SYSTEMIC AND IMMUNOLOGIC CONDITIONS AFFECTING THE CORNEA
WILSON’S DISEASE (HEPATOLENTICULAR DEGENERATION)
Wilson’s disease is a rare condition resulting in abnormal copper deposition throughout the body.
Etiology and Epidemiology
• Autosomal recessive condition caused by a deficiency of the enzyme ceruloplasmin
• Onset under age 40 years
Symptoms
• Usually no ocular symptoms
• May experience cirrhosis, renal disease, or neurologic dysfunction (typically motor disorders)
Ocular Signs
• Kayser-Fleischer ring: green-brown band of copper deposition in the peripheral zone of Descemet’s membrane (Figure 8-1; see also Figure 6-8). This ring usually begins in the vertical meridians and may be seen earliest with gonioscopy. A Kayser-Fleischer ring may be the presenting sign of the disease.
• Cataract is found in less than 10% of cases. A disc-shaped, central, polychromatic opacity with peripheral radiations can be seen (sunflower cataract).
Figure 8-1 Wilson’s disease A prominent Kayser-Fleischer ring can be seen. Brown copper pigment deposition is very apparent in the corneal periphery in this 18-year-old woman with Wilson’s disease. The deposits are at the level of Descemet’s membrane and deep stroma. In mild cases, the copper pigment is seen earliest using gonioscopy. See also Figure 6-8.
Differential Diagnosis
• Other causes of a Kayser-Fleischer ring: primary biliary cirrhosis, chronic active hepatitis, multiple myeloma
• Chalchosis: corneal copper deposition from an intraocular copper foreign body
Diagnosis
• Slit-lamp or gonioscopic examination
• Serum copper and ceruloplasmin levels, urine copper level
Treatment
• Treatment by an internist and/or neurologist with copper chelating agents such as D-penicillamine or tetrathiomolybdate.
Prognosis
• Good with early recognition and treatment. Treatment may be followed by resolution of the Kayser-Fleischer ring.
VITAMIN A DEFICIENCY
Vitamin A deficiency is a rare, potentially blinding disorder usually affecting the malnourished that is common in areas where polished rice is the main source of food.
Etiology
• Dietary deficiency of vitamin A, typically from chronic malnutrition
• Celiac diseases, biliary obstruction, cystic fibrosis, pancreatic or intestinal (e.g., gastric stapling) surgery, which impairs absorption of vitamin A
Symptoms
• Night blindness is the earliest symptom, dry eye, foreign body sensation, gradual loss of vision in severe cases
Signs
• Xerosis of cornea and conjunctiva
• Keratinization of conjunctiva (Bitot’s spot: superficial, triangular, silvery-gray, foamy, keratinized patch on the interpalpebral bulbar conjunctiva)
• Sterile corneal ulcers and melts (keratomalacia) which may lead to scarring or perforation (Figure 8-2).
Figure 8-2 Vitamin A deficiency This malnourished patient had severe xerosis of the cornea and conjunctiva. There was a deep sterile corneal melt near the limbus from the 6 to 7 o’clock positions. The xerosis and melt resolved over a week with systemic vitamin A therapy.
Differential Diagnosis
• Keratoconjunctivitis sicca
Diagnosis
• Serum vitamin A level.
• Consider impression cytology of the conjunctiva (demonstrates decreased goblet cell density) and electroretinogram.
Treatment
• Systemic vitamin A orally or intramuscularly and repeated 1 month later.
• Frequent preservative-free artificial tear drops or ointment to lubricate ocular surface.
• Treat malnutrition.
• Corneal transplantation for scars or perforation. Consider a keratoprosthesis for bilateral severe scarring.
Prognosis
• Very good if diagnosed and treated before significant corneal ulceration has occurred. Fair to poor if significant corneal damage is present.
CYSTINOSIS
Cystinosis is a rare disorder resulting in accumulation of cystine in the body.
Etiology and Epidemiology
• Autosomal recessive disorder.
• Results in deposits of the amino acid cystine in the conjunctiva, corneal stroma, iris, lens, and retina depending on severity.
Three Main Forms
• Infantile: associated with dwarfism and progressive kidney dysfunction. Poor prognosis without a renal transplant.
• Adolescent (intermediate): kidneys may be involved, but retina normal.
• Adult: minimal to no kidney disease, cystine deposits limited to anterior segment.
Symptoms
• Irritation, foreign body sensation, pain, occasionally decreased vision
Signs
• Myriad tiny, glistening crystals in the corneal stroma, conjunctiva, iris, lens, and retina, depending on the severity of the disease (Figures 8-3A,B).
• May have superficial punctate keratopathy, filaments, and recurrent erosions.
• There is growth retardation, renal failure, hepatosplenomegaly, and hypothyroidism.
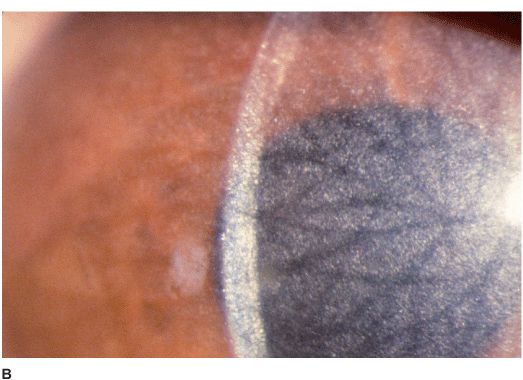
Figure 8-3 Cystinosis A. Confluent full-thickness tiny refractile corneal deposits are seen. These opacities are cystine crystals. Generally, the deposits do not affect vision; however if severe, they can cause significant visual symptoms. B. Slit-lamp beam view of the eye with cystinosis seen in Figure 8-3A. Note the full-thickness distribution of the crystals.
Differential Diagnosis
• See Crystalline Keratopathy in Chapter 6, page 137.
Treatment
• Lubrication for ocular surface disease.
• Cysteamine eye drops have been reported to be useful.
• Rarely, a corneal transplant is required.
Prognosis
• Poor for the infantile form, good for the intermediate and adult forms.
MUCOPOLYSACCHARIDOSES AND LIPIDOSES
A group of inherited systemic metabolic disorders resulting in abnormal accumulation of material in the body.
Etiology and Epidemiology
Mucopolysaccharidoses Lysosomal storage diseases including Hurler, Scheie, Hunter, Sanfilippo, Morquio, Maroteaux-Lamy and Sly syndromes. All are autosomal recessive except Hunter syndrome which is X-linked recessive.
Lipidoses Numerous disorders of lipid metabolism, including Fabry’s disease. All lipidoses are autosomal recessive except Fabry’s disease which is X-linked recessive.
Ocular Signs
Mucopolysaccharidoses All may have optic nerve, retinal, and CNS abnormalities. All have progressive corneal clouding except Hunter and Sanfilippo (Figure 8-4).
Lipidoses All may have macular cherry-red spots and optic atrophy. Bilateral, symmetrical, brownish corneal epithelial deposits arranged in a vortex fashion from a point below the pupil and swirling outward but sparing the limbus (cornea verticillata) is seen in males with Fabry’s disease and female carriers. Conjunctival aneurysms, lens opacities, papilledema, optic atrophy, and macular and retinal edema are also seen in Fabry’s disease.
Figure 8-4 Maroteaux-Lamy syndrome Diffuse full-thickness corneal haze can be seen in this child with Maroteaux-Lamy syndrome.
Treatment
• Severe corneal opacity may require a corneal transplant. No ocular treatment is required for cornea verticillata.
• Follow-up with a pediatrician or pediatric endocrinologist.
Prognosis
• Poor to good depending on the specific metabolic disorder.
COLLAGEN VASCULAR DISEASES
Collagen vascular diseases can cause a wide variety of ocular abnormalities, the most important of which is scleritis.
Etiology
• Rheumatoid arthritis (most common)
• Wegener’s granulomatosis (often causes a necrotizing scleritis)
• Polyarteritis nodosa
• Relapsing polychondritis
• Systemic lupus erythematosus (SLE)
Symptoms
• Range from minimal to significant pain, redness, discharge, decreased vision.
Signs
• Corneal findings include keratoconjunctivitis sicca, stromal keratitis, corneal stromal infiltrates or ulceration, typically peripheral but may be central. The peripheral corneal ulceration may occur with or without inflammation. The ulceration can be similar to Mooren’s ulcer in that it can extend circumferentially and centrally. However, unlike Mooren’s ulcer, the sclera is commonly involved. Corneal perforation may occur (Figures 8-5A,B,C).
• Other findings include episcleritis, scleritis (necrotizing with or without inflammation) and sclerokeratitis (Figure 8-5D). Healed episodes of scleritis can lead to scleral thinning and uveal show (Figure 8-5E).
• The corneal changes in SLE are often unremarkable.
Figure 8-5 Rheumatoid arthritis A. Slit-lamp beam view of a patient with rheumatoid arthritis demonstrates a peripheral corneal melt with severe ulceration. There is approximately 90% tissue loss. There is moderate corneal neovascularization peripherally and superiorly. Note the area of clear cornea superiorly; it is an additional large area of corneal melting. B. This patient with rheumatoid arthritis has three separate peripheral corneal infiltrates from the 9 to 11 o’clock positions. There is an additional, larger peripheral infiltrate with corneal melting from the 12 to 2 o’clock positions. The infiltrates are most likely sterile, inflammatory infiltrates. Rheumatoid arthritis C. This eye has a large sterile corneal melt leading to perforation in the midperiphery at the 5 o’clock position. The radiating stromal folds suggest a perforation. Peripheral corneal neovascularization and scarring from the 3 to 4 o’clock positions indicates previous corneal inflammation in that area. Wegener’s granulomatosis D.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree