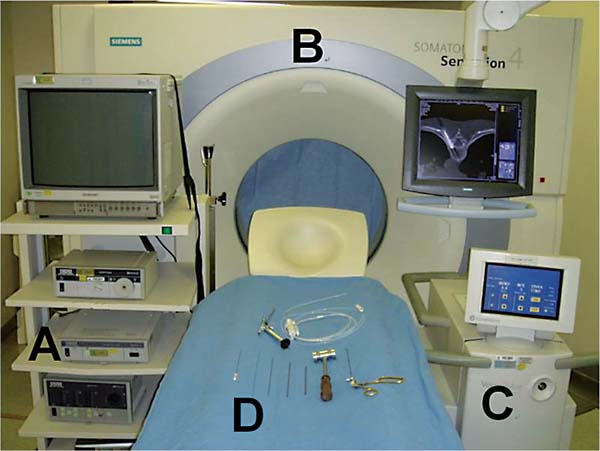
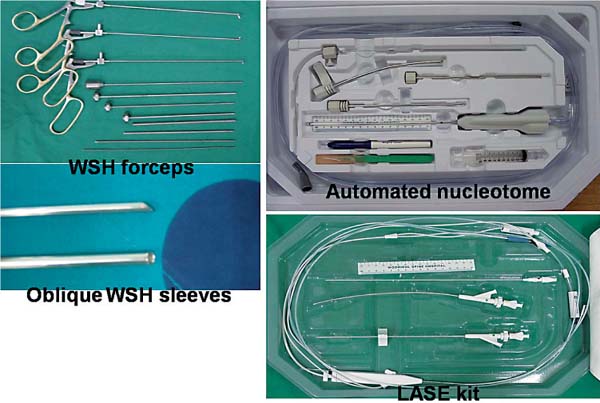
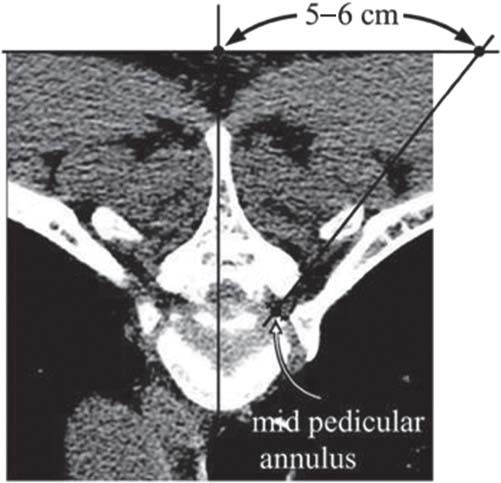
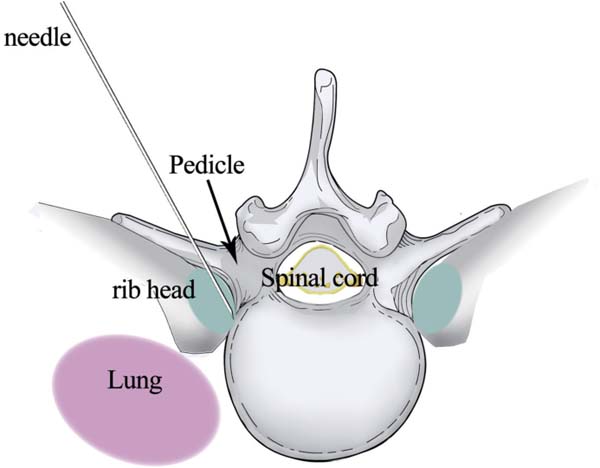
11 Surgical Techniques in Percutaneous Endoscopic Thoracic Diskectomy There are two types of percutaneous procedures currently available: • Percutaneous thoracic disk decompression (PTDD) with laser-assisted spinal endoscopy (LASE) with or without computed tomographic (CT) guidance (CTG-PTDD) • Percutaneous endoscopic thoracic diskectomy (PETD) using a working channel endoscope The operating room setup and instrumentation needed for percutaneous thoracic procedures are shown in Figs. 11.1 and 11.2. A CT scan and magnetic resonance imaging (MRI) are mandatory for preoperative planning, not only to determine if the patient is a candidate for a percutaneous thoracic procedure but also to plan the needle trajectory. Axial MRI or CT is used to calculate the needle’s skin entry point. The lateral coordinates of the skin entry point are determined by extrapolating a line from the midpedicular annulus to the lateral margin of the facet and extending up to the skin’s surface (Fig. 11.3). • The patient is positioned prone on a radiolucent operating table with the affected side facing the surgeon. • The arms are positioned above the patient. • The endoscopic and fluoroscopic monitors are positioned opposite the surgeon to facilitate viewing. Fig. 11.1 (A) Endoscopic set. (B) CT scan. (C) Ho:YAG laser. (D) Endoscope (KESS, Richard Wolf Medical Instruments Corporation, Vernon Hills, Illinois), dilators, and forceps. Fig. 11.2 Instruments necessary to perform a percutaneous endoscopic thoracic diskectomy. • Conscious sedation with midazolam and fentanyl allows continuous feedback from the patient during the entire procedure to avoid any damage to neural structures. • Midazolam is administered in the dose of 0.05 mg/kg intramuscularly 30 minutes before surgery followed by another dose intravenously during the operation if required. • The pathway from the skin to the facet is infiltrated with 1% lidocaine. Fig. 11.3 Measurements done over an axial CT scan to determine the skin entry point. • The appropriate operative level must be precisely located using lateral and anteroposterior (AP) fluoros-copy, counting the level from the sacrum or C1. • This procedure requires continuous fluoroscopic or interventional CT guidance. CT guidance is more precise. • Because the thoracic disk is more concave than the lumbar disks, lumbar fluoroscopic landmarks cannot be used for thoracic disks. Because of this concavity, thoracic disk herniations can only be approached through the foraminal region. • The skin entry point is determined with a preoperative axial CT scan based on an imaginary line projected toward the skin from the target area (between the rib and facet). • The safe route for the needle into the thoracic disk passes between the rib head and the thoracic facet (Fig. 11.4). • Routinely, the skin entry point is around 4 to 7 cm lateral to the midline. • A more lateral approach is required for larger patients to reduce any manipulation of the spinal cord during disk removal. • Always be careful to keep the needle posterior to the rib head because the pleura is located anterior to the ribs (Fig. 11.5). Fig. 11.4 Needle trajectory between the rib head and facet joint.
Special Instruments and Preoperative Planning
Position and Anesthesia
Needle Insertion Technique
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree