Fig. 1
27-week gestation fetus with a white arrow pointing toward a large solid-cystic cervical mass
Prenatal Evaluation
The prenatal identification of a fetus with potential airway obstruction warrants a comprehensive anatomical evaluation to determine the need for a special delivery strategy. Early diagnosis is essential so that the mother can be referred to a center with EXIT and fetal surgery capabilities. The prenatal evaluation not only includes a number of imaging studies (fetal ultrasound, 3D ultrasound, fetal echocardiography, fetal MRI) but also an amniocentesis for fetal karyotype (Fig. 2). Additional genetic studies may be warranted depending on the presence of associated findings. Care must be taken to assess the placenta, as abnormal placentation such as placenta previa or evidence of subchorionic hemorrhage might increase the risk of intraoperative complications (see chapter on “Prenatal Assessment and Perinatal Management of Suspected Airway Compromise in the Fetus and Neonate” for full description).


Fig. 2
Three-dimensional ultrasound view of a fetus with large cervical teratomas
Multidisciplinary Team and Equipment
In centers prepared to handle post-neonatal airway obstruction, a multidisciplinary team that is familiar with the equipment and surroundings must be present. This team includes anesthesiologists, pediatric surgeons, neonatologists, maternal fetal medicine specialists, and a dedicated group of diverse nursing staff. Simulation and comprehensive preoperative planning are essential to successfully perform an EXIT procedure and likely surgical resection thereafter (Fig. 3 and Table 1). Our approach includes a mandatory team meeting 1–2 days before the surgery in which the particular case is extensively analyzed; the planned procedure is reviewed step by step; parents are counseled one additional time with all team members present; and informed consent is obtained. A variety of airway equipment needs to be available including a rigid infant-type laryngoscope handle, a set of number 0, 1, and 2 straight Miller blades, a set of rigid ventilating bronchoscopes sizes 2.5 and 3.0, a set of wire-reinforced cuffless endotracheal tubes (ETTs) and tracheostomy tubes, and all surgical instruments required for a neonatal tracheostomy (Fig. 4). In addition, a sterile Mapleson circuit with a manometer and a 1-L bag must be ready on the operating table to manually ventilate the fetus once the airway has been established. In our institution our operating area includes two large operating rooms (one for the EXIT and one for any potential immediate post-EXIT procedures on the newborn) connected by a neonatal resuscitation room.



Fig. 3
Multidisciplinary team at the operating table
Table 1
Multidisciplinary teams required for each stage of the EXIT procedure
Preoperative team | Intraoperative team | Postoperative team |
|---|---|---|
High risk obstetrician | High risk obstetrician | Neonatologist |
Pediatric surgeon | Pediatric surgeon | Pediatric surgeon |
Radiologist | Anesthesiologist | Nurse practitioners |
Anesthesiologist | Fetal cardiologist | Nurses |
Fetal cardiologist | Scrub nurses | Radiologist |
Social worker | Circulating nurses | Standby OR team |
Coordinator | Standby ECMO team | Standby ECMO team |

Fig. 4
A separate table with all the airway equipment must be available at the time of the surgery
Timing of Delivery
Ideally, fetuses with airway obstruction should reach term and be delivered electively. Depending on the cause of the airway obstruction and the effects on the fetal health, this may not be possible. For instance, fetuses with large cervical tumors that compress the airway can also suffer compression of the pharynx/esophagus, which can lead to polyhydramnios and preterm labor. When a fetus with airway obstruction develops signs of impending labor (i.e., severe recurrent polyhydramnios, shortened cervix), it is better to perform an elective preterm EXIT at a time that all the required personnel is available, than waiting for the fetus to reach term at the risk of developing labor at a time that not all the resources necessary for an EXIT are readily available. In a previously large series of fetuses with cervical teratomas, only 23 % of the fetuses reached term [8].
Surgical Technique: The EXIT Procedure
The EXIT procedure must be performed under deep general anesthesia because the general anesthetic drugs are the strongest uterine relaxants known to date. An epidural catheter is placed to facilitate maternal postoperative pain management. Intraoperative maternal monitoring includes pulse oximetry, continuous electrocardiogram, invasive arterial blood pressure monitoring (radial artery angiocatheter), urinary output via a bladder catheter, core body temperature, and peripheral nerve stimulation. The combination of drugs used for induction and maintenance of anesthesia during an EXIT procedure can vary, but the principle of deep inhalational anesthesia must not change. Generally, induction is done with intravenous propofol (2 mg/kg) immediately followed by a muscle relaxant (succinylcholine, 1 mg/kg) for a rapid endotracheal intubation. Maintenance is done with desflurane, titrated between 5 and 10 % according to the uterine tone evaluated by palpation during the operation. Muscle relaxation is maintained with vecuronium (0.1 mg/kg/dose, repeated as needed). The deep maternal anesthesia required to facilitate uterine relaxation can induce maternal hypotension, which is treated with an alpha-1-adrenergic agonist (phenylephrine) as a continuous infusion (10–200 μg/min) throughout the operation to maintain the maternal mean arterial pressure above 60 mmHg. Dopamine can be added as needed, as a continuous infusion. As soon as the procedure is completed and the umbilical cord is clamped, oxytocin (50 U) is given intravenously to the mother to induce uterine contraction. Other drugs can be used if necessary, like methylergonovine and carboprost or misoprostol.
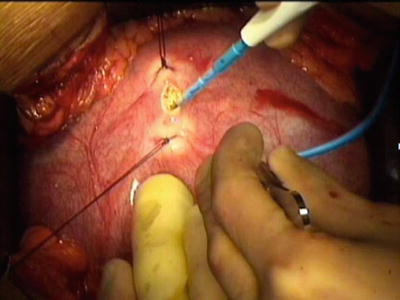
Uterine Exposure
A wide transverse laparotomy halfway between the symphysis pubis and umbilicus is the standard incision for all EXIT procedures because it provides excellent access to the anterior uterine wall, has a low dehiscence rate, and is cosmetically better than a midline laparotomy. Flaps of skin and subcutaneous tissue are raised superiorly and inferiorly. The fascia is divided in the midline from the symphysis pubis to the umbilicus. A Turner-Warwick retractor is placed, and a peritoneal bladder flap is raised. Once the uterus is exposed, intraoperative sterile ultrasonography is used to map the position and edges of the placenta as well as to evaluate the amniotic fluid index. A low-anterior-uterine-segment hysterotomy is the preferred approach for all EXIT procedures. The exceptions are those cases in which the placenta is located in the anterior lower uterine segment. In those cases, a midline laparotomy is performed and the uterine fundus is exteriorized from the abdomen to perform a fundal or posterior hysterotomy. After the placenta is carefully mapped by ultrasound and marked on the uterine surface, a site is chosen ideally at least 6 cm away from the marked edge. This can be complicated in the setting of polyhydramnios when the placental edge can be difficult to identify. Two monofilament stay sutures (0-PDS; Ethicon, Somerville, NJ) are placed through the uterine wall under ultrasound guidance, and the myometrium and membranes are incised with monopolar cautery (Fig. 5). The hysterotomy is completed in a bloodless manner with a uterine stapling device (Premium Poly CS 57; Covidien Auto suture, Mansfield, MA) (Fig. 6). It is important to carefully inspect the uterine edges and make sure that hemostasis is achieved before manipulating the fetus. After hysterotomy, the uterine cavity is filled continuously with warm (37 °C) lactated Ringer solution using a high-flow fluid warmer/pump (Level I-H1200; Smiths Medical, St. Paul, MN) to maintain adequate uterine volume and prevent compression of the umbilical cord. The tone of the uterine wall must be monitored continuously by palpation, and the inhalational anesthesia adjusted accordingly. After the closure of the hysterotomy and the laparotomy, epidural anesthesia (bupivacaine 0.2 %, 5–10 mL) and opioids (morphine, 4–8 mg) are started, and muscle relaxation is reversed (2.5–5 mg of neostigmine plus 0.4–0.6 mg of glycopyrrolate).