12

Temporomandibular Disorders,
Masseteric Hypertrophy, and
Cosmetic Masseter Reduction
Temporomandibular disorder (TMD) is the most common cause of facial pain after toothache. Two forms exist, which can occur independently or simultaneously. The first is myogenous, or muscle related, and is the more common of the two types. The second is arthrogenous, or joint related.
Botulinum neurotoxin (BoNT) has been used successfully in the treatment of chronic pain syndromes of muscular origin and in various headache syndromes. In addition, BoNT has been proposed as an effective treatment for spastic conditions of the head and neck such as oromandibular dystonia and torticollis.1 Consequently, clinicians have started using BoNT for treatment of TMD, bruxism, and masseteric hypertrophy with success. In 2001, Von Lindern et al2 treated seven patients for masseter and temporalis hypertrophy and noted a marked decrease in the size of the affected musculature with no relapse after a follow-up period of 25 months. In a second larger study, the sample size was increased to 90 patients, and patients were randomized to receive either BoNT or saline; 90% of the patients receiving botulinum had a decrease in their chronic facial pain.
Freund and Schwartz3 treated 46 patients with BoNT/A for TMD symptoms and assessed them at 2- and 8-week intervals for subjective pain, mean maximum voluntary contraction, interincisal oral opening, and tenderness to palpation. All patients demonstrated an improvement in all outcome measures except maximum voluntary contraction. Maximum voluntary contraction was reported to decrease after 2 weeks but then revert to baseline levels at 8 weeks.
In an unpublished open label study by Bentsianov et al,4 the authors discovered a 70% response rate (defined as 50% reduction of severity and/or frequency of pain) when using BoNT injection into the masseter and temporalis muscles for TMD symptoms. Another study by Kurtoglu et al5 examined 24 patients who underwent either saline (placebo) or BoNT/A injection into the masseter and anterior temporal muscles. On days 14 and 28, electromyography (EMG) recordings were taken and each patient completed a subjective questionnaire, which revealed decreased muscle action potentials in 14 days and demonstrated improvement of pain and psychological status.5
Nixdorf et al6 reported in 2002 a randomized controlled trial of BoNT/A for chronic myogenous orofacial pain. This study involved 15 women with pain of masticatory muscles and showed no statistically significant differences between control and placebo groups and a decrease in maximal interincisal opening. However, this study involved only a small sample size, and many patients dropped out due to the tight restriction on analgesics (acetaminophen only).
 Anatomy
Anatomy
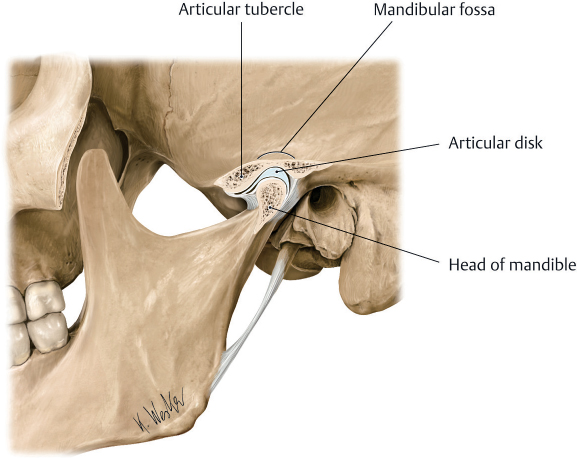
The temporomandibular joint is a synovial joint with articular surfaces on the condyle inferiorly, and articular tubercle and mandibular fossae of the squamous portion of the temporal bone superiorly. The articular surfaces are separated by an articular disk (or meniscus), which is a fibrocartilaginous structure providing a gliding surface for the condyle (Fig. 12.1).
Fig. 12.1 Temporomandibular joint. (From Atlas of Anatomy, © Thieme 2008, Illustration by Karl Wesker.)
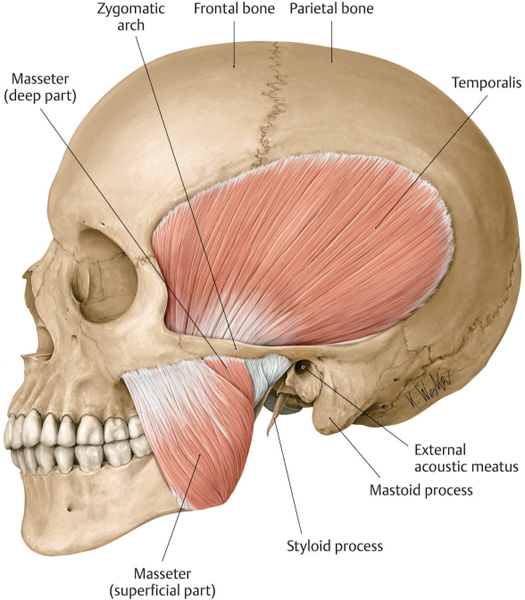
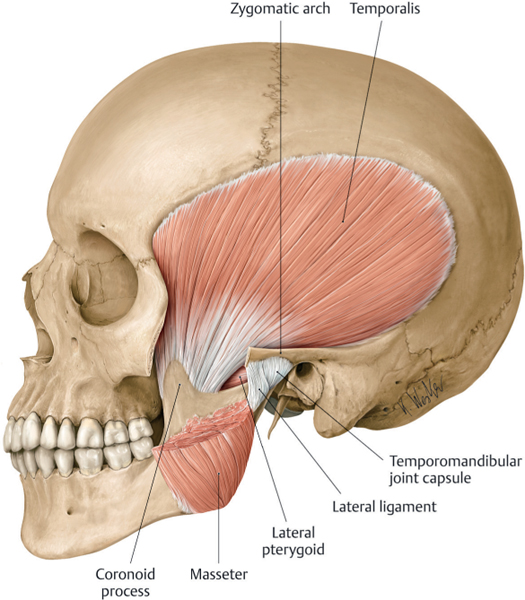
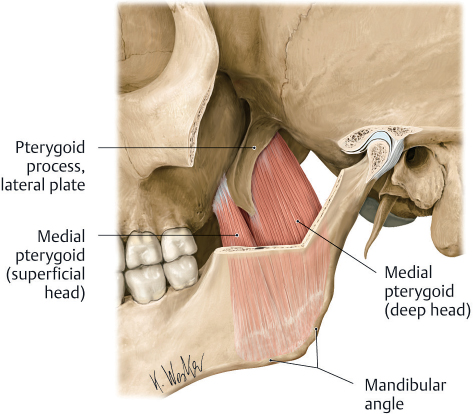
The adduction of the mandible (elevation or closing) is performed by the actions of the masseter (Fig. 12.2), temporalis (Fig. 12.3), and medial pterygoid (Fig. 12.4). The mandible is actively abducted (depressed or opened) by the lateral pterygoids (Fig. 12.5) and the supra- and infrahyoid musculature. Lateral excursion is allowed by actions of the contralateral pterygoids and masseter and the ipsilateral anterior portion of the temporalis muscles (Tables 12.1 and 12.2).
 Patient Selection
Patient Selection
Patients should be at least 18 years old and have had symptoms for at least 3 months that have been refractory to conventional treatments for at least 6 weeks. The following patients should not be considered for BoNT therapy: patients with proven arthrogenic TMD, those who have had prior surgery for TMD, and patients using medications that have an effect at the neuromuscular junction or who have another disorder that interferes with neuromuscular function (e.g., myasthenia gravis).