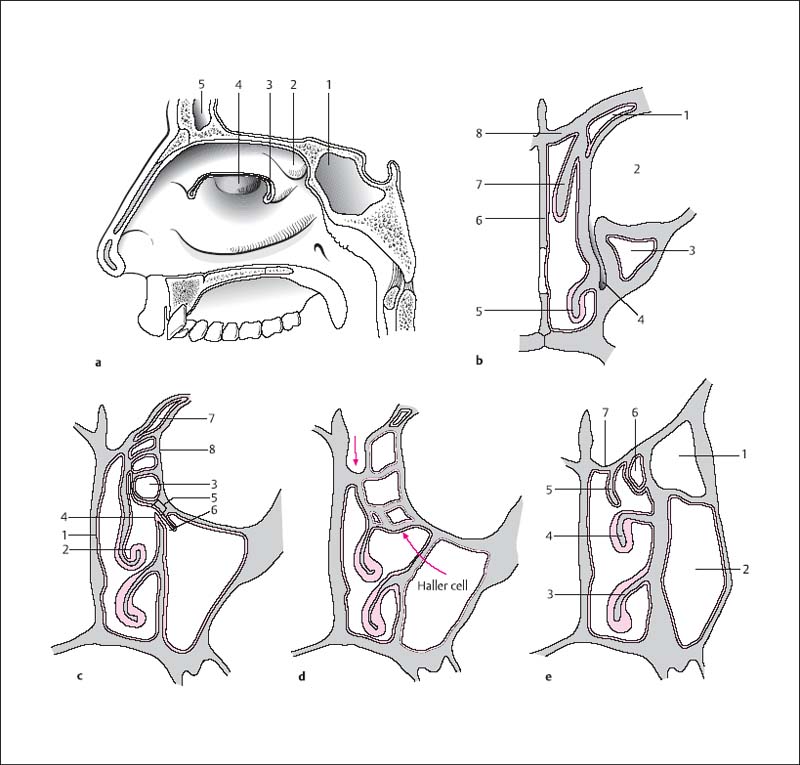
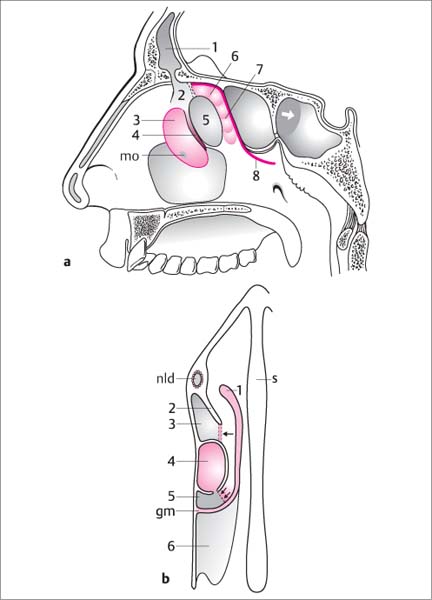
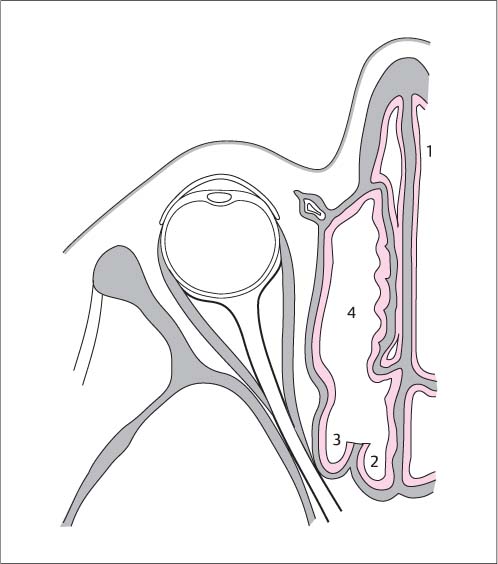
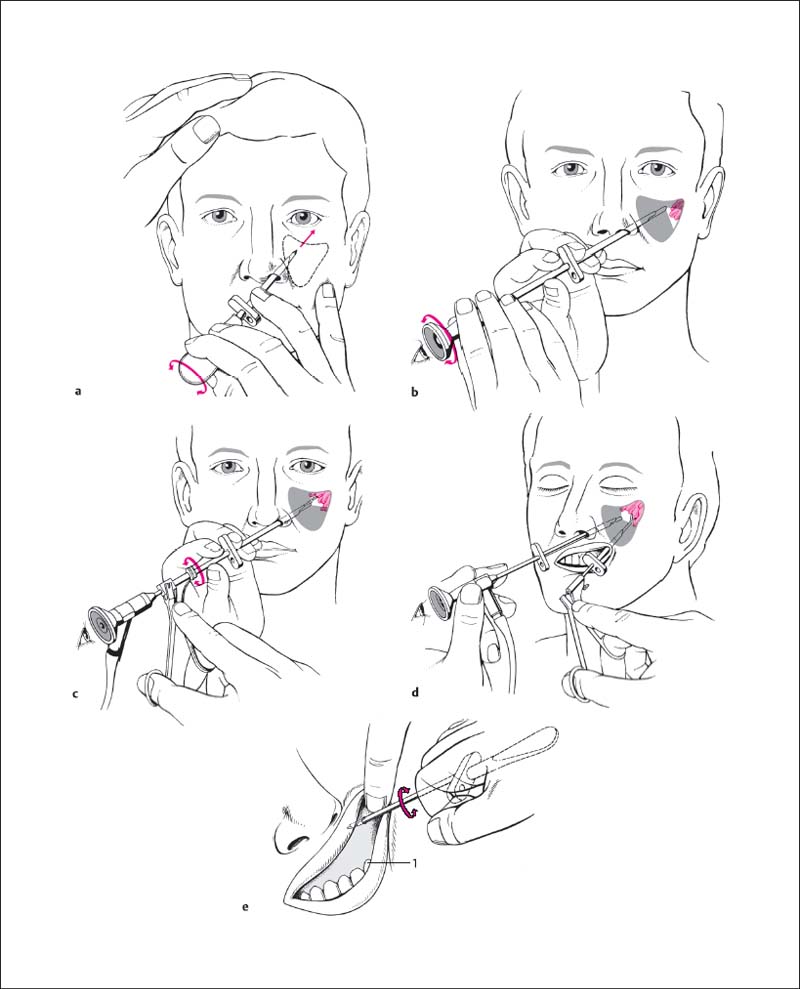
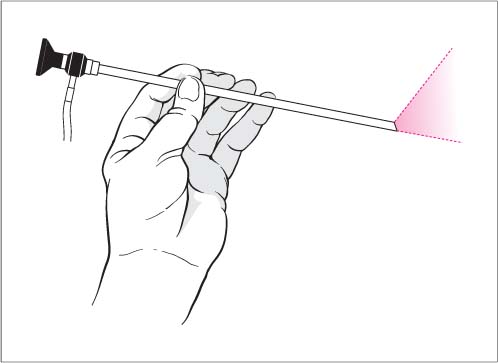
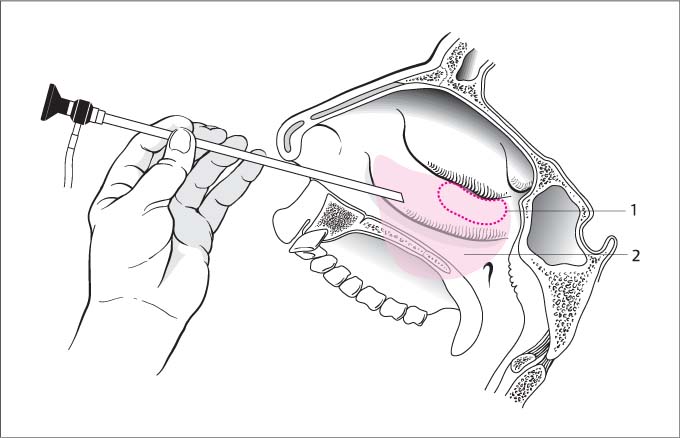
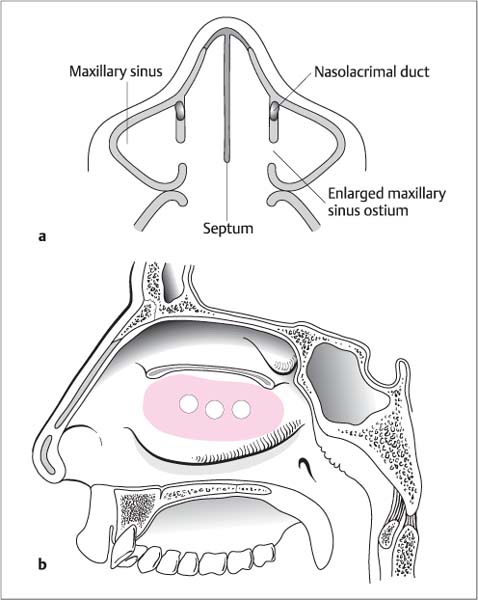
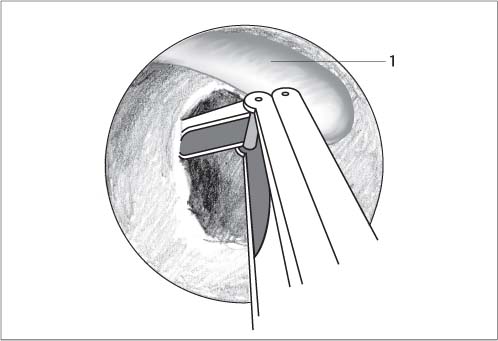
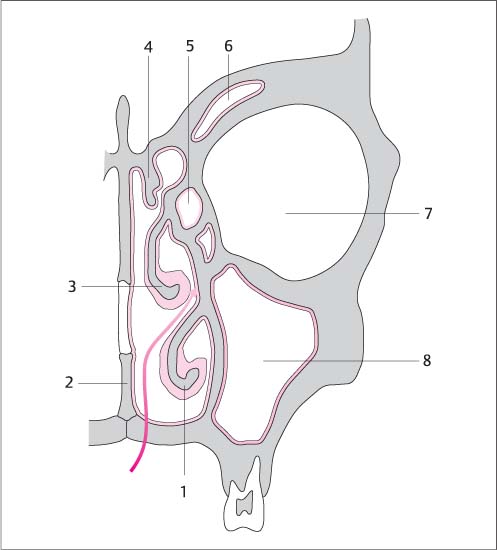
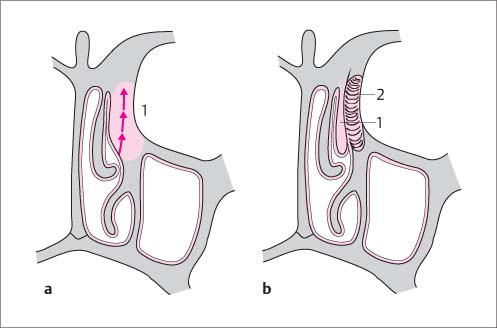
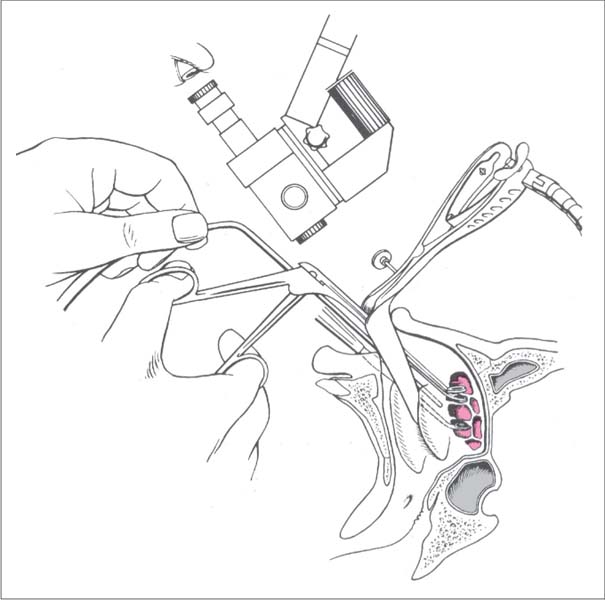
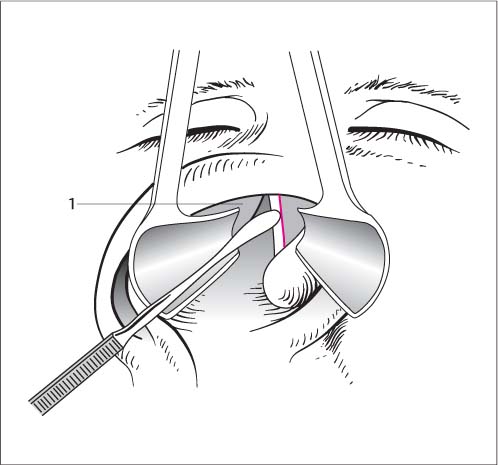
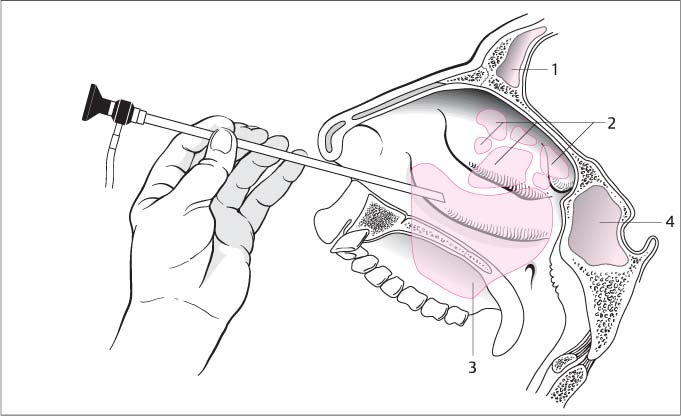
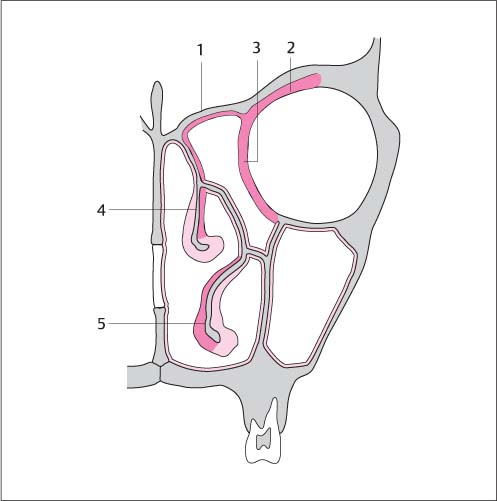
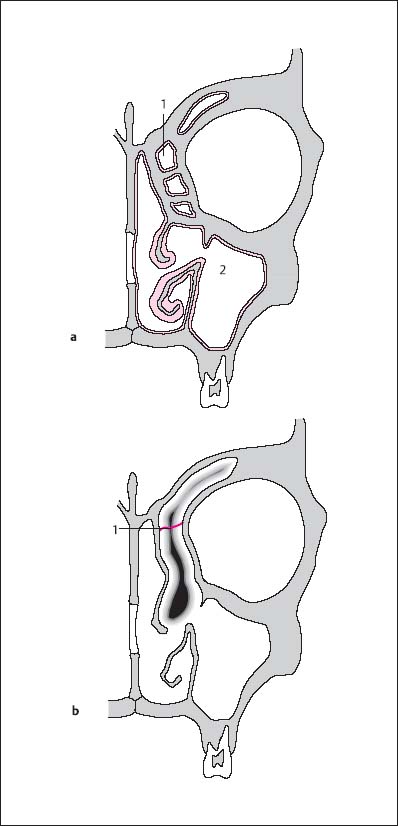
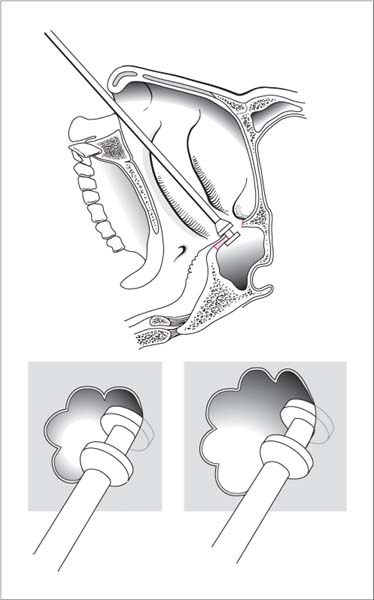
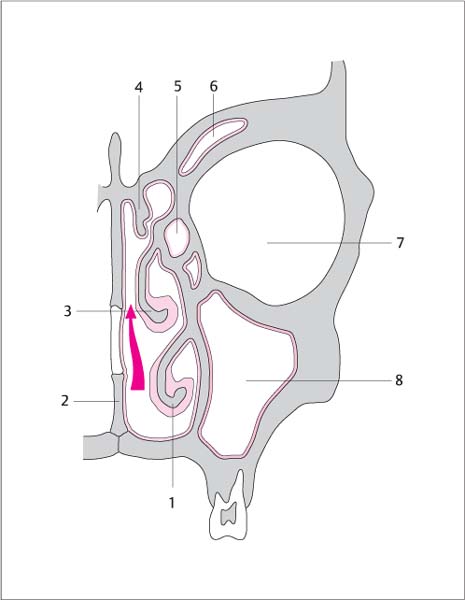
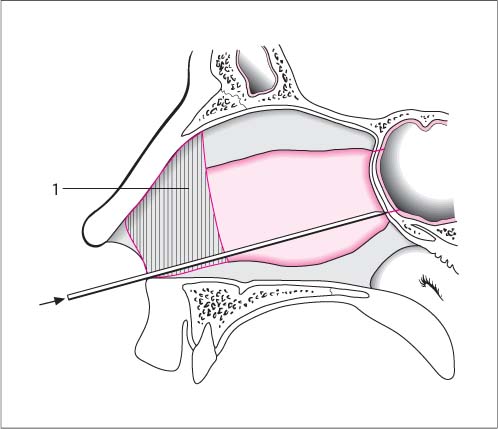
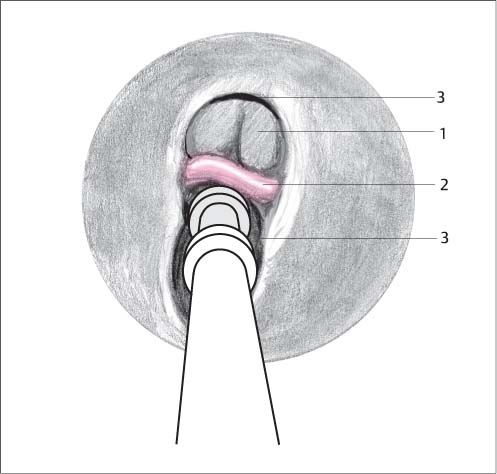
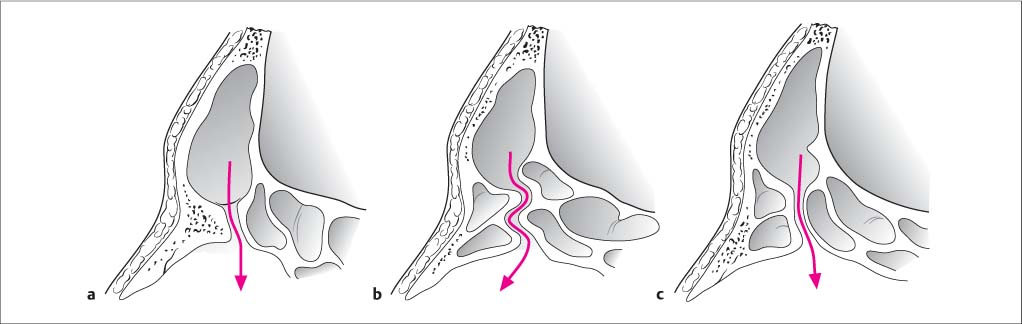
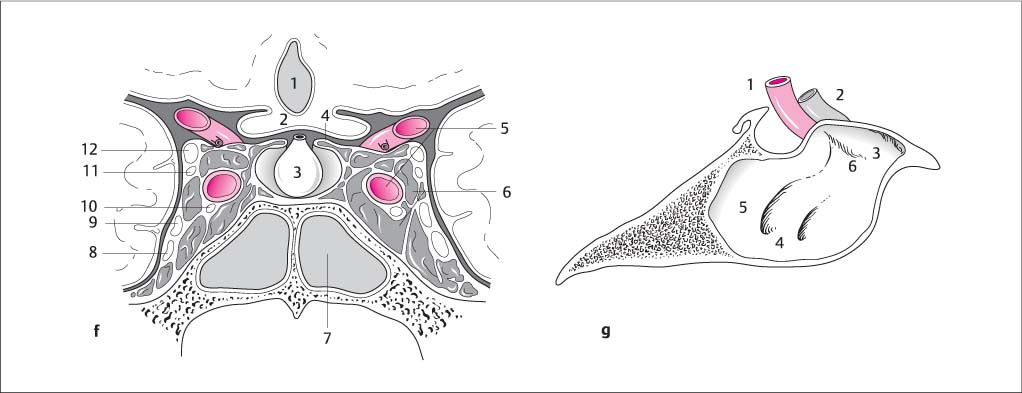
7 Surgery of the Paranasal Sinuses and Their Adjacent Structures Today, endonasal surgery of the paranasal sinuses involves the use of optic systems—endoscopes and/or microscopes—and so allows the use of operative techniques that incorporate functional aspects of mucosal physiology and related anatomical structures. These procedures can therefore also be classified as functional operations. A distinction is made between endoscopic surgery of the paranasal sinuses, also referred to as functional endoscopic sinus surgery (FESS), and a combined microscopic and endoscopic technique. FESS comprises the circumscribed opening of the paranasal sinus system and the removal of its contents, as determined by the presenting pathology. Unlike earlier surgical procedures, this technique is minimally invasive: for example, the radical removal of mucous membranes from the paranasal sinus is avoided. The four paranasal sinuses—the maxillary sinus, ethmoid sinus (ethmoidal labyrinth), frontal sinus, and sphenoid sinus—rep-resent paired lateral outgrowths from the main nasal cavities. The medial border of the main nasal cavity is the septum, while the lateral nasal wall bears the nasal turbinates (Fig. 7.1a). The three turbinates divide the lateral nasal wall into three distinct airspaces: the superior, middle, and inferior meatus. The paired ethmoid sinuses contain 10–15 air cells, which are lined with respiratory epithelium. Medially, the ethmoid is bordered by the middle turbinate. Superiorly it closes off the frontal bone, which is also referred to as the anterior roof of the ethmoid (Fig. 7.1b). The entire roof of the ethmoid extends from the planum sphenoidale to the frontal bone and can have various anatomic configurations, knowledge of which is of great importance for surgery of the sphenoid. Embedded in the cribriform plate of the ethmoid is the crista galli, a crest like elevation which extends into the anterior cranial fossa (Fig. 7.1c). The lateral border of the ethmoid sinus is formed by the lamina papyracea (Fig. 7.1c), a thin, bony structure separating the orbit from the paranasal sinuses. The lamina cribrosa fits into the ethmoid notch. The olfactory nerves pass through the lamina cribrosa from the olfactory region into the olfactory bulb. Basically, various types of ethmoid roof configurations are described, which develop according to the length of the lateral lamella of the lamina cribrosa. The longer the lateral lamella, the deeper is the olfactory groove (= “risky ethmoid”). This means that there is an increased risk of injury to the bone of the skull base as compared with a flat ethmoid roof (Fig. 7.1d). The basal lamella of the middle turbinate divides the ethmoid complex anatomically into an anterior and a posterior ethmoid cell (Fig. 7.2a). The course of the basal lamella can be described in three parts as it extends between its endpoints (the ethmoid crest of the maxilla and the ethmoid crest of the perpendicular process of the palatine bone): Anterior ethmoidal complex. The ostium of the maxillary sinus drains into a narrow funnel-shaped space, the maxillary infundibulum (Fig. 7.1c), which runs in a sagittal direction in the lateral nasal wall. Cranially the maxillary infundibulum drains into the ethmoid infundibulum (anterior ethmoid), which continues medially and dorsally into the hiatus semilunaris. The inferior hiatus semilunaris is a two-dimensional gap, which, when opened from a medial dorsal access, leads into the ethmoid infundibulum (Fig. 7.2a, b). Further anteriorly, the medial wall of the infundibulum is formed by the uncinate process (a sickle-shaped process, which corresponds to the rudiment of the first lamella in the middle meatus). Its anterior margin attaches to the lacrimal bone and the orbital surface (facies orbitalis) of the maxilla. Small processes extend out to the roof of the maxilla, with further connections fusing with processes of the palatine bone and the turbinate bone. This bony labyrinth is covered medially by nasal mucosa and laterally by mucosa of the maxillary sinus. The ethmoid infundibulum can merge without interruption with the frontal recess in a ventral and cranial direction, depending on how the uncinate process bends and attaches to the lamina papyracea. This makes it difficult to distinguish the ethmoid infundibulum from the frontal recess. The natural maxillary ostium is located at the junction between the middle and dorsal third of the ethmoid infundibulum, which is why it is often hidden in the middle meatus. Fig. 7.1a–g Anatomical relationships of the paranasal sinuses. a Lateral nasal wall. 1 right sphenoid sinus 2 superior turbinate 3 middle turbinate 4 inferior turbinate 5 right frontal sinus b Coronary section through the nasolacrimal duct. 1 frontal sinus 2 orbit 3 maxillary sinus 4 nasolacrimal duct 5 inferior turbinate 6 septum 7 middle turbinate 8 ethmoid roof c Coronary section through the maxillary sinus ostium. 1 middle turbinate 2 turbinate sinus 3 ethmoid bulla 4 uncinate process and medial infundibular wall 5 ethmoid infundibulum 6 maxillary sinus ostium 7 frontal recess 8 lamina papyracea (lamina orbitalis) d Low-lying lamina cribrosa and Haller cell. e Coronary section through the posterior ethmoid sinuses. 1 orbit 2 maxillary sinus 3 inferior turbinate 4 middle turbinate 5 superior turbinate 6 posterior ethmoid cell 7 lamina cribrosa f Coronary section through the sphenoid sinus. 1 third ventricle 2 optic chiasma 3 pituitary 4 sellar diaphragm 5 internal carotid artery 6 cavernous sinus 7 sphenoid sinus 8 maxillary nerve 9 ophthalmic nerve (first branch of the trigeminal nerve, CN V) 10 abducens nerve (CN VI) 11 trochlear nerve (CN IV) 12 oculomotor nerve (CN III) g Lateral view of the sphenoid sinus. 1 internal carotid artery 2 optic nerve 3 prominence of the optic nerve 4 prominence of the maxillary nerve 5 prominence of the internal carotid artery 6 infraoptic recess The second lamella in the anterior ethmoidal complex is formed by the ethmoid bulla (Fig. 7.1a), which extends as far as the lamina papyracea and finally continues onto the medial roof of the maxillary sinus as the frontal crest. An anterior ethmoid cell, known as the agger nasi cell or cellula lacrimalis, often takes its origin from the superior aspect of the ethmoid infundibulum or the frontal recess, descends into the agger nasi, and abuts on the lacrimal fossa. Sometimes one or two cells drain into the lateral infundibular wall, just under the ethmoid bulla, and extend into the medial orbital floor; these are known as Haller cells (Fig. 7.1d). Clefts in the anterior ethmoid complex, which are situated above and behind the ethmoid bulla, are referred to as suprabullar and retrobullar recesses and are synonymous with a lateral sinus (Fig. 7.2a, b). The frontal infundibulum is a funnel-shaped protrusion from the floor of the frontal sinus, caudally toward the natural frontal sinus ostium. From an anatomical view, the frontal infundibulum lies within the frontal sinus itself. The frontal recess is located caudal to the frontal infundibulum and to the natural frontal sinus ostium (Fig. 7.2a, b). It is shaped like a reversed funnel and forms the most anterior part of the anterior ethmoid sinus. It can be considerably narrowed by anatomic variations of the uncinate process, the ethmoid bulla, and the agger nasi cells. A knowledge of the anatomy and the course of these variations facilitates the search for the natural ostium of the frontal sinus during surgery. The caudal part of the middle turbinate may be significantly curled downward laterally, especially in the middle part, or it may even appear as an almost horizontally and laterally bent crest. Its concave lateral surface forms the turbinate sinus. Cavities are frequently found in the middle turbinate; the best known of these is a cell in the anterior part known as the concha bullosa. Posterior ethmoidal complex. The posterior middle meatus is formed medially by the first posterior ethmoid cell and by the superior meatus, which often indents into the middle turbinate. The posterior ethmoidal complex therefore projects medially slightly beyond the anterior ethmoid (Fig. 7.1e). Cranially the optic nerve lies against the lateral wall of the sphenoid sinus (Fig. 7.1g, h) and below it is found the anterior genu of the internal carotid artery. Onodi cells are posterior suprasphenoidal ethmoid cells, which can displace the location of the sphenoid cavity far laterally (Fig. 7.3). The optic nerve and the internal carotid artery then also run in the lateral wall of these cells. It should be borne in mind that in ca. 4 % of cases the bony cover of the optic nerve, and in ca. 8 % of cases of that of the internal carotid artery, is dehiscent. Fig. 7.2a, b Longitudinal and horizontal sections through the lateral nasal wall and the paranasal sinus system (modified after A. Hambrosch, Graz University, Austria). a Highly schematized presentation of a paramedian longitudinal section through the lateral nasal wall and the paranasal sinus system. The red area shows the insertion line of the middle turbinate to the lateral nasal wall and skull base. For reasons of perspective, the anterior fifth of this insertion is not shown. 1 frontal sinus 2 frontal recess 3 uncinate process 4 hiatus semilunaris (inferior) 5 ethmoid bulla 6 suprabullar recess 7 retrobullar recess 8 insertion line of the middle turbinate (basal lamella), which separates the anterior ethmoid cells from the posterior ethmoid cells. mo maxillary sinus ostium b Schematic presentation of a horizontal section through the lateral nasal wall just above the horizontal course of the dorsal third of the middle turbinate. s septum nld nasolacrimal duct gm frontal part of the basal lamella of the middle turbinate, which separates the anterior ethmoid cells from the posterior ethmoid cells. 1 cut edge: vertical part of the middle turbinate 2 uncinate process 3 ethmoid infundibulum 4 ethmoid bulla 5 retrobullar recess 6 posterior ethmoid cell → hiatus semilunaris (inferior) → → hiatus semilunaris (superior) Fig. 7.3 Sphenoethmoid cell: Onodi cell. 1 septum 2 sphenoid sinus 3 Onodi cell 4 cleared ethmoid cells Tapered sponge or ribbon gauze soaked in lidocaine and epinephrine (1:1 000) for approximately 10 minutes (ratio 5:1 lidocaine to epinephrine 1:1 000). Inject 1 % lidocaine and epinephrine 1: 200 000 beneath the mucosa of the uncinate process and agger nasi. Additional infiltration of the insertion of the middle turbinate. Peripheral block of the ethmoid nerves if required: depot injection of 2 mL at a depth of 1–2 cm. Transnasal puncture of the maxillary sinus with a trocar via the lower meatus, or transoral puncture through the canine fossa. This allows exploration of the entire maxillary sinus using fine rigid scopes with various viewing angles. Tissue biopsies may be taken using instruments introduced either through the sleeve or using a combined transnasal and transoral approach. As a rule, the transnasal route should be adopted in children to avoid damage to the unerupted teeth. Local anesthesia. Transnasal decongestion of the nose. Lidocaine spray to the middle turbinate and in the lower meatus. A ribbon gauze soaked in local anesthetic is placed in the lower meatus. Enough time (ca. 5 minutes) should be allowed for the onset of action. An additional depot of 1 mL 1 % lidocaine may be administered to the nasal floor for a vasoconstrictive effect. Depot injection of 1 % lidocaine with the addition of a vasoconstrictor transorally into the canine fossa. Positioning is semi-supine or supine. Square-end trocar for children and adults. Sinoscopes with 0°, 25°, 30°, 70°, and 120° viewing angles, biopsy grasping forceps if required, flexible forceps, small scissors, and pediatric scopes. Transnasal approach (Fig. 7.4a–d). The head of the inferior turbinate is visualized and displaced with the speculum. The trocar is inserted into the inferior meatus to its highest point, roughly in the middle. Careful pressure is exerted in the direction of the lateral canthus until the bony lamella is perforated. The heel of the operating hand is supported on the patient’s cheek, while the other hand applies counter-support to the patient’s head. Transoral approach (Fig. 7.4e). The lip is raised laterally over the canine tooth. The upper border of the canine fossa is identified by palpation with the left index finger (ca. 1 cm below the infraorbital nerve). Here the trocar pierces the mucous membrane and is drilled into the facial maxillary wall using rotary movements in a strictly sagittal direction. The heel of the hand is simultaneously supported on the cheek. The trocar sleeve is then advanced a little further with twisting movements. Then as in the transnasal approach. The patient should avoid nose-blowing with occlusion of both nostrils for 2–3 days and press the hand against the cheek during any inadvertent sneezing. Endonasal enlargement of the maxillary ostium to the middle meatus for aeration and improvement of drainage. Nasal endoscopy, conventional radiography of the paranasal sinuses, CT if appropriate. Local anesthesia or general endotracheal anesthesia. Endoscopes (0°, 30°, 45°, 70°) (Fig. 7.5), microscope (250- or 300-mm lens), ethmoid or Blakesley forceps, forward- and backward-oblique bone punches, Freer elevator, and microdisk knife. Positioning. The head is not reclined and the upper body of the patient is slightly elevated. The surgeon sits or stands on the right of the patient. Fig. 7.4a–e Transnasal and transoral sinuscopy. a Perforation of the lateral nasal wall using short counter-rotating movements. The hand is supported on the cheek. b Inspection of the maxillary sinus after turning the optical trocar. c Polypectomy in the maxillary sinus using rigid optical forceps. d Biopsy of the maxillary sinus using a combined approach. Optical trocar nasal; forceps transoral. e Transoral sinuscopy. Sagittal approach in the lateral canine fossa and above the canine tooth (1). Fig. 7.5 Holding the endoscope. The middle turbinate is displaced medially under endoscopic vision without fracturing it. The posterior fontanelle region of the maxillary sinus is identified dorsally, just above the dorsal end of the uncinate process (Figs. 7.6 and 7.7b). The fontanelle is covered medially by nasal mucosa and laterally by the mucosa of the maxillary sinus, and as such is a bone-free region of the lateral nasal wall. The two mucous membranes are connected by fibrous tissue. Accessory ostia also drain into the maxillary sinus via the fontanelle and may also be used to enlarge the maxillary ostium (Fig. 7.7a, b). After gently penetrating the fontanelle with an angled suction probe or an angled Blakeley forceps, the lumen of the maxillary sinus becomes visible, allowing it to be enlarged with an appropriate punch (backward-oblique bone punch, Fig. 7.8) superiorly, anteriorly, and inferiorly. By using various scopes (30°, 70°), all areas of the lumen of the maxillary sinus can now be assessed and the pathological lesion removed with appropriate forceps. The hiatus semilunaris is left untouched when enlarging the maxillary ostium. If an accessory maxillary ostium is present, the enlargement should be accomplished via the accessory ostium. The creation of a second enlarged ostium should be avoided, otherwise recirculation of mucus via both ostia will occur. A loose nasal pack is inserted at the end of the operation. The patient is positioned supine on the operating table. After displacement of the middle turbinate (without fracturing it), the medial wall of the maxillary sinus is gently penetrated between the back end of the lower turbinate over the region of the fontanelle with a curved suction probe or an angled Blakesley forceps. The further procedure is identical to that of the endoscopic operation. The contents of the ethmoid sinus are removed using an endonasal approach after dislocating the middle turbinate in a medial direction. An infundibulotomy (partial ethmoidectomy) involves only the anterior parts of the ethmoid. A complete sphenoethmoidectomy (pansinus operation) involves removing all pathological mucosa from the entire ethmoid cell system, including the sphenoid sinus, the maxillary sinus, and the access to the frontal sinus (Fig. 7.9). The optimal preservation of healthy mucous membrane is essential, which is why the use of punching instruments is important. Fig. 7.6 Endoscopic enlargement of the maxillary sinus ostium. 1 location of the enlarged maxillary sinus ostium (shaded red) 2 extent of the maxillary sinus Fig. 7.7a, b Position of the enlarged maxillary sinus ostium. a Position is axial to the nasolacrimal duct. b Position of the fontanelle and the accessory ostia after resection of the vertical part of the middle turbinate. Endonasal enlargement of the ethmoid infundibulum by removing the uncinate process, and if necessary opening the ethmoid bulla to aerate and drain the downstream paranasal sinuses. Maximal protection of affected mucous membranes is essential, especially at anatomical bottlenecks. Fig. 7.8 Widening of a maxillary sinus ostium on the right with a back-biting punch. View through the endoscope. 1 posterior end of the middle turbinate Fig. 7.9 Endonasal approach to the ethmoid cells. 1 inferior nasal turbinate 2 nasal septum 3 middle nasal turbinate 4 superior nasal turbinate 5 ethmoid cells 6 frontal sinus 7 orbit 8 maxillary sinus See Risks and Complications (p. 117). Local anesthesia with a topical anesthetic or general endotracheal anesthesia. Microscope, rigid scopes, ethmoid forceps, bone punches, curette, Freer elevator. After decongestion of the nose, the free edge of the uncinate process is exposed and an incision is made around it. Starting cranially, just below the insertion of the middle turbinate, the incision is extended dorsally to the level of the maxillary sinus ostium (Fig. 7.10a). The medial wall of the infundibulum is then removed. From here, any obstructing processes, such as a medial-leaning uncinate process or infundibular wall, are corrected. If the ethmoid bulla is protruding and thus causing an obstruction (Fig. 7.10b), it is gently penetrated with a blunt ethmoid forceps and its wall removed. Any more far-reaching polyposis is pursued into the ethmoid sinus. The prevailing mucosal appearance and the anatomical situation will determine whether a supraturbinal fenestration of the maxillary sinus is indicated. A pack attached to a thread is then inserted into the middle meatus and left for a day. After decongestion of the nose, the middle turbinate is retracted medially with the speculum. A self-retaining speculum is then inserted (Fig. 7.11). The free edge of the uncinate process is easily identified under the microscope. As with the endoscopic operation, an incision is made around the uncinate process with a Freer elevator (Fig. 7.12) and it is removed with a Blakesley forceps. After removal of the uncinate process, residual parts of the ethmoid infundibulum now lie exposed cranially. Fig. 7.10a, b Schematic presentation of an incision around the uncinate process (a). Direction of the incision (1). The ethmoid bulla becomes visible further dorsally (b). 1 uncinate process displaced to one side 2 ethmoid bulla Fig. 7.11 Endoscopic surgery of the paranasal sinuses using the microscope. Endonasal surgery of the ethmoid. Removal of the contents of the cell system under the microscope using the double-spoon forceps and Volkmann curette. A pack attached to a thread is then inserted into the middle meatus and left for a day. Removal of the contents of the ethmoid cells via an endonasal approach within their anatomical borders: ethmoid roof, medial turbinate, orbital roof, and lamina papyracea (Figs. 7.13 and 7.14). Fig. 7.12 Microscopical incision around the uncinate process using a Freer elevator. 1 middle turbinate retracted medially. The anterior ethmoid is exposed as far as the basal lamella of the middle turbinate, whereas the posterior ethmoid is accessible only after penetrating the basal lamella. Positioning and preparation. As for an endoscopic operation. The patient is positioned supine with the upper part of the body slightly raised (20°). The surgeon sits or stands on the right of the patient, while the scrub nurse is positioned on the left side of the patient. The middle turbinate is identified with a 0° or 25° scope, a crescent-shaped convex incision is made around the uncinate process, which is then removed using rotary movements to avoid tearing the mucosa in a caudal or cranial direction. The ethmoid bulla, which bulges out antero-inferiorly, is opened using a Blakesley forceps and the lumen is displayed (see Infundibulotomy, p. 118). The retrobullar recess and the suprabullar recess may be found dorsal to and above the bulla, respectively. To open the posterior ethmoid sinus, the basal lamella of the middle turbinate is perforated anteriorly, ca. 3–4 mm above the dorsal third of the basal lamella. The individual ethmoid cells, which are bordered by a few bony septa, are then removed with a curved Blakesley forceps or with ethmoid punches. The roof of the ethmoid is then identified, paying due regard to the bony landmarks—the middle turbinate medially and the lamina papyracea laterally (Fig. 7.15a, b). Fig. 7.13 Projection of the paranasal sinuses onto the lateral nasal wall. 1 frontal sinus 2 ethmoid sinus 3 maxillary sinus 4 sphenoid sinus Fig. 7.14 Boundaries of surgery of the ethmoid. 1 ethmoid roof 2 orbital roof 3 lamina papyracea 4 middle nasal turbinate 5 low nasal turbinate Attention should be directed to a possible attenuated lamina papyracea or to ethmoid cells, which extend far dorsally, so-called suprasphenoid Onodi cells. In the presence of Onodi cells, the ethmoid sinus will need to be identified further medially to protect the optic canal. When removing the contents of the ethmoid cells anteriorly, care should be taken to identify the ethmoid arteries, which run transversely across the roof of the ethmoid. After the contents of the ethmoid sinus are removed, the frontal sinus ostium can be identified ventral to the anterior ethmoidal artery, which runs horizontally (see Surgery of the Frontal Sinus, p. 123). A pack is inserted for 1 day. Positioning and preparation. The patient is positioned supine, with the head slightly lowered. The surgeon sits below the head on the contralateral side; depending on the direction of access, the patient’s head will need to be turned toward or away from the surgeon (see Infundibulotomy, p. 118). For work on the anterior ethmoid region it is important that the head is reclined as far as possible. As a rule, it is recommended that surgical landmarks and anatomical borders are identified when performing microscopic surgery of the ethmoid, as well as for endoscopic ethmoid surgery. Fig. 7.15a, b Principle of endonasal ethmoidectomy. a Wide enlargement of the maxillary sinus ostium and opened ethmoid bulla. 1 ethmoid cells 2 enlargement of the maxillary sinus ostium b Ethmoid cells after removal of their contents. 1 anterior ethmoid artery in projection Removal of the anterior wall of the sphenoid sinus converts it into a wide open secondary nasal sinus. Removal of the mucous membranes is undertaken only to the extent that is absolutely necessary, and should also be performed extremely conservatively in the region of the optic nerve. Access to the sphenoid sinus can be endonasal, trans-septal, or transethmoidal. Thin-slice CT or MRI. Mushroom punch (see below) and other punches. General endotracheal anesthesia. Transethmoidal approach. At first the contents of the entire ethmoid sinus are removed. Next, the anterior wall of the sphenoid sinus is identified, further medial and caudal to the ethmoid cells which have already been opened and emptied of their contents. The ethmoid cells are gently perforated with an elevator or grasping forceps. Use of an angled punch or a mushroom punch is recommended for the removal of further parts of the anterior wall (Fig. 7.16). Transnasal approach. Decongestion of the nose. The posterior part of the middle turbinate is retracted laterally under direct endoscopic view (Fig. 7.17). The mucosa is swept off the anterior wall of the sphenoid sinus. The sphenoid sinus ostium is identified. The anterior wall of the sphenoid sinus is gently penetrated with light pressure ca. 1 cm above the turbinate, lateral to the septum. The anterior wall of the sphenoid sinus is then removed piecemeal with a punch. Trans-septal approach. The trans-septal approach to the sphenoid sinus initially requires the temporary removal of the bony nasal septum and resection of the superior part of the vomer. After careful elevation of the mucous membranes off the vomer, the vomerine plate is mobilized by careful movements to and fro with forceps or Blakesley forceps, and removed. The anterior wall of the sphenoid sinus is mobilized with a careful horizontal tap of the chisel ca. 5 mm below the nasal roof, and a further blow ca. 1 cm lower and parallel. The two fracture lines are joined with two cuts placed at right angles to them to remove the bony plate, which is now mobile (Fig. 7.18). The pathological lesion is now removed via this opening in the anterior wall. Fig. 7.16 Schematic illustration of transethmoidal enlargement of the sphenoid sinus ostium (modified after Stammberger). Removal of the anterior wall of the sphenoid sinus with a mushroom punch. A pack is then inserted. Fig. 7.17 Enlargement of the sphenoid sinus ostium; transnasal approach. 1 inferior nasal turbinate 2 nasal septum 3 middle turbinate 4 superior turbinate 5 ethmoid cells 6 left frontal sinus 7 orbit 8 maxillary sinus Transethmoid. Surgery in the region of the frontal recess to identify the frontal sinus ostium is usually performed during a pansinus operation under endoscopic view using curved punches, small forceps, and angled scopes, with as little traumatization as possible. Apart from endoscopic operations, endonasal drainages of the frontal sinus (three types) using Draf’s micro-endoscopic surgical technique are also described. The principle of simple drainage of the frontal sinus (Draf Type 1) involves the identification of the frontal recess, removal of its contents, and identification of the frontal sinus ostium. The Draf Type 2 extended drainage procedure involves the removal of those parts of the frontal sinus that are obstructing the ostium (type 2A), and the removal of the floor of the frontal sinus, from the medial border of the orbit to the nasal septum, anterior to the level of the posterior wall of the frontal sinus (type 2B). Draf Type 3 endonasal median drainage consists of the additional removal of the parts of the septum adjacent to the frontal sinus floor as well as the floor of the contralateral frontal sinus. Fig. 7.18 Trans-septal enlargement of the sphenoid sinus ostium. The cartilaginous septum (1) remains intact. Fig. 7.19 Endonasal enlargement of the frontal sinus ostium. View through the endoscope. 1 frontal sinus ostium 2 anterior ethmoid artery 3 bone to be removed, cranial and posterior Fig. 7.20a–c Variations of development and position of the frontal recess (nasofrontal duct). General endotracheal anesthesia. Diamond burr, endoscope, operating microscope. Endonasal. After removal of the uncinate process and, if appropriate, the ethmoid bulla, the frontal recess, which represents the uppermost front part of the anterior ethmoid sinus, is visualized. After identification of the frontal sinus ostium, which merges cranially into the infundibulum of the frontal sinus, the anterior ethmoid artery can be visualized, marking the limits of dissection. The anterior ethmoid artery usually runs in a bony canal across the roof of the ethmoid and through the ethmoid fovea toward the lamina cribrosa, dorsal to the frontal sinus ostium. The ostium should not be looked for too far medially, to avoid injury to the lamina cribrosa (skull base defect) (Fig. 7.19). Any soft tissue obstructing the frontal sinus ostium should be removed with an angled forceps. Angled circular punches are also suitable for opening and enlarging a frontal sinus ostium obstructed by scarring. Removal of the mucous membrane lining the frontal sinus should be avoided as far as possible, to prevent the formation of circular scars. Draf Type 2 drainage.
Endonasal Surgery of the Paranasal Sinuses
Indications
 Acute or chronic ethmoid, maxillary, frontal and/or sphenoid sinusitis, polyposis of the nose and sinuses.
Acute or chronic ethmoid, maxillary, frontal and/or sphenoid sinusitis, polyposis of the nose and sinuses.
 Orbital complications of ethmoiditis.
Orbital complications of ethmoiditis.
 Surgical approach to the orbit.
Surgical approach to the orbit.
 Drainage of mucoceles, pyoceles, and pneumatoceles.
Drainage of mucoceles, pyoceles, and pneumatoceles.
 Tumors of the lateral nasal wall and of the paranasal sinus system.
Tumors of the lateral nasal wall and of the paranasal sinus system.
 Fractures involving the paranasal sinus system, midface, orbit, and optic nerve.
Fractures involving the paranasal sinus system, midface, orbit, and optic nerve.
 Management of the dura secondary to injuries to the roof of the ethmoid.
Management of the dura secondary to injuries to the roof of the ethmoid.
Anatomical Aspects of the Paranasal Sinus System
 An anterior vertical part at the lateral edge of the lamina cribrosa.
An anterior vertical part at the lateral edge of the lamina cribrosa.
 A middle frontal part, lateral to the skull base and extending to the lamina papyracea.
A middle frontal part, lateral to the skull base and extending to the lamina papyracea.
 A posterior horizontal part, forming the roof of the posterior third of the middle meatus.
A posterior horizontal part, forming the roof of the posterior third of the middle meatus.
Preparation for Endonasal Surgery of the Paranasal Sinuses
Preoperative Measures to Achieve Decongestion
Local Anesthesia
Surgery of the Maxillary Sinus
Endoscopy of the Maxillary Sinus (Sinuscopy, Antroscopy)
Surgical Principle
Indications
 Culture swab for suspected mycosis or immune suppression.
Culture swab for suspected mycosis or immune suppression.
 Biopsy for suspected malignancy.
Biopsy for suspected malignancy.
 Cyst excision.
Cyst excision.
Contraindications
Anesthesia
Instruments
Surgical Technique
Postoperative Care
 Risks and Complications
Risks and Complications
 Injury to the wall of the maxillary sinus, orbit, retromaxillary space with bleeding, abscess formation, phlegmon, thrombophlebitis, and eye symptoms.
Injury to the wall of the maxillary sinus, orbit, retromaxillary space with bleeding, abscess formation, phlegmon, thrombophlebitis, and eye symptoms.
 Air emboli have never been reported, although they cannot be completely ruled out.
Air emboli have never been reported, although they cannot be completely ruled out.
 Surgical emphysema, paraesthesias, hypaesthesias and neuralgia in the distribution of the second branch of the trigeminal nerve, buccal phlegmon, and abscess formation after using the transoral approach.
Surgical emphysema, paraesthesias, hypaesthesias and neuralgia in the distribution of the second branch of the trigeminal nerve, buccal phlegmon, and abscess formation after using the transoral approach.
Endonasal Enlargement of the Maxillary Ostium
Surgical Principle
Indications
 Incipient complication of an acute maxillary sinusitis.
Incipient complication of an acute maxillary sinusitis.
 Acute recurrent maxillary sinusitis.
Acute recurrent maxillary sinusitis.
 Chronic maxillary sinusitis.
Chronic maxillary sinusitis.
 Cysts and mucoceles.
Cysts and mucoceles.
Specific Points Regarding Informed Consent
 Postoperative bleeding.
Postoperative bleeding.
 Injury to the nasolacrimal duct.
Injury to the nasolacrimal duct.
 Paraesthesias in the region of the canines and incisors from an opening created too far forward, damage to the unerupted teeth in children.
Paraesthesias in the region of the canines and incisors from an opening created too far forward, damage to the unerupted teeth in children.
Operative Planning
Anesthesia
Special Instruments and Implants
Endoscopic Technique for Endonasal Enlargement of the Maxillary Ostium
Microscopic Technique for Enlargement of the Maxillary Ostium
 Risks and Complications
Risks and Complications
 Postoperative bleeding from the sphenopalatine artery after enlarging the ostium too far dorsally.
Postoperative bleeding from the sphenopalatine artery after enlarging the ostium too far dorsally.
 Injury to the nasolacrimal duct.
Injury to the nasolacrimal duct.
 Paraesthesias in the region of the canine and incisor teeth, from enlarging the ostium too far anteriorly.
Paraesthesias in the region of the canine and incisor teeth, from enlarging the ostium too far anteriorly.
 Damage to the unerupted teeth in children, which must be avoided.
Damage to the unerupted teeth in children, which must be avoided.
Surgery of the Ethmoid
Surgical Principle
Infundibulotomy
Surgical Principle
Indications
 Acute, acute recurrent, and chronic nasal parasinusitis, especially in the region of the anterior ethmoid cells and the frontal and the maxillary sinuses without any significant changes to the mucous membranes.
Acute, acute recurrent, and chronic nasal parasinusitis, especially in the region of the anterior ethmoid cells and the frontal and the maxillary sinuses without any significant changes to the mucous membranes.
 Mucoceles.
Mucoceles.
Contraindications
 Pronounced nasal polyposis involving the entire paranasal sinus region.
Pronounced nasal polyposis involving the entire paranasal sinus region.
 Bleeding tendency and coagulopathies that are irreversible or therapy-resistant.
Bleeding tendency and coagulopathies that are irreversible or therapy-resistant.
Specific Points Regarding Informed Consent
Anesthesia
Instruments
Endoscopic Surgical Technique
Endoscopic–Microscopic Infundibulotomy
Endonasal Surgery of the Ethmoid
Surgical Principle
Indications
 Acute and chronic sinusitis.
Acute and chronic sinusitis.
 Orbital complications of sinusitis.
Orbital complications of sinusitis.
 Intracranial complications of sinusitis.
Intracranial complications of sinusitis.
 Drainage of muco-, pyo-, and pneumatoceles.
Drainage of muco-, pyo-, and pneumatoceles.
 Trauma: extensive fracture of the ethmoid, fracture of the anterior cranial base, and/or decompression of the optic nerve.
Trauma: extensive fracture of the ethmoid, fracture of the anterior cranial base, and/or decompression of the optic nerve.
 Tumors.
Tumors.
 Access to the orbit.
Access to the orbit.
Endoscopic Surgical Technique
Microscopic Surgical Technique
Surgery of the Sphenoid
Endonasal Opening of the Sphenoid Sinus
Surgical Principle
Indications
 Acute and chronic isolated sphenoid sinusitis.
Acute and chronic isolated sphenoid sinusitis.
 Acute and chronic parasinusitis.
Acute and chronic parasinusitis.
 Irradication of the underlying focus of ocular complications (retrobulbar neuritis, optic neuritis, cavernous sinus thrombosis).
Irradication of the underlying focus of ocular complications (retrobulbar neuritis, optic neuritis, cavernous sinus thrombosis).
 Exploration and biopsies for suspected tumors.
Exploration and biopsies for suspected tumors.
 Mucocele formation in the region of the sphenoid sinus.
Mucocele formation in the region of the sphenoid sinus.
 Cerebrospinal fluid (CSF) fistula in the sphenoid region.
Cerebrospinal fluid (CSF) fistula in the sphenoid region.
Operative Planning
Special Instruments
Anesthesia
Surgical Technique
 When removing the anterior wall of the sphenoid sinus, care should be taken not to remove it too far laterally and posteriorly, as it is possible to injure the internal carotid artery or the optic nerve, which both run here. Nor should the anterior wall be removed too far caudally and laterally, because of the course of the sphenopalatine artery.
When removing the anterior wall of the sphenoid sinus, care should be taken not to remove it too far laterally and posteriorly, as it is possible to injure the internal carotid artery or the optic nerve, which both run here. Nor should the anterior wall be removed too far caudally and laterally, because of the course of the sphenopalatine artery.
Surgery of the Frontal Sinus
Endonasal Surgery of the Frontal Sinus
Surgical Principle
Indications
 Draf Type 1: Simple drainage of the frontal sinus for uncomplicated disturbances of aeration of those frontal sinuses with a wide natural ostium.
Draf Type 1: Simple drainage of the frontal sinus for uncomplicated disturbances of aeration of those frontal sinuses with a wide natural ostium.
 Draf Type 2A: Removal of ethmoid cells obstructing the frontal recess to produce a natural wide funnel.
Draf Type 2A: Removal of ethmoid cells obstructing the frontal recess to produce a natural wide funnel.
 Draf Type 2B: For recurrences and narrow ethmoid, small natural frontal sinus ostium.
Draf Type 2B: For recurrences and narrow ethmoid, small natural frontal sinus ostium.
 Draf Type 3: Reserved for revision surgery after acute and chronic sinusitis, mucoceles located far medially, and endocranial complications of sinusitis (cautious indication).
Draf Type 3: Reserved for revision surgery after acute and chronic sinusitis, mucoceles located far medially, and endocranial complications of sinusitis (cautious indication).
Anesthesia
Instruments
Surgical Technique
![]()
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree