External & Middle Ear Trauma
- History of trauma to ear or foreign body insertion into the ear
- Symptoms of pain and hearing loss
- Bloody otorrhea.
Injuries localized to the external or middle ear include auricular hematoma, external auditory canal abrasion or laceration, tympanic membrane perforation, and ossicular chain dislocation. Local trauma to the tympanic membrane and ossicles can occur by a penetrating injury with objects such as a cotton-tipped applicator, a bobby pin, a pencil, or a hot metal slag during welding. In addition, barotrauma, such as a slap to the ear or a blast injury, can cause a tympanic membrane perforation or ossicular chain dislocation.
An auricular hematoma may present after a forceful blow to the external ear. It can be recognized as a tender swelling of the pinna that is fluctuant on palpation. The hematoma arises after the perichondrium is sheared off the cartilage of the auricle. This fluid accumulation needs to be drained to prevent chondronecrosis and lead to a misshapen pinna, commonly known as a “cauliflower ear” or “wrestler’s ear.” After incision and drainage, a compression dressing is sutured through the pinna to bolster the skin and perichondrium against the auricular cartilage, preventing reaccumulation of the fluid.
Injuries to the external auditory canal most commonly occur when a patient is trying to remove his or her own earwax with a cotton-tipped applicator or bobby pin. The injury is usually a simple abrasion or laceration. Treatment consists of using an antimicrobial otic drop to prevent bacterial or fungal superinfection of the area. Alternately, there may be a localized area of blood collection underneath the skin of the external auditory canal, called a bulla. Perforating the tense bulla with a sharp pick often helps to reduce the patient’s discomfort. Patients with diabetes have a high risk of developing external otitis from this type of injury because of their poor microcirculation. These patients need to be followed up closely to verify wound healing.
A tympanic membrane perforation can occur after the use of a cotton-tipped applicator, a bobby pin, a pencil, or the entry of a hot metal slag into the ear canal during welding. Finally, barotrauma, such as a slap to the ear or a blast injury, can cause a perforation. In all cases, patients usually complain of pain and hearing loss, and the perforation can be diagnosed by otoscopy. It is important to note how much of the tympanic membrane has been perforated. A central perforation does not involve the annulus of the eardrum, whereas a marginal perforation does. In addition, the Weber tuning fork test should be performed to verify that it radiates to the affected ear, and the eyes should be checked for nystagmus. If the Weber test does not radiate to the affected ear and the patient has nystagmus, it is likely that stapes subluxation with sensorineural hearing loss has occurred. This is termed a perilymphatic fistula and requires urgent treatment (see Perilymphatic Fistula, Treatment).
If no evidence of sensorineural hearing loss is found, no specific treatment is required because traumatic tympanic membrane perforations, especially central perforations, typically heal spontaneously. However, strict dry ear precautions should be followed to prevent water from getting into the ear. Instructions to the patient include no swimming and use of a cotton ball thoroughly coated with petrolatum (eg, Vaseline) in the affected ear during bathing. An audiogram should be performed after about 3 months to verify that hearing has returned to normal and that there is no ossicular chain discontinuity. If the perforation has not healed by 3 months, a tympanoplasty will likely need to be performed.
Penetrating trauma with objects such as a cotton-tipped applicator, a bobby pin, or a pencil can injure the ossicular chain (after perforating the tympanic membrane). Barotrauma, such as a slap to the ear, a blast injury, or rapid decent in an aircraft, can cause ossicular chain dislocation without tympanic membrane perforation. Ossicular chain dislocation with an intact eardrum manifests as a maximal (60 dB) conductive hearing loss. Ossicular chain dislocation with a perforated eardrum results in lesser degrees of hearing loss. Treatment in any case is middle ear exploration and ossicular chain reconstruction, with tympanoplasty if needed.
Temporal Bone Fractures
- History of blunt head trauma
- Symptoms of hearing loss and possibly vertigo and facial nerve palsy
- Signs include Battle sign, hemotympanum, and bloody otorrhea.
The skull base includes the frontal bone, the sphenoid bone, the temporal bone, and the occipital bone. A fracture in the skull base (otherwise known as a basilar skull fracture) must involve at least one of these bones and may involve all of them. Temporal bone fractures represent roughly 20% of all skull fractures. Risk factors include being male and under 21. The most common causes include motor vehicle accidents, falls, bicycle accidents, seizures, and aggravated assaults. Blunt trauma to the lateral surface of the skull (the squamous portion of the temporal bone) often results in a longitudinal fracture. A blow to the occipital skull may go through the foramen magnum and result in a transverse fracture of the temporal bone (Figure 59–1).
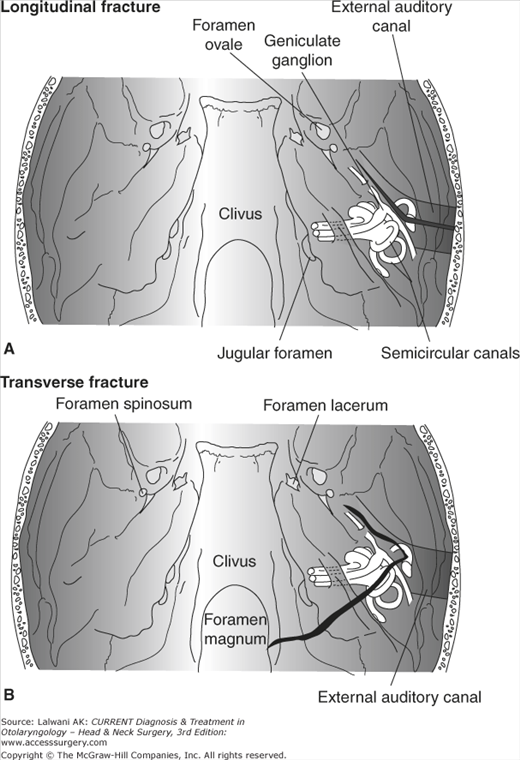
Figure 59–1.
Types of temporal bone fractures. (A) Longitudinal fractures begin at the squamous portion of the temporal bone, run through the external auditory canal, and then turn anteriorly toward the foramen lacerum. (B) Transverse fractures begin from the foramen magnum, run through the otic capsule bone that surrounds the inner ear, and then turn anteriorly toward the foramen lacerum.
Longitudinal fractures involve the squamous portion of the temporal bone, follow the axis of the external auditory canal to the middle ear space, and then course anteriorly along the geniculate ganglion and eustachian tube, ending near the foramen lacerum. In a longitudinal temporal bone fracture, the otic capsule is spared. In contrast, transverse fractures course directly across the petrous pyramid, fracturing the otic capsule, and then extend anteriorly along the eustachian tube and geniculate ganglion. Longitudinal temporal bone fractures and transverse temporal bone fractures represent 80% and 20%, respectively, of temporal bone fractures.
Symptoms include hearing loss, nausea and vomiting, and vertigo. Clinical signs include Battle sign, which is a postauricular ecchymosis resulting from extravasated blood from the postauricular artery or mastoid emissary vein. The “raccoon” sign (periorbital ecchymosis) is associated with basilar skull fractures that involve the middle or anterior cranial fossa. Physical examination may demonstrate an external auditory canal laceration with bony debris within the canal. A hemotympanum is almost always identified. Cerebrospinal fluid (CSF) otorrhea or rhinorrhea may be seen. Tuning fork tests should always be performed on patients with a temporal bone fracture. The Weber tuning fork test radiates to the fractured ear if conductive hearing loss is present and radiates to the contralateral ear if sensorineural hearing loss is present. The presence or absence of facial nerve paralysis should be documented in all patients with temporal bone fractures.
After initial resuscitation in the emergency room, computed tomography (CT) scanning of the head is usually the first study performed on patients with head trauma. It is critical to rule out an intracranial hemorrhage, which may require urgent neurosurgical treatment. It is at this point that a temporal bone fracture is usually identified. High-resolution CT scanning of the temporal bone is valuable in delineating the extent of the fracture, but it is not required unless a complication is suspected (eg, otic capsule fracture, facial nerve injury, or CSF leak). Patients with a longitudinal fracture associated with hemotympanum, without nystagmus, without evidence of CSF leak, with a Weber tuning fork test that radiates to the affected ear, and with normal facial nerve function typically do not need a CT scan of the temporal bone. Angiography may be performed if there is significant hemorrhage from the skull base to rule out vascular injury, but this is uncommon.
Audiometry should be performed on all patients with a temporal bone fracture. However, this does not need to be done acutely in most cases. If clinical examination is consistent with conductive hearing loss and there is no evidence of otic capsule fracture, audiometric assessment can be performed several weeks after the injury, permitting time for the hemotympanum to resolve. If the otic capsule is fractured, there is a high likelihood of permanent complete sensorineural hearing loss and there is no treatment available to alter this prognosis. Urgent audiometry may be considered if stapes subluxation into the vestibule has occurred and surgery to repair a perilymph fistula is planned.
Facial nerve testing should be performed if a delayed, complete facial palsy occurs. The rationale is to identify patients with >90% degeneration of the facial nerve, because these patients have poorer recovery of the function and may benefit from surgical decompression. The nerve excitability test is performed by placing the two probes of a Hilger nerve stimulator across the stylomastoid foramen and slowly turning up the current until a facial twitch is just barely visible. This is the stimulation threshold of the facial nerve. A 3.5-mA difference between the injured and uninjured sides correlates with a > 90% loss of neural integrity.
Alternately, electroneuronography can be performed by a neurophysiologist. This involves stimulating both facial nerves with equal currents while simultaneously measuring the evoked myogenic potential in the muscles of facial expression. If the amplitude of the ipsilateral evoked potential is < 10% of that from the contralateral side, >90% loss of neural integrity has occurred. Neither of these tests is accurate within 3 days of the injury because it takes about 72 hours for nerve fibers distal to the site of the injury to degenerate. Nonetheless, surgical decompression of delayed facial paralysis remains controversial.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree