and Yi Ning J. Strube2
(1)
Wright Foundation for Pediatric Ophthalmology and Adult Strabismus Medical Center, Los Angeles, CA, USA
(2)
Queen’s University, Kingston, Ontario, Canada
Keywords
Medial rectusLateral rectusSuperior rectusInferior rectusSuperior obliqueInferior obliqueSpiral of TillauxFat adherenceAnterior segment ischemiaAn intimate knowledge of anatomy, including the extraocular muscles, periocular fascia, and orbit, is necessary to be an accomplished strabismus surgeon. This chapter reviews anatomical relations relevant to strabismus surgery.
9.1 Muscle Measurements
The basic anatomic features of the extraocular muscles are summarized in Table 9.1. The four rectus muscles are essentially the same length (40 mm), although the amount of tendon varies, with the medial rectus having the shortest tendon length (4 mm), and the lateral rectus having the longest tendon length (8 mm). Of all of the extraocular muscles, the superior oblique has the shortest muscle length (32 mm) and the longest tendon length (26 mm), whereas the inferior oblique has only a 1 mm tendon. The distances in millimeters in Table 9.1 and Fig. 9.1 are for adults.
Table 9.1
Extraocular muscles
Muscle | Approximate muscle length, mm | Origin | Anatomic insertion | Tendon length, mm | Arc of contact, mm | Action from primary position |
|---|---|---|---|---|---|---|
Medial rectus | 40 | Annulus of Zinn | 5.5 mm | 4 | 6 | Adduction |
Lateral rectus | 40 | Annulus of Zinn | 7.0 mm | 8 | 10 | Abduction |
Superior rectus | 40 | Annulus of Zinn | 8.0 mm | 6 | 6.5 | Elevation |
Intorsion | ||||||
Adduction | ||||||
Inferior rectus | 40 | Annulus of Zinn | 6.5 mm | 7 | 7 | Depression |
Extorsion | ||||||
Adduction | ||||||
Superior oblique | 32 | Orbit apex above annulus of Zinn | From temporal pole of superior rectus to within 6.5 mm of optic nerve | 26 | 12 | Intorsion |
Depression | ||||||
Abduction | ||||||
Inferior oblique | 37 | Lacrimal fossa | Macular area | 1 | 15 | Extorsion |
Elevation | ||||||
Abduction |
Fig. 9.1
The rectus muscle insertions are horseshoe-shaped, with the horse walking toward the limbus. The progressive increase of insertion distance from the limbus, with the medial rectus being the closest and the superior rectus being the farthest, is called the spiral of Tillaux. The surgeon should heed the posterior extension of the horseshoe insertion when passing a hook behind the muscle. The approximate tendon width, at the insertion, of each rectus muscle is 10 mm, and the average distance between rectus muscle insertions is 6–8 mm. Thus, even a half-tendon width transposition of any rectus muscle places it within a few millimeters of the adjacent rectus insertion. Because of the proximity of the muscles, it is possible to inadvertently hook the wrong rectus muscle during strabismus surgery
9.2 Conjunctiva
It is often said that the conjunctiva is forgiving to the surgeon, but beware because poorly placed incisions can lead to functional and cosmetic problems. The plica, lateral canthus, and extraconal fat pad are important structures to avoid. Conjunctival incisions that extend into the plica are painful, cause unsightly scarring, and may cause a restrictive strabismus. Incisions that extend from the bulbar conjunctiva to the lateral canthus may cause symblepharon and restriction. In the inferior fornix, the extraconal fat pad starts approximately 10 mm posterior to the limbus and can be identified as a soft bulge deep in the fornix. Fornix incisions should be placed anterior to this fat pad to avoid fat adherence and bleeding.
9.3 Subconjunctival Fascia
9.3.1 Muscle Pulley System: Muscle Sleeve
The extraocular muscles are held in place within the orbit by an intricate fascial network. This fascial network suspends the muscles as they approach the eye, and was termed “muscle sleeve” by the late Dr. Parks. The new term, popularized by Dr. Demer et al. [1], is “muscle pulley” system. In the anterior orbit, the pulley system holds the rectus muscles close to the orbital wall until the muscle exits the pulley to attach to the eyeball. Ectopic pulley location has been implicated as a cause of some types of incomitant strabismus [2]. Ectopic muscles have been a well-documented cause of incomitant strabismus in patients with craniofacial synostosis. In these patients, extorsion of the orbits is responsible for displacing the muscles [3]. The medial rectus muscles are displaced up and the lateral rectus muscles down, causing apparent inferior oblique overaction. The superior rectus muscles are displaced laterally and inferior rectus muscles nasally, producing a V pattern. These cases aside, ectopic pulleys, as a rule, are not a common cause of incomitant strabismus.
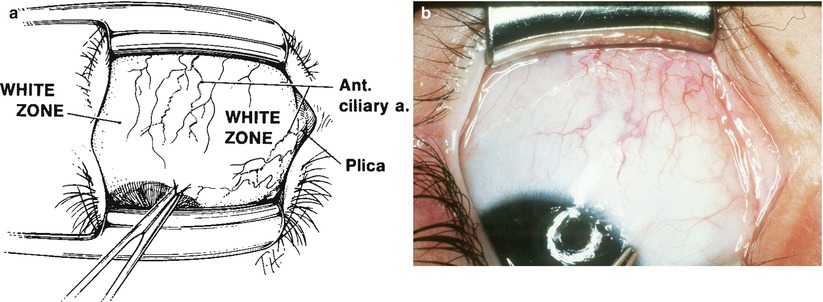
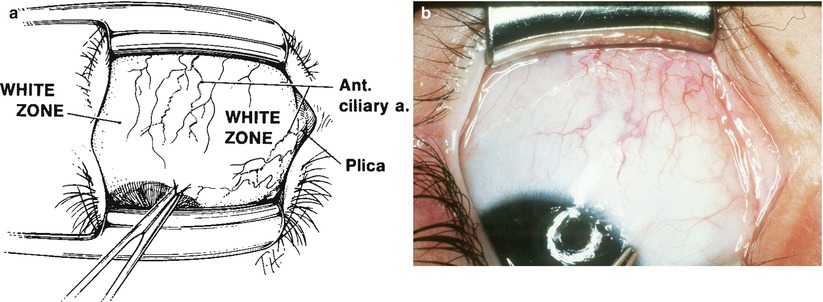
Fig. 9.2




The drawing (a) and companion photograph (b) show the left inferior rectus muscle insertion and its anterior ciliary arteries as seen through the intact conjunctiva (surgeon’s view). The rectus muscle insertions usually can be located before surgery by identifying their ciliary arteries, which are associated with a band of pink tissue. Anterior ciliary arteries lie deep below the conjunctival vessels and do not move if the conjunctiva is manipulated. Preoperative identification of rectus muscle insertions and the white zone between the muscles is important, as these landmarks guide the placement of the conjunctival incision and reduce the possibility of inadvertently hooking the wrong muscle. The white zone is the clear area between the rectus muscles. Sometimes it is difficult to positively identify the anterior ciliary arteries and the rectus muscles. The white zone, on the other hand, is a consistent landmark and can be identified in virtually all patients
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


