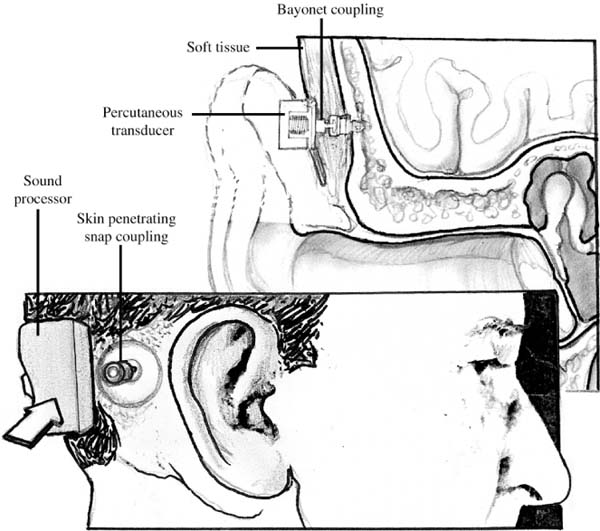
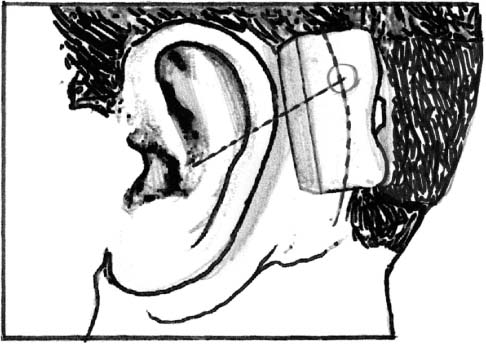
Chapter 29 Implantable hearing aids, compared to conventional hearing aids, are a spectrum of prosthetic device that is wholly or partially implanted through surgery to ameliorate hearing loss.1 To extrapolate this definition, one may consider cochlear implant and brainstem implant as close relatives, if not actual types, of implantable hearing aids. On the other end of the spectrum, a bone-anchored hearing aid (BAHA), essentially a temporal bone stimulator, also qualifies as an implantable hearing aid. Its implantation is less invasive and its method of cochlear stimulation is similar to that of conventional bone conduction hearing aid. Recent technologic advances and innovation in digital microcircuitry have promoted the design of new implantable hearing aids. An ideal implantable hearing aid provides better sound reception and better cosmesis; is nonirritating, biocompatible, and trouble free; and has a long life expectancy. The implanted component should be easily removed or changed without incident. It should not reduce residual hearing, or limit activities such as swimming, or predispose the patient to recurrent infection. The surgical procedure should be simple and free of major complications. Finally, the cost of the device should be similar to a conventional high-power, ear-level aid.1 Over the past decade a number of implantable hearing devices have been introduced, but some have since been discontinued from the competitive market. With the rapid evolution of hearing aid technology, newer implantable hearing aids will soon emerge. This chapter provides a summary of implantable hearing aids: BAHA, middle ear implants, and brainstem implants. Chapter 28 discusses cochlear implantation. In the quest for complete hearing restoration, the cornerstone remains amplification. Many advances have been made in middle ear and chronic otomastoiditis surgery. Despite these advances, there will always remain those patients who despite aggressive surgical interventions continue to drain or begin draining once the canal is occluded with a conventional air-conduction hearing aid. Likewise, there will continue to be congenital aural atresia in which reconstructive endeavors should not or will not be undertaken by the patient or by the wishes of the family. For these patients few options exist. Historically bone-conduction transducers are the aid of choice. Prior to 20 years ago, standard bone-conduction aids transmitted sound waves to the cochlea through the overlying soft tissues and bone. The sound quality was generally thought to be poor and the transmission inefficient. Much of the sound energy could be lost at the level of the soft tissue. The magnitude of attenuation could be as high as 15 to 20 dB in the speech frequencies. To counteract the attenuation of sound energy, the old bone conductors were driven hard, also raising the level of distortion. BAHA (Entific Medical Systems, Goteborg, Sweden) allows a direct coupling between the transducer and the skull, bypassing the soft tissues (Fig. 29–1). Energy transmission is more efficient and sound quality improved. Another advantage is the lack of discomfort from the pre-viously required pressure of the transducers to the soft tissues by the headbands, metal springs, or heavy frames. It should not be disputed that this is the simplest hearing aid implant with respect to both functional concept and implantation.2 FIGURE 29–1 Schematic drawing of the bone-anchored hearing aid (BAHA) in bone. A surgically implanted titanium screw is allowed to osseointegrate into the skull to reduce extrusion and to improve acoustic transmission. The timing of applying a load to the screw after surgery ranges from 1 to 3 months to allow for osseointegration and to reduce irritation of the surrounding soft tissues in the operated field. The BAHA vibrates the screw and skull, which in turn vibrates the cochlear fluids directly. Patient selection involves two main groups of patients: patients with chronically draining ears and a conductive, sensorineural, or mixed hearing loss; and patients with bilateral ear canal atresia whose reconstruction is not advisable, such as those with a Jahrsdoefer rating of 7 or less,3 or in pediatric patients whose reconstructive surgery will be delayed until adulthood so that they can then contemplate the risks of facial nerve injury and hearing loss themselves.4 Acceptable hearing loss for BAHA depends on the use of the ear-level transducer such as the BAHA HC 300 Classic or the body aid transducer BAHA Cordelle, which is more powerful and allows for greater hearing loss. Patients with better cochlear function, such as discrimination scores better than 60% and bone conduction less than 45 dB, have better outcomes with the HC 300 Classic style. Many patients demonstrate a mixed loss. Those with a mean bone conduction loss of 45 dB and an air bone gap of 60 dB (with a total of 105 dB speech threshold) through the speech ranges may consider the Cordelle. Those with a mean bone conduction loss of 60 dB and a maximal air bone gap of 60 dB (with a total of 120 dB speech threshold) are more likely to require the Cordelle.4–7 Preoperative evaluation is limited to audiometric testing and imaging studies. A high-resolution computed tomography (CT) imaging study of the temporal bone is performed in anyone whose sigmoid sinus, middle fossa plate, or facial nerve position is in question as in congenital ear cases. Informed consent should include local infection, subcutaneous tissue reduction in the area, alopecia in the operative site, bleeding from violated sigmoid sinus, and possible dural disruption if a shallow bone plate or low-lying middle fossa is present. In addition reasonable hygiene is expected because the implant penetrates the skin. The surgical steps are relatively simple and are easily learned. Most adults can have this performed under local anesthesia, whereas children usually have a general anesthetic for practical purposes only. The proposed site is marked 55 mm posterior to the external meatus and superiorly in the linea temporalis. The transducer should not contact the pinna when attached to the screw (Fig. 29–2). The following are the operative procedures4: FIGURE 29–2 Site for BAHA placement. 1. A 30-mm radius shave and sterile prep and drape. 2. A 20-mm anteriorly based U-shaped incision is carried down through skin and soft tissues and the flap is reflected forward. 3. The flap is thinned of subcutaneous tissue and sometimes hair follicles. 4. The underlying bone is cleaned of muscle and periosteum in a 6-mm radius in the proposed drilling site. 5. A low-speed (1500 to 2000 rpm) drill, saline irrigation, and a 3-mm drill guide is chosen to allow a 1.8-mm diameter bit. 6. A countersink hole is created with a 4-mm drill guide always remaining at the same initial perpendicular angle of entry to the bone surface. 7. A 3- to 4-mm titanium tap is loaded onto the stainless steel drill hand piece with touching of gloves and will be tapped at an ultralow drill speed of 8 to 15 rpm and at a torque setting of 20 to 40 N×/cm depending on bone softness. 8. The tap is removed by slowly reversing the drill. 9. The fixture flange is implanted by screwing the internal screw and holding the fixture mound with the organizer. 10. A skin punch is utilized directly over the area of the fixture device. 11. If fixture device is stable, the skin abutment is connected immediately. If it is unstable, the connection is delayed 3 to 4 months to allow for osseous integration. 12. The skin flap edges are approximated with 6-0 nylon monofilament. 13. A healing cap is affixed to the abutment cap; gauze and a light mastoid dressing are utilized. Mastoid dressing is removed on the following day. 14. Gauze and cap are maintained until suture removal in one week. 15. Gauze and cap are reapplied for another week. Postoperative complications include local skin reactions treated with topical antibiotic ointments and good hygiene, granulation tissue formation, and loose screws that can usually be tightened without anesthesia with the screwdriver and wrench supplied. Granulation tissue is removed by standard techniques, and the device is not used until the wound is well healed. Overall, the BAHA has specific indications; the technique for implantation is easily learned and the minor complications easily dealt with, making this a worthwhile device that is likely to stand the test of time.
SURGICAL IMPLANTABLE HEARING AIDS
BONE-ANCHORED HEARING AID
MIDDLE EAR IMPLANTS
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree