 cm below the malar eminence.
Medially, at the level of the thyroid cartilage, the platysma fibers interdigitate forming an inverted “V.” The apex can be at the level of the chin, or slightly below at the level of the thyroid cartilage. Because of this, the submental area may or may not be covered by the muscle fibers. If there is laxity or dehiscence of the anterior borders of the muscle, it creates banding in the midline, which occurs with age. Patients may then also have a chin droop, as the submental area lacks tissue. Laxity of the platysma can lead to “turkey gobbler” deformity and a more obtuse cervicomental angle. Flaccidity of superolateral fibers of the platysma muscle may be a contributing factor to chin droop and submental laxity.
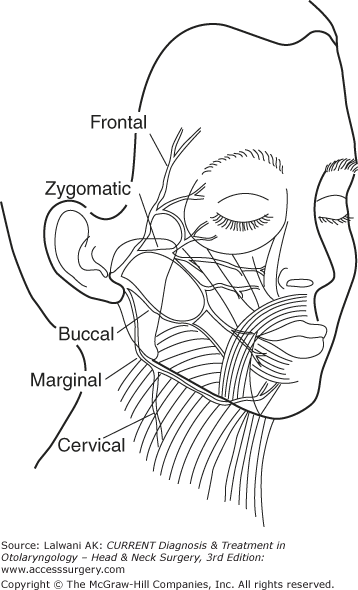
The facial nerve exits the stylomastoid foramen and courses through the parotid gland. It branches into five branches: temporal (or frontal), zygomatic, buccal, (marginal) mandibular, and cervical rami. (Figure 73–3) within the parotid gland, the main trunk usually divides a superior (temporofacial) and inferior (cervicofacial) branches. From there, the branching pattern becomes variable. There is frequent anastamosis between the zygomatic and buccal branches. After exiting the parotid gland in the face, the nerve branches are just deep to the parotideomasseteric fascia, which is a barely appreciable thin facial layer just deep to the SMAS.
Knowledge of the anatomy of the facial nerve is essential to avoiding nerve injury. The frontal and marginal branches are the most commonly injured branches in facelift. The frontal branch runs within the temporoparietal fascia and is superficial to the superficial layer of the deep temporal fascia. It crosses the zygoma midway between the tragus and lateral canthus of the eye. The marginal mandibular branch runs just deep to the platysma and can be found as low as the level of the hyoid bone, usually two fingerbreaths below the mandibular line.
Derived from second and third cervical nerves (C2 and C3), the greater auricular nerve provides sensation to the upper lateral neck and ear lobule. It emerges at the posterior border of the sternocleidomastoid muscle 6 cm inferior to the external auditory canal, wraps around this border, and ascends in the neck on the surface of the SCM. Eventually it gives off a small postauricular branch then pierces the parotid gland to provide its sensory innervation.
History of Facelift Techniques
Prior to the 1970s, much of facelift surgery involved a superficial skin dissection with the excision of excess skin. While this technique was popular at that time, skin excision did not provide a long-term benefit nor does it have any effect on the midface. Additionally, the technique tended to make patients look “over-pulled” and unnatural look. In the 1970s, facelift techniques changed dramatically with the description of the SMAS layer by Mitz and Peyronie. Skoog is credited with the development of SMAS manipulation. This began an era of different strategies to attain optimal vector pull for lax soft tissue and fat pad repositioning. The field is constantly evolving as evidenced by the push for minimally invasive techniques using smaller incisions and endoscopic instrumentation. The surgeon’s armamentarium is vast and the choice of which technique to use depends on a variety of factors.
Each patient is entirely different and requires a unique, individualized approach. The surgeon must thoroughly discuss the patients concerns and expectations. In addition, a full medical history and physical exam must be performed. A careful bleeding history should be taken to rule out need for hematologic consultation. A full list of medications, including over the counter and herbal supplements, must be obtained as many drugs can increase the risk of bleeding with surgery.
All patients should be photographed preoperatively. Standard photographic views include: frontal, right and left oblique, and right and left lateral. The reliability and consistency of the photographer is essential to the preoperative consultation. During the initial aesthetic consultation, each patient is evaluated for signs of facial aging, as well as intrinsic anatomic imbalances. A thorough facial analysis should be performed, and the surgeon should be prepared to diagnose photoaging of the skin, volume loss, bony abnormalities, and soft tissue deformities. Specifically, the signs of facial aging identified in patients who proceed to facelift surgery are jowling, neck laxity (with or without platysmal diastases), and midface descent. Patients are given options for treatment and counseled on expected outcomes. The surgeon must be certain that the patient has realistic expectations. The full surgical plan is discussed, including proposed areas of incisions and the reasoning behind placement of these incisions. Patients should also be counseled on all the risks of the surgery, which are discussed later.
Markings are made on the patients face in the holding area while sitting upright. This allows the surgeon to mark anatomical sites, which he or she needs to identify locations of the face during surgery. In Figure 73–4 it also allows the surgeon one last time to communicate with the patient about the surgical plan.
Once the patient is in the operating room, the patient’s hair is combed away from incision lines and rubber bands or petroleum jelly are used to keep hair away from the incisions. Preoperative hair rinse with betadine or chlorhexidine has been shown to decrease the rate of surgical site infections, as one dose of intravenous antibiotics has been given before surgery and within 1 hour of incision.
Anesthesia
Rhytidectomy can be performed with local anesthesia and sedation; however, many surgeons prefer to use general anesthesia because of the length of the procedure and meticulous dissection needed to prevent facial nerve injury. The airway can be secured with either a laryngeal mask airway or an endotracheal tube. Muscle paralytics should be avoided during any procedure that may necessitate intraoperative facial nerve identification.
With either sedation or general anesthesia, local infiltration of tissues is necessary for hemostasis, anesthesia, and enhanced tissue dissection planes. Knowledge of the maximum weight-based dose of the local anesthetic, either with or without epinephrine, is essential and the amount used should be communicated with the anesthesiologist.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree