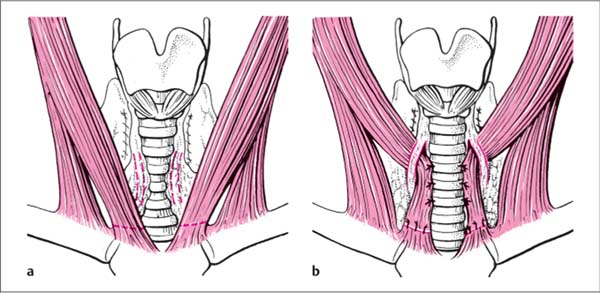
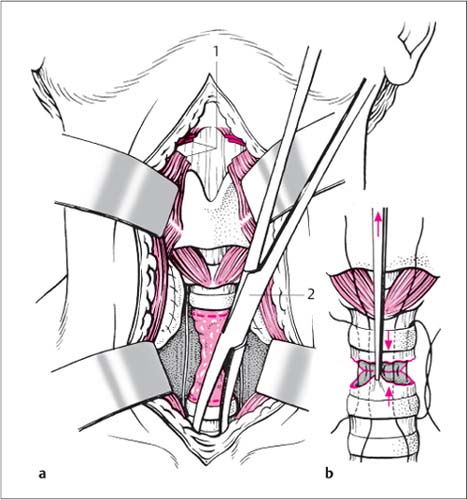
10 Surgery of the Larynx, Hypopharynx, and Trachea Endolaryngeal operations may be performed under topical anesthesia using indirect laryngoscopy or—and this is virtually standard practice nowadays—under general anesthesia and under direct vision using the operating microscope. Direct microlaryngoscopy under general anesthesia has the additional option of using angled telescopes, which provide significantly better exposure for even poorly accessible areas. Involves performing localized endolaryngeal operations under topical anesthesia using curved instruments, under mirror or angled endoscopic guidance (mirrored vision involves guiding the instruments in the opposite direction). Curved cotton buds, Reichhardt epiglottis retractor, epiglottis double-cup grasping forceps and punches, or curved universal handpiece with various tools. Binocular microscope with a 30-cm objective lens or magnifying laryngoscope. Premedication (atropine, administered IM 20 minutes before surgery, plus trifluopromazine or pethidine if required, although they are not obligatory for outpatient surgery.) The patient should be fasting. Topical anesthesia with lidocaine. The oral cavity, pharynx, and laryngeal mucosa are sprayed successively, and the larynx is additionally brushed with anesthetic on a curved cotton bud under indirect laryngoscopic vision. A hyperactive gag reflex will require a peripheral block of the superior laryngeal nerve from an external approach and infiltration of the glossopharyngeal nerve at the inferoposterior tonsillar pole, each with 2 mL 1 % lidocaine. Positioning. The patient is positioned sitting upright, with slightly reclined head stabilized in the headrest in preparation for binocular microscopy. The assistant may stand just behind the patient’s left shoulder. Preparation. Appropriate instrument attachment piece (double-cup grasping forceps and punch); the working direction of the attachment is parallel to the vocal fold and is verified using thumb and index finger of the left hand, which are spread apart in a V shape to simulate the position of the vocal folds. Insertion of the instruments. The tongue is held from the right by the patient or an assistant. The laryngoscope or magnifying laryngoscope is inserted with the left hand and the larynx visualized (if necessary, first adjust the microscope with the right hand). If necessary, ask the patient to phonate (Fig. 10.1a). Technique for overhanging epiglottis. With an overhanging epiglottis, the Reichhardt retractor is positioned beneath the epiglottis and supported by the assistant. Tissue removal. Using the right hand, the closed instrument is introduced laterally through the mouth into the larynx under vision. The instrument is advanced with the position of the vocal folds during respiration and the tissue removed (optimal view and complete anesthesia are absolute prerequisites for precise positioning) (Fig. 10.1a–c). Hemostasis. The excision site is checked, a second sample is taken if necessary, the area is smoothed out, and hemostasis is achieved with a cotton bud soaked in a vasoconstrictive agent. Fig. 10.1a–c Indirect biopsy from the larynx under the guidance of a magnifying laryngoscope. a Cross-section. Head reclined. Tongue drawn far forward. b Positioning the opened biopsy graspers with the position of the vocal folds during respiration. c Directing the instrument from the angle of the mouth with the right hand, while guiding of the magnifying laryngoscope with the left hand. Direct laryngoscopy. Direct endolaryngeal operations are always performed under general anesthesia, usually as so-called “direct distending laryngoscopy.” After intubation using a relatively thin tube, a relatively wide, conical endoscope tube is introduced into the larynx and stabilized with a support placed on the chest. This allows fine manipulations to be performed bimanually under microscopic, stereoscopic vision and without time restrictions from pauses for breathing. The walls and the sinus of Morgagni are inspected using angled telescopes. The ventricle is held open with small retractors to allow inspection. Microlaryngoscopy/hypopharyngoscopy, rigid tracheobronchoscopy: A set of operating laryngoscopes (e. g., Kleinsasser) with chest support and fiber-glass illuminator, distending laryngoscope (e. g., Weerda), the Lindholm self-retaining vocal fold retractor. A set of instruments for laryngeal microsurgery with double-cup grasping forceps and small scissors with various types of curved blades, needle holder, sickle blade, curette, suction tubes, and diathermy. Operating laryngoscopes and instruments should all have suction tubes for laser surgery. Operating microscope with 400-mm lens, side-viewing endoscope. Intubation with a 24–28 Fr Woodbridge or single-use tube for adults, appropriately smaller tubes for children. Complete muscle relaxation should be achieved for inserting the laryngo-scope. Alternatively, jet ventilation anesthesia or intermittent ventilation with the option of performing the operation during apnea. Positioning. The patient should be positioned absolutely flat on the operating table, head dorsally flexed and stabilized in a small rubber ring. Remove dentures, if this has not already been done, and insert a mouth guard. After insertion of the laryngo-scope, the whole operating table is inclined to approx. 30°. Exposure. Recline the head with the left hand. Displace the lip to one side and introduce the laryngoscope from the right corner of the mouth—displacing the tongue to the left—and let it glide deeper down, using the intubation tube as a guide (Fig. 10.2). The tip of the blade elevates the epiglottis; it is introduced into the larynx under direct vision until the vocal folds are fully visible. Fixation of the endoscope. Fix the endoscope in this position by placing the support onto the holding plate, which is positioned on the chest (Figs. 10.3 and 10.4). If insertion is difficult or there is inadequate visualization, the telescope may also lie obliquely in the corner of the mouth or in a gap in the teeth; in addition, a smaller-caliber tube may be resorted to. Optimization of exposure. Tightening the adjusting screw on the side will improve the view of the anterior commissure as well as stabilizing the support; care should be taken here, however, because this increases pressure on the incisors. External counter-pressure on the larynx also improves the view into the anterior larynx (Fig. 10.4). Exposure of the posterior commissure. The posterior commissure only comes into view after the tube has been elevated by the laryngoscope. The telescope should be advanced a little further if the vocal folds are obscured by the false cords; introducing the endoscope too deeply will excessively abduct and even occasionally injure the vocal folds. Inspection of the subglottis and the sinus of Morgagni. The subglottic space and the sinus of Morgagni cannot be viewed completely, even with optimal visualization, and therefore need to be inspected with the aid of angled telescopes. It has proved helpful here to elevate the false cords with an angled blunt hook. Fig. 10.2 Direct distending laryngos-copy: first step. Insertion of the laryngoscope tube into the oral cavity and oropharynx. Fig. 10.3 Direct distending laryngos-copy: second step. After the endolaryngeal space is exposed, the support is positioned on the chest. Examination of the ventricles may be optimized by lateral pressure as well as by pressing the tip of the laryngoscope laterally against the false cord. Fig. 10.4 Direct distending laryngoscopy: third step. The alignment of support and laryngoscope tube can be regulated by an adjusting screw. Jet ventilation allows an intubation-free general anesthesia with muscle relaxation when the larynx is narrow or where there are alterations in the most posterior part of the vocal folds or in the region of the posterior wall. Rapid insertion of the operating microscope is followed by connection of the injector cannula to the ventilator; the oxygen supply should be carefully monitored. If significant hemorrhage should occur, e. g., during carcinoma resection, then rapid intubation should be considered, followed by tracheobronchoscopy to aspirate blood, should hemostasis not be achieved immediately. Direct inspection of the larynx and trachea under general anesthesia using a thin tube (available also battery-operated for emergency cases) and ventilator connection, especially during emergency endoscopy or where intubation proves difficult. Severe general disorders precluding general anesthesia. As for direct distending laryngotracheoscopy. Laryngoscope blades, emergency tracheoscope (various diameters and lengths), appropriate suction probes and double-cup grasping forceps which can be introduced through the tube. Before inducing muscle relaxation, it should be ensured that mask ventilation is possible or that insertion of the telescope through the glottis has been successful. Positioning. Position the patient flat on the operating table, head slightly raised, neck maximally reclined. Remove dentures. Oxygenate well using mask ventilation before commencing the procedure. Ensure muscle relaxation (see above), consider insertion of a mouth guard. Unfolding the pharynx. The laryngoscope blade (which should not be too large) is inserted with the left hand, past the right-hand corner of the mouth toward the midline, and the tip is slid as far as the vallecula. Do not elevate the epiglottis. The right hand maintains the head in reclination. Lifting the blade in the direction of the laryngoscope handle (do not lever it) will unfold the pharynx and raise the epiglottis until the arytenoid cartilage and posterior parts of the vocal folds come into view. Apply suction (Fig. 10.5a, b). Introduction of the laryngoscope. With the right hand, pass the emergency laryngoscope tube (with tube size selected to suit the larynx or any stenosis present) from the corner of the mouth beneath the epiglottis—if possible, use any gap in the teeth—and then withdraw the laryngoscope blade. Exposure of the larynx. The arytenoid cartilages with their mucosal coverage are now visible through the tube. Elevate the tip of the tube slightly and slide it under direct vision as far as the glottis. The tube is first rotated 90° just before the glottis and the slender tip is introduced into the glottis; during the subsequent passage, the tube is rotated back again and the entire diameter of the tube is passed through the glottis. During this maneuver, the tube is supported at the teeth with the thumb and index finger of the left hand, while the head is maintained in reclination (Fig. 10.6). Inspection of the trachea. Carefully withdraw the tube past the level of the glottis to inspect the larynx and then advance it back into the trachea and ventilate. Do not allow unduly long ventilation gaps. Check oxygen saturation. Fig. 10.5a, b Direct laryngotracheoscopy. a Positioning with raised and reclined head. The laryngoscope blade is held with the left hand and drawn in the direction of the handle. b The ventilation laryngotracheoscope is introduced with the right hand from the corner of the mouth. The tip of the tube slides over the epiglottis and is then raised slightly. Fig. 10.6 Direct laryngotracheoscopy. 1 arytenoid cartilage, vocal folds, vestibular folds are visualized 2 for insertion into the trachea, the tip of the tube is positioned in the sagittal direction and then advanced through the glottis 3 rotating the tube 90° allows its entire circumference to pass the glottis when advanced further Fig. 10.7a, b Procedure for the difficult intubation. a A thin bougie is introduced into the trachea via a ventilation tracheobronchoscope. b Intubation via the bougie, under digital guidance. Place the polyps on traction with grasping forceps and incise the mucosa around the base of the polyp with straight or curved scissors, without injuring the muscle or vocal ligament. If necessary, the incision margins can be carefully evened out with small scissors. Avoid creating opposing mucosal defects in the anterior commissure. Hyperkeratoses are often indistinguishable macroscopically from carcinomas in situ. Therefore, always excise completely leaving an adequate safety margin—but superficially. One option is to inject a vasoconstricting agent into a lesion-free area of the vocal fold to elevate the superficial mucosal layer from its undersurface (hydrodissection). Incise the mucosa behind the hyperkeratosis transversally using scissors, a sickle blade, or a straight disk blade, then slit it anteriorly along the sinus of Morgagni and incise again using scissors anteriorly, in front of the anterior commissure as far as the free border of the vocal fold. Then elevate the mucosal flap thus created with a fine forceps and release it extensively with scissors or the disc blade before excising it behind the end of the lesion at the free border of the vocal fold. Hemostasis is achieved with a cotton bud soaked in epinephrine, for example. In the presence of Reinke edema, it is recommended to open Reinke space along the ventricle, i. e., in the direction of vocal folds, and remove the thick liquid contents by suction (Fig. 10.8). The part of the mucosa covering the region of incision is reflected back. Then, any excess mucosa is carefully excised, avoiding removing too much. If bilateral treatment is required, an incision is made on one side transverse to the anterior commissure, which is not correspondingly denuded. Fig. 10.8 Opening the Reinke space with the curved blade or the disc blade. Mucosal injuries in the region of the anterior commissure with an opposing wound surface in the region of the anterior vocal folds may become the origin of extensive web formations, which will then require treatment. Postoperative voice therapy is advised for polyps of the vocal folds and occasionally also for Reinke edema. Surgical treatment of cysts may consist either of excision or, in many cases, enucleation. Cysts of the vocal folds are by no means always confined to the free margin, but may also occur on the subglottic wall. More or less pronounced phonatory gap with subsequent hoarseness. None, apart from medical aspects. Mucosal incision. After exposing the lesion using microlaryngoscopic technique, the mucosal membrane covering the vocal folds is incised and drawn medially with fine forceps. Excision of the cyst. The complete enucleation of the cyst then follows. The real value of selective laser surgery undertaken with low performance parameters in the treatment of Reinke edema and vocal fold polyps has not yet been clarified. The question remains: Why should a thermal resection technique be used when the above-mentioned indications can be successfully treated with cold-steel surgery and complementary speech therapy? Always use microscopic magnification. Use both hands: the left hand guides the forceps to grasp the tissue and puts it on stretch, while the right hand dissects. Flex the arms slightly and if necessary support the elbows. Ensure optimal visualization, remove blood by suction, consider infiltration with a saline solution supplemented with epinephrine (1:10 000). Ensure hemostasis by pressure of a cotton bud soaked in naphazoline, and also consider microsuction diathermy. Exposure. First, ensure optimal exposure of the anterior commissure. Web release. The web is released on one vocal fold side as far as the anterior commissure, either using cold steel or by laser surgery; the epithelial tip thus formed is held up with a suture or tissue glue. Insertion of the spacer. If recurrence of the web occurs, the web lamina is excised as a triangle and a narrow triangular dilator made of silicone is inserted into the anterior commissure for ca. 3–4 weeks. It is important to mention that the increased production of granulation tissue is occasionally observed after spacer insertion, and can considerably interfere with the healing process. Positioning the spacer. A thin cannula is inserted into the larynx at the inferior edge of the thyroid cartilage; a nylon suture is passed through its lumen into the larynx, grasped with a fine grasping forceps, and withdrawn superiorly. The cannula is then withdrawn. The triangular silicone wedge is threaded onto the suture; the length of the dilator should not exceed 1.5– 2 cm. The superior thread is now re-introduced into the larynx, a Reverdin needle is inserted slightly obliquely in an inferior direction through the thyroid notch, and the suture is threaded onto the needle and withdrawn. The thread is then knotted externally over a dental swab under mild traction, after checking the position of the dilator on the inside and, if necessary, correcting it. An instrument for advancing the needle, which was developed by Lichtenberger, has proven of assistance during this maneuver (Endo-extralaryngeal Needle Holder, 8267.50, Wolf, Knittlingen, Germany) and may also be used for the reversible endo-extralaryngeal expansion of the glottis (p. 200). After completion of epithelialization, which usually takes about 4 weeks, the dilator is removed by repeat endoscopy. Tracheotomy is not usually required. Even though long-term trials and controlled studies still remain to be undertaken, there are indications that topical application of mitomycin C after division of the anterior glottic stenosis demonstrates better long-term results than those after web release alone. Web release can be done with cold steel or using a CO2 laser. An excavated vocal fold in the intermediate position can be medialized by injecting autologous fat or collagen; this is known as augmentation. The problem with autologous fat injection is that the absorption rate is unpredictable, requiring a repeat injection after months to years. Unilateral incomplete glottic closure. Severe general disorder that does not justify the risk of a general endotracheal anesthesia. Complications as for microlaryngoscopy. Three-ring syringe (e. g., Ultra-Asept K. Storz, Tuttlingen, Germany), injection cannula (e. g., PV 27 200S 18-cm injection cannula, K. Storz, Tuttlingen, Germany). (Peri-) umbilical skin incision with harvesting of fat and transfer into the injection cannula. Abdominal wall fat is harvested surgically via a skin incision extending into the umbilicus and is then manually fragmented. Alternative technique for autologous harvesting of abdominal wall fat. An 18 G needle is inserted into the subcutaneous abdominal fatty tissue. The plunger is retracted to create a vacuum. Material is harvested by moving the needle around in the subcutaneous tissue. The harvested material is rinsed with saline solution. When allowed to stand it settles out into three layers: (1) free fatty acids; (2) fat cells; (3) blood cells, saline solution, and cellular particles. The layer containing the fat cells is filtered out with a sieve (e. g., a tea strainer) to separate it from the other layers. Endolaryngeal injection. The harvested fat is injected with a three-ring syringe using a long 19 G needle. The autologous fat can easily be injected through this long needle. Autologous fat injection can be used on the vocal folds, the false cords, the aryepiglottic folds of the larynx, and the medial wall of the piriform sinus. Autologous fat can be injected at the vocal fold membrane into the thyroarytenoid muscle to improve atrophy of the vocal fold and incomplete glottic closure. The fat is also injected into the thyroarytenoid muscle at the part near the cartilage to produce rotation of the arytenoid cartilage. Autologous fat may also be injected into the false cord and the aryepiglottic fold. Fat injections into the vocal fold, false cord, or aryepiglottic fold are intended to compensate atrophy of the laryngeal tissue and to facilitate glottic closure. In addition, fat can also be injected into the medial wall of the piriform sinus of the hypopharynx to reduce its width. Since the introduction of the basic technique of thyroplasty by Isshiki over 25 years ago, it has become a frequently used procedure in laryngeal surgery for the treatment of incomplete glottic closure. Various modifications of Isshiki type I thyroplasty have been suggested to improve operating time, placement of the implant, and implant material (e. g., autologous cartilage implants or alloplastic material such as hydroxylapatite, vitalium [miniplates], and polytetrafluoroethylene [Gore-Tex]). In 1999 Friedrich, from Graz, Austria, reported a surgical technique in which external vocal fold medialization is undertaken using an adjustable, pre-formed titanium implant for vocal fold medialization. It is the author’s view that this procedure, which has since been increasingly used, may be regarded as a proven form of therapy for vocal fold medialization in cases that remain unsuccessful, or apparently so, after medialization by augmentation using autologous fat transfer. The reason is the titanium prosthesis developed by Friedrich, which allows an uncomplicated and time-saving operation with adequate fixation over the thyroid cartilage. Inadequate medialization achieved by autologous fat injection (although fat injection is not necessarily a prerequisite). Unilateral incomplete closure of the glottis. Severe general disorder that does not justify the risk of a surgical intervention. Complications as for microlaryngoscopy, skin incision at the level of the thyroid cartilage, titanium spacer, wound infection, wound breakdown, intolerability, dyspnea, tracheotomy. For example, the Friedrich prosthesis (K. Storz, Tuttlingen, Germany), microlaryngoscopy (MLS) tube, drill if needed. The operation should be performed under local anesthesia to be able to adjust the depth of the implant intraoperatively to the optimal voice quality achieved. Skin incision. After infiltration using 1 % lidocaine with the addition of epinephrine, a skin incision is made at the level of the thyroid cartilage, which is then exposed while protecting the perichondrium. Construction of a cartilaginous window. A reference line is drawn parallel to the inferior edge of the thyroid cartilage, beginning in the middle between the superior and inferior borders of the thyroid cartilage arch. The line divides the distance between the superior and inferior borders of the thyroid cartilage in a ratio of 2:1 and corresponds to the free border of the vocal folds in the endolarynx. A further important landmark for the fenestration is the oblique line. The cartilaginous window should be positioned caudal to the reference line and the inferoposterior corner of the window, close to the oblique line. For the 13-mm implant (which is normally used for female patients), the size of the window should be 6 × 11 mm, while for the 15-mm implant (normally used for male patients) it should be 6 × 13 mm. After the window is marked, cartilage and bony material are drilled out with a steel drill until the internal perichondrium becomes visible (Fig. 10.9a). Once the internal perichondrium has been reached, the edges and corners of the window are smoothed with a small diamond drill. The internal perichondrium is incised along the dorsal margin and in part along the inferior and superior margin, using an electric knife. It is important that the paraglottic space is not encroached upon and the endolaryngeal vessels are not touched. Fig. 10.9a–d Medialization of the vocal folds after Friedrich. a A cartilaginous window is drilled out down to the inner perichondrium. b Creation of subperichondrial pocket ventrally, insertion of the Friedrich prosthesis with the aid of a clamp—first ventrally, then dorsally. c Fixation of the Friedrich prosthesis in a dorsal direction using a monofilament suture. d Final appearance after dorsal placement of the Friedrich prosthesis and fixation with two sutures. Placement of the implant. A subperichondrial pocket is created ventrally. The dorsal edge of the Friedrich prosthesis is held with a clamp and first inserted ventrally (Fig. 10.9b). The basal plate of the Friedrich prosthesis is 2 mm larger than the cartilaginous window. The implant must therefore be slightly bent between the clamp and index finger of the other hand. This allows the prosthesis to be inserted through the cartilaginous window into the endolarynx under mild tension. The optimal depth of medialization is determined by pressing the prosthesis in and marking the position with the clamp according to the optimal voice achieved. The dorsal edge is bent in a dorsal direction at the level of this mark and the prosthesis secured with two stitches of a monofilament, nonabsorbable suture (Fig. 10.9c). Due to the form of the prosthesis, no further fixation in the ventral region is usually required (Fig. 10.9d). It is recommended to administer a single dose of 250 mg prednisolone and a one-off perioperative dose of a broad-spectrum antibiotic, which should be given 30–60 minutes before surgery. Adjuvant speech therapy is beneficial. Isshiki or Montgomery vocal fold medialization. Laser surgery of benign and circumscribed malignant tumors of the larynx has become a common treatment concept in many institutes. The final assessment of this method in terms of reproducible long-term results has not yet reached a conclusion, especially as a therapeutic concept for advanced laryngeal carcinoma and in comparison to possible alternative treatments. The use of laser surgery techniques is inextricably linked to the need for sound surgical training. It should in no way be understood as being “easier” than partial surgical resection using an open approach. This is all the more true when laser surgery is used for transoral treatment of advanced laryngeal carcinomas, although the required experience in this very demanding microsurgical technique may be lacking. Furthermore, situations will always arise, even with very experienced surgeons, where the difficulties of a tumor exposure that is “just about” acceptable or functional limitations during the postoperative course become apparent. These caveats indicate why endolaryngeal laser surgery has its detractors. There are some recognized laryngologists who regard laser surgery merely as a helpful alternative in certain indications, and a few who strictly rule out laser surgery of the larynx. Modern laser technology allows surgery using a precisely aligned laser beam without producing any significant carbonization. A micromanipulator that produces a laser beam well below 0.5 mm in diameter should be used. The physical properties of the laser beam allow maximum use of both cutting qualities and coagulation. Laryngoscope tube and instruments with special suction units; protective eyewear. Operations may be carried out under general anesthesia, intermittent apnea, or jet ventilation. Various safety precautions must be observed during use of the laser in order to avoid serious complications, such as ignition of the endotracheal tube with its potentially fatal outcome. It is known that the endotracheal tube usually ignites if the laser beam accidentally penetrates unprotected components of the tube. The greatest risk potential lies in the cuff region and the tip of the endotracheal tube. Because the cuff region is particularly vulnerable, it is recommended to cover it with damp neurosurgical cotton padding. The risk can be further minimized by inflating the cuff with dyed physiological saline instead of air. The blue dye will immediately indicate that the cuff is damaged. If the tube ignites despite these precautions, then immediate disconnection of the ventilation tube from the ventilator is necessary, with removal of the laryngoscope, followed by re-intubation and interdisciplinary emergency management of the patient (depending on the severity—pulmonology, intensive care, visceral surgery, nephrology, etc). After extubation, laryngotracheal injection of Ringer solution may be initiated using a preprepared 50 mL syringe, provided the laryngoscope is still in its original position. The introduction of the CO2 laser into laryngology began with the treatment of benign disorders. The benign lesions of the larynx described in this chapter, such as cysts and granulomas, may also be resected using cold-steel instruments, with equivalent therapeutic results. For certain indications, such as laryngeal papillomatosis, however, laser surgical treatment is usually more advantageous than conventional surgery. Intubation should be avoided. Excision of the intubation granuloma should be undertaken during an apnea phase or, if appropriate, using jet ventilation. The glottis is exposed using a closed laryngoscope; the granuloma is grasped and excised at its base. Unnecessarily excessive exposure of the arytenoid cartilage should be avoided. Because of the presence of persisting inflammation, recurrences in the region of the vocal process may originate from the perichondrium. This also applies after careful removal using the CO2 laser. Speech therapy. Excision or marsupialization of the soft, more or less spherical, bulge of mucosa protruding from the ventricle or the mucosa and extending into the supraglottic space. Circumscribed external laryngoceles which are accessible by the open or endolaryngeal route. As for microlaryngoscopy. Exposure. Transoral surgery of laryngoceles requires exposure of the supraglottic region with the aid of a closed or open laryngoscope. Identification of the laryngocele. The mucosa covering the laryngocele is incised in the region of the false cord or the aryepiglottic fold and the wall of the laryngocele is identified. Opening the laryngocele. After the laryngocele is opened, it becomes apparent whether it contains air or thin or viscous mucus. Transoral resection of the laryngocele. The secretion is removed by suction. After the subsequent collapse of the laryngocele, it may be dissected peripherally and completely excised, even in the case of smaller laryngoceles. Marsupialization. Often wide marsupialization of the laryngocele in the direction of the internal larynx is also possible. This applies particularly to extensive laryngoceles. Approach for external laryngoceles. Depending on their extent, external laryngoceles are removed using conventional surgical technique via an open approach (p. 282) or, in special cases, marsupialization is performed transorally using the CO2 laser surgical technique as described above. Vaporization of papillomas, which at the time may comprise multiple foci, may be repeated at short intervals, depending on the activity of the disorder, e. g., to avoid the necessity of a tracheotomy. Histological confirmation of the disorder is absolutely essential, however, even with more or less complete vaporization. In addition to endolaryngeal manifestations, patients with laryngeal papillomas must be assessed for possible extralaryngeal involvement of the tracheobronchial system as well as the region of the upper digestive tract. Papillomatosis of the upper aerodigestive tract. As for microlaryngoscopy. Surgery for laryngeal papillomas is performed on the intubated patient or with intermittent apnea or using jet ventilation to allow an optimal endolaryngeal view. A slightly defocused laser beam is usually employed. Low laser power allows the controlled removal of the polyps, while ensuring that surgery is restricted to the mucosa. With bilateral involvement of the vocal folds it should be ensured that near the anterior commissure the laser is only used unilaterally to minimize the risk of postoperative web formation. A single-dose application of a steroid (e. g., 3 mg/kg prednisolone) may be helpful to avoid postoperative dyspnea. In addition to laser surgery, promising results have been achieved using photodynamic therapy. Further studies in the future will show to what extent long-term freedom from papillomas is possible with this type of treatment. There is an increasing number of trials using systemic treatments for extensive forms of papillomatosis with involvement of the tracheobronchial tree. Isolated results with interferonα2b or the intralesional injection of the antiviral drug cidofovir do not as yet allow a conclusive assessment of the value of this type of therapy. About 60–70 % of stridor-associated laryngeal anomalies in childhood are attributed to laryngomalacia. The stridor associated with laryngomalacia is either congenital or manifests itself within the first weeks after birth. The symptoms of stridor will have reached their maximum by the age of 6 months, after which they usually recede by the end of the second year of life. Active surgical intervention is required in ca. 20 % of cases of laryngomalacia. An inward collapse of the supraglottic mucosa during inspiration is an indication for a so-called supraglottoplasty. This term includes all forms of surgical treatment that are aimed at reducing the hypermobile supraglottic tissue. In most cases this involves the mucosa of the aryepiglottic folds and the arytenoid cartilage regions. If the symptoms of stridor result from short aryepiglottic folds, then bilateral laser surgical incision of these anatomical structures can usually be made. On the other hand, if there is an inward collapse of the epiglottis during inspiration, then a so-called epiglottopexy should be performed. These various treatment strategies for infants suffering from severe laryngomalacia underline the need for a careful preoperative diagnostic assessment, including an examination of the tracheobronchial system. Swallowing problems (dysphagia), dyspnea, and life-threatening symptoms of apnea. Intermittent apnea or general endotracheal anesthesia (e. g., for epiglottopexy). Intubation and general approach. All the following measures are preceded by flexible laryngo (tracheobroncho) scopy, with the infant held upright. To diagnostically assess the underlying cause of inspiratory stridor in infancy or childhood, the supraglottic region is viewed using an intubation blade. This is followed by rigid endoscopy and imaging via a monitor with the child sedated and breathing spontaneously. This will allow the diagnosis of laryngomalacia and the various forms of laryngeal and tracheal stenosis to be obtained. A tracheobronchoscopy may be regarded as obligatory. If the condition is to be treated transorally using laser micro-surgery, then the question arises as to whether to operate with the patient intubated or using intermittent apnea. If the latter technique is to be used, the endotracheal tube is inserted into the trachea via the operating microscope. Oxygen saturation is monitored by the anesthetist. Once 100 % oxygen saturation is achieved, the tube is removed and laser surgery commenced. If oxygen saturation falls below 90 % (which sometimes does not occur until after 5 minutes if the patient has been sufficiently pre-oxygenated), then the patient is re-intubated via the tube until 100 % oxygen saturation has been regained. If a short-segment stenosis is present, the membranes often have a web-like appearance; this is an excellent indication for laser surgery. Anesthesia is performed as described above and CO2 lasering is commenced. It is not necessary to undertake a circular resection of the entire membranous web, as subsequently this carries the risk of creating a circumferential stenosis. Instead, a star-shaped incision should be made in the membrane, or a semi-circular portion excised. Creation of opposing wound surfaces. This involves vaporizing or superficially resecting a circumscribed part of the tongue base using laser microsurgery, subsequently creating an opposing laser wound at the lingual epiglottic fold (laser power 1–2 W) (Fig. 10.10a). Fixation of the epiglottis to the base of the tongue. Next, the epiglottis is fixed to the base of the tongue with the aid of two or three interrupted sutures using an absorbable suture material (e. g., Vicryl 4/0) (Fig. 10.10b–d). Short aryepiglottic folds require incision using CO2 laser (1 W, 0.25 mm). Tissue beneath the folds must be protected from injury during the procedure. Hemangiomas typically present as well-defined, reddish, space-occupying lesions in the posterior part of the subglottis, often at the subglottic undersurface of the vocal fold. Hemangiomas, which develop in the region of the posterior commissure and then extend along subglottic undersurfaces of both vocal folds, are less frequently seen than lesions in the region of the anterior commissure. The various therapeutic options for subglottic hemangiomas range from tracheotomy to a submucous surgical excision and systemic or intralesional steroid injections as well as the systemic administration of interferon-α2a. Circumscribed lesions can also be brought to involution using CO2 laser and low laser energy (1–2 W). The use of a Nd:YAG laser is no longer recommended because of the often significant postoperative fibrin exudation. Following the adoption of propanolol for the treatment of problematic hemangiomas in infants, it is to be hoped that the excellent effect of this medication will also be extended to reduction of the volume of subglottic hemangiomas. Unlike the biological behavior of the hemangiomas described above, vascular malformations of the larynx often only manifest themselves clinically in adulthood or are only discovered incidentally. Typical symptoms include foreign-body sensation, urge to clear the throat, or a slowly developing, usually mild stridor. Fig. 10.10a–d Epiglottopexy a Laser microsurgical vaporization of lingual epiglottal mucosa and the opposing mucosa of the base of the tongue. b–d Stepwise fixation of the epiglottis to the base of the tongue using as many as three interrupted sutures. There are no contraindications in the presence of an absolute indication with compromise of vital functions. General endotracheal anesthesia, surgery using intermittent apnea, jet ventilation. CO2 laser treatment of subglottic hemangiomas is performed either with the aim of shrinking the lesion, which is achieved by single laser spots (2 W) placed at adequate distances apart, or via a mucosal incision followed by enucleation of the angioma. Postoperative edema formation can usually be avoided by the careful use of CO2 laser treatment. A tracheotomy should be performed in uncertain cases. Cortisone administration is indicated. The possibility that the excellent efficacy of propanolol will be extended to subglottic hemangiomas has already been alluded to. Vascular malformations may be excised; this particularly applies to cases where the differential diagnosis is uncertain. If histological clarification is dispensed with, the vascular malformation may be brought to involution by using the Nd:YAG laser (e. g., 20 W, 0.5 seconds in single applications, bare fiber 0.6 mm). Oral medication using prednisolone, 3–5 mg/kg body weight distributed over three doses per 24 hours, has proved successful in the management of subglottic hemangiomas (in addition to laser surgical vaporization). This should be undertaken in close cooperation with pediatricians to immediately diagnose and adequately treat any subsequent arterial hypertension or temporary diabetes mellitus. Hemorrhage, edema formation with the need for tracheotomy, infection with the subsequent risk of stenosis. Paralysis of the vocal folds is most often the result of thyroid gland surgery. Its incidence depends on the surgical technique, bearing in mind that injury to the recurrent laryngeal nerve can occur even in the hands of experienced surgeons. Unilateral injuries may initially remain undetected, only to become clinically manifest in the further course of the disorder. For this reason, pre- and postoperative assessment of vocal fold function should be standardized. In the presence of unilateral vocal fold paralysis, patients usually complain of isolated dysphonia. Bilateral paralysis, however, results in a paramedian position of the vocal folds, which produces a noticeable inspiratory stridor, usually associated with dyspnea at rest and in many cases quite well-preserved voice quality. Some of those affected are capable of tolerating the associated dyspnea without any further surgical intervention, although additional infections of the upper respiratory tract can sometimes also lead to a life-threatening increase in dyspnea. Other patients, however, need immediate surgical intervention, which is usually undertaken in the form of a tracheotomy. Currently four basic operative approaches are available for expanding the glottis: This technique is based on the development of a special suture instrument with which, in the case of a bilateral paralysis of the vocal folds, a vocal fold can be temporarily lateralized. Lateralization is performed on the less mobile vocal fold. The operation should be performed as early as possible to avoid injury to the vocal fold tissue secondary to intubation, while also sparing the patient symptoms of dyspnea, which considerably affect the quality of life and are associated with anxiety states. Given that restitution cannot be expected after more than 12 months, a definitive expansion of the glottis should be undertaken in cases of recurrent laryngeal nerve paralysis lasting longer than 1 year. The same as for microlaryngoscopy, plus chondritis, soft-tissue infection, scar formation, sensory disturbances, injury to the hypoglossal nerve, wound infection, suture line breakdown, revision surgery for removal of sutures. Monofilament sutures (e. g., Prolene 2/0), special Endo-extralaryngeal Needle Holder, (8267.50, Wolf, Knittlingen, Germany), special needles (8267.951, Wolf, Knittlingen, Germany). Intermittent apnea, high-frequency jet anesthesia. Visualization of the level of the glottis. Once the level of the glottis has been visualized with the aid of a distending laryngo-scope (Fig. 10.11a), the endo-extralaryngeal sutures are positioned after temporarily removing the endotracheal tube (ensure adequate pre-oxygenization). Positioning the sutures. Two monofilament sutures are positioned with the aid of the special needle holder, using a translaryngeal approach. One end of the suture attached to the needle is inserted through the laryngoscope and brought out through the soft tissue of the neck, below the posterior third of one vocal fold (Fig. 10.11b). The needle holder is then withdrawn, the remaining end again attached to a needle, which is inserted using the needle holder above the posterior third of the vocal fold to form a loop (Fig. 10.11c) and brought out through the soft tissue of the neck. The second suture inserted to perform the laterofixation is positioned in an appropriate fashion ca. 2–3 mm ventral to the first suture loop (Fig. 10.11d). If the first suture loop is sufficient, the second loop may be dispensed with. Fixation of the sutures. After knotting the second suture loop subcutaneously, the orginal skin incision is closed. Fig. 10.11a–d Endo-extralaryngeal expansion of the glottis after Lichtenberger. a View onto the glottic and supraglottic region using a distending laryngoscope. b Subglottic positioning of the instrument for advancing the needle just in of front the vocal process with subsequent puncture through the soft tissue of the neck. c The remaining endolaryngeal suture is once again passed through the needle and brought out via the ventricle. d Final appearance with two suture loops. To achieve an optimal surgical result using the endo-extralaryngeal suture technique, the guide suture should be placed as far dorsally as possible, close to the vocal process. Occasionally there is difficulty here because the adjacent part of the thyroid cartilage is often compacted or even ossified. If it is impossible to bring the suture out transcutaneously for this reason, the method may be modified to pierce the thyroid cartilage further ventrally. The sutures may create a superficial tear or even a deep tear in the vocal fold tissue, especially when operating under inflammatory conditions. The perioperative administration of a broad-band cephalosporin is initiated as infection prophylaxis, given that bacterial colonization of the soft tissues of the neck cannot be excluded after endo-extralaryngeal passage of the suture. With regard to regaining the initially lost function of the vocal folds, the further outcome must be awaited with patience. Certainty as to whether or not physiological vocal fold function has been regained is not usually to be expected until at least 12 months after the operation. It should also be borne in mind that the prognosis of bilateral paralysis may differ for the two affected sides. Unilateral arytenoidectomy (Thornell 1948) and attenuation of the posterior part of the vocal fold muscle with lateral retraction of the vocal fold (Kleinsasser 1976), or partial resection of the false cord and craniolateral fixation (Langnickel and Koburg 1970) of the posterior vocal fold under distending microscopic visualization of the larynx. Since the introduction of the CO2 laser into otorhinolaryngology, laser surgical expansion of the glottis after Dennis and Kashima (1989) or a modification of this technique is increasingly being undertaken. The advantage of this procedure in comparison with the open approach is a better postoperative voice, on average; expansion of the glottis cannot, however, always be achieved to the same extent as with an open approach. The dilemma of operations to expand the glottis is that they can only improve the voice at the cost of breathing, or vice versa. Surgery can only represent the best possible compromise between a reduction in voice quality and improvement of breathing. Bilateral vocal fold paralysis in the paramedian position, associated with dyspnea. Subglottic stenosis or tracheal stenosis. CO2 laser with its appropriate instruments. The patient is positioned flat on the operating table. For special instruments see “Microlaryngoscopy.” Identification of the level of the glottis. Exposure of the larynx using the largest possible distending laryngoscope. The arytenoid cartilage and the posterior region of the vocal folds and false cords must be completely visible. The arytenoid cartilage and the posterior third of the vocal folds are infiltrated with a vasoconstricting agent. Incision. Under the microscope, a longitudinal incision is placed over the vocal fold, extending in an anterior-to-posterior direction over the vocal process, upward as far as the dome of the arytenoid cartilage. This incision was previously done with scissors or a sickle blade, but nowadays is usually done by CO2 laser. A further incision is made from the end of this incision over the arytenoid cartilage in a lateral direction toward the aryepiglottic fold for a distance of approximately 8–10 mm; a third incision is made from this end point to the vocal process. The mucosal triangle incised in this fashion is later discarded. Excision of the arytenoid cartilage. The cartilage is carefully taken up with grasping forceps and released from its surroundings (Fig. 10.12a). The cartilage must be removed in toto. Thinning out the posterior third of the vocal fold. Excision of the vocal fold musculature. The previously placed incision is deepened and the vocal fold musculature is largely removed in its posterior and middle parts. The conus elasticus is vertically incised posteriorly (Fig. 10.12b). Mucosal suture. The incision is repaired with two interrupted sutures (4/0 absorbable). The needle is passed first into the lower and then the upper fold using the special curved delicate needle holder. The surgical knot is tied in front of the tube and then the short end of the suture directed in an inferior direction using the grasping forceps, keeping the long end under tension. The second knot is tied as an instrument knot and drawn downward using a double hook or opened double-cup grasping forceps. Alternatively, the wound may be closed using fibrin glue (Fig. 10.12c, d). Fig. 10.12a–d Endolaryngeal microscopic expansion of the glottis after Kleinsasser. a Longitudinal incision over the posterior vocal fold and triangular mucosal excision over the arytenoid cartilage using a CO2 laser. b Release of the arytenoid cartilage. c Excision of the vocal fold muscles using scissors and grasping forceps, incision of the conus elasticus. d Suture repair of the incision. Incision of the dorsal vocal folds in the region of the vocal process while protecting the arytenoid cartilage. This approach allows an individually adapted compromise between adequate breathing and voice function. Exposure of the posterior glottis. Surgical division of the vocal ligament and the musculature of the vocal muscle by CO2 laser (usually low power) immediately in front of the arytenoid cartilage. The tissue is divided lateral to the vocal process, down to the level of the thyroid cartilage. Good respiratory results are achieved in the long term by an additional incision extending from the lateral tip of the excision area in the direction of the anterior commissure and resection of the lateral thyroarytenoid muscle. Without these measures, the initially wide glottis not infrequently becomes narrow again as a result of scar formation in the excision area. Steiner (of Göttingen, Germany) favors the bilateral posterior cordectomy to avoid injuring the ventral part of the vocal folds, which is so important for phonation. All the techniques described presuppose sound knowledge of the anatomy of each individual patient. This also allows a choice of treatment method, tailored to suit the patient. For “Rules, Tips, and Tricks” and “Risks and Complications” see p. 201. Open exposure of the laryngeal framework. Identification of the arytenoid cartilage via a window in the thyroid cartilage lamina, mobilization, and lateral displacement of the vocal process with a suture. As breathing is improved, the voice deteriorates. The procedure described here is based on the technique reported by McCall and Gardiner. This technique may be considered above all for the situation where a transoral exposure is not possible. Preoperative diagnostic examinations, indications, and contraindications, as well as the choice of sides, are the same as for the endolaryngeal technique. Intubation, tracheotomy, re-intubation. The orotracheal tube is left in the glottis to displace the arytenoid into the operative field. Positioning. A roll is placed beneath the shoulders; the head is turned to the contralateral side. Incision. The skin incision runs obliquely from the anterior margin of the sternocleidomastoid muscle, in an antero-inferior direction over the lamina of the thyroid cartilage. The incision is deepened through the platysma; the omohyoid muscle and the prelaryngeal strap muscles are divided. If still present, the thyroid gland may need to be displaced caudally. Identification of the thyroid cartilage (Fig. 10.13a). Creation of a window in the thyroid cartilage. A window is made in the thyroid cartilage. The perichondrium is incised above the planned window as an inferiorly based swing-door flap. The window is created in the cartilage with a scalpel or punch, leaving only a relatively narrow (ca. 0.5 cm) frame posteriorly and superiorly (Fig. 10.13b). The internal perichondrium is divided and a large blood vessel that regularly traverses the area is diathermied. The exposed musculature is bluntly spread apart posteroinferiorly until the arytenoid cartilage is encountered in the depths. Arytenoidectomy. While holding the musculature aside with a retractor, the arytenoid cartilage is released down to the vocal process with small scissors and the disk blade. The articular cartilage and the cricoarytenoid ligament in particular must be safely divided (Fig. 10.13c). A nonabsorbable polyester suture (e. g., Mersilene) is passed around the vocal process, which is exposed but still firmly attached to the vocal ligament, knotted initially over the cartilage, then drawn downward around the previously exposed thyroid cartilage and then knotted again. Before finally pulling this knot tight, the position of the vocal fold must be confirmed by endolaryngeal inspection with a laryngoscope and, if necessary, corrected (Fig. 10.13d, e). Wound closure. Fixation of the elevated perichondrium using a retention suture, insertion of a suction drain, wound closure in a layered fashion. Mündnich approach. The superior and posterior frame of the thyroid cartilage as described above is also excised; this considerably facilitates dissection of the arytenoid cartilage and placement of the suture during this approach, which is otherwise practically similar to that described above. In addition, a notch is placed in the inferior part of the thyroid cartilage to guide the suture. However, a partial collapse of the corresponding half of the larynx later occasionally affects the inner stability of the larynx. Fig. 10.13a–e Lateral fixation from an open approach. a Oblique skin incision over the lamina of the thyroid cartilage. b Creation of a window in the thyroid cartilage after elevation of overlaying cervical muscles. c Identification of the arytenoid cartilage. d Lateral fixation of the arytenoid cartilage with a suture passed around the vocal process and the inferior horn of the thyroid cartilage. e Lateralization as shown in the cross-section. Antibiotic, voice rest, antitussive agents, steroids for significant edema. Remove drain on the second or third day; phoniatric treatment may be indicated later. Decannulation after the endolaryngeal swelling has receded. After thyrotomy or laryngofissure, all adductors (lateral, external and transverse muscles) are removed unilaterally or, if necessary, bilaterally in a submucous plane. Additionally the posterior wall of the cricoid lamina may also be split. Tracheotomy is always required. As with endolaryngeal lateral fixation. Dilator. General endotracheal anesthesia, re-intubation after preliminary tracheotomy. Incision. Midline skin incision, extending from the hyoid bone to the suprasternal notch, tracheotomy. Approach. Thyrotomy or, in the presence of a high-grade stenosis, laryngofissure with subsequent division of the cricoid lamina (laminotomy) (Fig. 10.14a). Arytenoidectomy. Curved incision from the medial tip of the arytenoid cartilage downward, circumventing below the vocal fold to the anterior commissure. The arytenoid cartilage is elevated with a small hook. Division of the capsule of the arytenoid joint. Release of the mucosa from the posterior margin of the arytenoid. Division of the transverse muscle. The incision is deepened along the vocal fold and the adductors removed, if necessary under the microscope (Fig. 10.14b). Wound closure. Mucosal suture; if appropriate, the same approach is repeated on the contralateral side. Stenosis secondary to scar formation requires a mucosal incision and a submucous resection of the scar tissue, followed by splitting of the posterior wall across the entire cricoid lamina in the midline from top to bottom, followed by lateral displacement. Fig. 10.14a, b Combined endo- and extralaryngeal lateral fixation after Rethi. a Mucosal incisions to remove the adductors. Auxiliary incision in the middle of the posterior wall to enable laminotomy. b The incision is spread open to remove the adductors. Spasmodic dysphonia, a form of pharyngeal dystonia, is a chronic neurological phenomenon characterized by action-induced spasms of the vocal folds. It usually presents as the adductor type, less often spasms of the abductor type are observed, and in some cases there is a combined adductor–abductor disturbance of function. Spasmodic dysphonia is nowadays preferably treated by the injection of botulinum toxin type A (Botox), either transoral and endoscopically controlled or transcutaneous and electromyographically controlled. Various studies have shown that this should be done unilaterally. It is known that patients who have been treated long-term and at short intervals with a high cumulative total dose develop antibodies against neurotoxins. In this case, conversion to neurotoxin type B (e. g., Neuro-Bloc) is indicated. Dose. Botox: 3.75 units/0.1 mL. For neurotoxin type B the equivalent dose must be verified individually by multiple injections. At the moment the literature recommends a dose between 250 MU and 1 250 MU of Neuro-Bloc. (An MU, or “mouse unit,” corresponds to the LD50 using Swiss-Webster mice.) Adductor spasmodic dysphonia. Verification of spastic dysphonia by magnifying laryngoscopy, fiberoptic endoscopy and videolaryngostroboscopy with the assessment of vocal performance and voice quality, together with the auditory evaluation of voice quality using electroacoustic methods in the form of a hoarseness diagram. High-pressure syringe (Order Nr. 771 400, High Pressure Syringe, K. Storz, Tuttlingen, Germany), butterfly needle (needle diameter 0.6 mm, 23 G). Topical anesthesia of the mucosa of the mouth, pharynx, and larynx using lidocaine spray. To reduce saliva flow and the urge to cough, an oral premedication of 0.5 mg atropine and 20 mg codeine is administered. Positioning. The transoral intralaryngeal injection technique is performed with the patient placed in a seated position. Transoral approach. First the level of the glottis is visualized endoscopically. After exposing the ventricularis and thyroarytenoid muscles, the injection is applied using a butterfly needle, causing only a small amount of tissue traumatization. The approach is usually unilateral. The injection may be applied transcutaneously under electromyographic guidance. This approach is less effective because the muscles are targeted less accurately. Current studies found in the literature indicate that unilateral injection is preferable to the bilateral approach. A single injection results in healing in 20 % of the patients; the remainder return for follow-up within the first 2 weeks postoperatively. If these patients have suffered no problems, an additional injection in the region of the contralateral side with 0.6–2.5 units/mL is indicated. About one-third of patients require the additional oral administration of clonazepam, trihexyphenidyl, or baclofen. A lateralization thyroplasty is indicated for recalcitrant cases. The time required to reach an optimal voice function is highly variable, both inter- and intra-individually. The onset of effect of the botulinum injection usually occurs after a latency of 2–8 days and the effect subsides after 3–6 months on average. The development of antibodies against botulinum toxin, anaphylaxis. The bilateral injection of botulinum toxin into the cricoarytenoid muscle can result in stridor. Therapy of stenosis of the larynx and trachea is highly varied, given the different locations and forms as well as the heterogeneous pathogenetic mechanisms. Congenital circumferential stenosis, especially if situated at a subglottic level, may initially be dilated with bougies. Repeated bougie dilation is possible. Web-like membrane formations in the anterior commissure (congenital or post-intubation) are incised using a microlaryngoscopic technique. Stenosis of the glottic aperture—post-traumatic, radiotherapeutic, or postoperative in origin—can often be managed with a supraglottic transverse laryngectomy. Long-segment stenosis in the larynx secondary to trauma, surgery, or intubation usually requires a laminotomy. Major plastic surgical measures are required for atresia or stenosis secondary to large defects. Circumferential subglottic web-like stenosis. First, the extent of the subglottic stenosis is assessed by laryngotracheoscopy. The extent of the often circumferential button-hole stenosis may be palpated with a small curved hook. Web-like stenoses with a thickness of a few millimeters are released using laser surgery by making a stellate incision, e. g., at 2 o’clock, 6 o’clock, and 10 o’clock positions. Full-thickness excision of the circumferential stenosis must be avoided at all costs. Such an approach will result in recurrent stenosis, leading in some cases to complete obstruction of the trachea. A functionally irrelevant residual stenosis often remains and usually does not require any further management. The combination of the botulinum toxin injection with postoperative voice therapy is strongly recommended. A laryngotracheoscopic follow-up examination should be performed, e. g., 6–8 weeks after the operation. Postoperative management following the release of a web formation in the region of the anterior commissure is a problem that still has not been solved definitively. One option is for the surgeon to remove the fibrin deposits from the commissure under local anesthesia using a curved instrument and indirect laryngoscopy, with the patient holding out the tongue. The interval between removal sessions should be decided according to each individual case. Another possibility is applying mitomycin C intraoperatively onto the wound surface after web release to reduce postoperative fibrin exudate. But not only does the efficacy of mitomycin C on the anterior commissure remain unexplained, but the question of whether the fibrin deposits should be removed at all remains unanswered. More conservatively orientated surgeons dispense with removing fibrin from the anterior commissure altogether, because they do not believe it to be worthwhile. This difference of opinion illustrates the difficulty that still exists with regard to postoperative management. See supraglottic transverse resection of the larynx, p. 248. Over the years stenosis in the region of the laryngotracheal junction has undergone a change in its varied ethiopathology. Thess stenoses used to be primarily congenital or of inflammatory origin, but nowadays they are usually iatrogenic, the result of complications secondary to long-term intubation or tracheotomy. The incidence of cicatricial stenosis of the laryngotracheal segment in newborns and infants has increased as a result of the growing number of intensive care measures performed in patients of this age group. One-half of all cases stenoses caused by long-term intubation are found in the region of the cricoid cartilage. Surgical treatment of these poses a significant challenge. Here laminotomy, described for the first time by Rethi as early as 1956, and its modifications, as well as partial resection of the cricoid cartilage with subsequent thyrotracheal anastomosis as reported by Persson et al. in 1975, has proved effective in a large number of cases. A clinically simple and commonly used grading system of subglottic stenosis originates from Myer. Grade I stenosis corresponds to an obstruction of 0–50 % of the lumen, grade II to an obstruction of 51–70 %, grade III to an obstruction of 71–99 %, and grade IV to complete obstruction of the lumen. Resection of the stenosis with division of the cricoid cartilage and insertion of a stent. Subglottic stenosis of the cricoid secondary to perichondritis, supraglottic stenosis, complete stenosis of the glottis, combined stenosis or atresia of the cricoid and the upper trachea. Microlaryngoscopy and tracheobronchoscopy for the exact assessment of the indication for stenosis surgery, CT diagnostic examination. Cartilage graft (rib, also the auricle in children), stent (e. g., Aboulker stent, or a tailored transparent stent, e. g., made of Plexiglas). General endotracheal anesthesia. Incision. The skin incision commences in the midline below the hyoid bone and continues to the upper border of the tracheostoma, where it proceeds in a semicircle around the upper border of the tracheostoma. Laminotomy. Division of the cricoid cartilage, and also if necessary the thyroid cartilage, in the midline using a scalpel. If the thyroid cartilage is significantly ossified, it may be divided with Killian scissors. Division of the posterior laryngeal wall. Corresponding to the approach for the anterior wall of the larynx, the posterior laryngeal wall is now opened, ensuring that the mucosa covering the external larynx wall, which already constitutes part of the hypopharynx, remains intact. The incision runs between the arytenoid cartilages, starting vertically in the midline and continuing downward past the level of the thyroid cartilage, 1–2 cm into the trachea. The lamina of the cricoid cartilage is now divided with a strong scalpel. If it is ossified, it should be carefully divided using primarily stab incisions. A Freer elevator is then used to verify that the cartilaginous wall has been completely divided. After this, two single hooks or two Rethi hooks are inserted to separate the two halves of the larynx. The transverse muscle is identified and resected. An autologous cartilage graft is then sutured between the incision margins of the cricoid lamina, making the width of the posterior wall gap ca. 1 mm per year of the patient’s age (rule of thumb for children). With regard to the use of this technique in children, it should be pointed out here that alternative procedures have increasingly won recognition, not least because of their long-term results. To avoid an open laryngotracheal groove, the laminotomy is often supplemented by a “stepped incision” as described by Evans and Todd. For this purpose, two caudally or cranially based mucosal flaps are elevated using microsurgical ear instruments to almost completely cover the surface of the expanded lumen as a pedicled U-flap. Then the stent is inserted into the larynx, coming to rest on the tracheotomy cannula and projecting slightly over the level of the vocal folds. Residual stenosis, perichondritis. Endoscopic follow-up of the stent: initially weekly, later 3- to 4-weekly. Operations purely for support (lateropexy, augmentation) are indicated for compression and collapse stenoses. Resection procedures (transverse laryngectomy, longitudinal split, open groove) must be chosen for stenoses secondary to scar formation and associated with loss of substance. Diaphragms and short stomal stenoses, i. e., those in the region of a tracheostoma, may be managed using laser surgery. The option of a stent implantation should also be considered. Stabilization of the tracheal wall, softened by pressure, by creating a muscle loop using the sternocleidomastoid muscle after prior resection of the compressing parts of the goitre or after scar revision. External compression of the trachea, in the region of the neck affecting breathing, by a goitre or scar with loss of cartilage elasticity but without scar formation involving tracheal cartilage or mucosa. As for a transverse resection of the trachea (see p. 210). Laryngotracheoscopy, thyroid scintigraphy, lateral and anterior–posterior spot films of the trachea (sucking–pressing), CT if appropriate (including 3D reconstruction). General endotracheal anesthesia. Incision with identification of the trachea. Kocher transverse collar incision, resection of compressing goitre nodes in typical fashion, resection of hypertrophic scars lateral to the trachea. Identification of the ventral tracheal cartilage. Release of the trachea. A tunnel is created on either side of the stenosis beneath the scar tissue attached to the lateral tracheal wall (Fig. 10.15a). Creation of the sternocleidomastoid muscle loops. Next, the sternal tendon of the sternocleidomastoid muscle is divided and the attachment released further proximally. The mobilized tendon is passed through and around the scar tunnel at the trachea and secured back to the clavicle or the clavicular head of the sternocleidomastoid. If it is not possible to draw the muscle through the scar tunnel, it may also be secured with several sutures to the lateral tracheal wall (Fig. 10.15b). Wound closure. Wound closure over a suction drain. Instead of stabilizing the trachea using a muscle sling, elastic material may be used for stabilization, placing it onto the trachea as a strut and securing it with a suture. Beware of the recurrent laryngeal nerve: when dissecting lateral and posterior to the trachea, spread the tissue only in the direction of the course of the nerve. For remarks on the course of the recurrent laryngeal nerve see page 285. If no tracheostoma is present, then tracheotomy as a rule is not essential. Fig. 10.15a, b Lateropexy. The trachea is supported by loops created from the sternal bellies of the sterno-cleidomastoid muscles which are passed through the lateral tunnels created within the scar tissue. Postoperative observation for possible respiratory failure; antibiotic; remove drain depending on amount collected. The part of the trachea contracted by scar formation is resected; the resulting gap is bridged by mobilizing the distal and proximal stumps and repaired with sutures. Cicatricial tracheal stenosis with a maximum length of 4–5 cm secondary to scar formation with loss of cartilaginous and mucosal coverage. Endoscopy, spot films of the trachea, CT diagnostic investigation. General endotracheal anesthesia, usually initially via an already present tracheostomy, followed by intraoperative re-intubation. Skin incision. Longitudinal midline incision, extending from the hyoid to the suprasternal notch, or large transverse Kocher collar incision. Exposure of the tracheal anterior wall of the larynx. Identification of the trachea. Skeletonization of the trachea; dissection is strictly along the lateral wall, spreading the tissue only in the direction of the course of the recurrent nerve. Resection of the stenosis. Transverse incision of the trachea at the caudal end of the stenosis, ensuring that the level of re-section is free of scar tissue. The distal stump of the trachea is secured with two lateral stay sutures. The narrowed segment is then carefully released from the anterior wall of the esophagus under protection of the recurrent nerve and resected back to healthy tissue (Fig. 10.16a). Mobilization of the trachea. To bridge longer defects, the trachea is mobilized in an inferior direction, down into the thoracic space (release is done only between sternum or esophagus and the trachea due to the lateral vascular supply). The straight prelaryngeal musculature and the thyrohyoid membrane are incised at the hyoid bone, allowing the larynx to be also moved downward. Fig. 10.16a, b Transverse tracheal resection with end-to-end anastomosis for cicatricial tracheal stenosis. a After resection of all scar tissue, a transverse incision is made through the strap muscles at the level of the hyoid bone (1) and the trachea is released between sternum and anterior tracheal wall (2) and between posterior tracheal wall and esophagus. b Suture repair of the tracheal stumps. Wound closure. In layers over a suction drain. Antibiotic, nasogastric tube, antitussive agent, 250 mg cortisone, anteflexion of the head. Longitudinal division of the anterior and posterior wall of the trachea with expansion (anteroposterior split widening), keeping it open with a stent or by insertion of a free spreading graft in the anterior and posterior wall. As for transverse resection of the trachea. As for transverse resection of the trachea. Prosthesis for tracheal stenting (e. g., Montgomery T-tube or Aboulker prosthesis). Skin incision and identification of the trachea. There is usually a tracheostoma already in place: if it is sited caudal to the stenosis, it is left untouched; if it is situated in the region of the stenosis, it is included in the incision. A midline skin incision is made over the narrowed tracheal segment, followed by skeletonization of the trachea beyond the stenosis. Compressing scars or a goitre are resected. Tracheotomy. Longitudinal division of the anterior wall of the trachea along the entire narrowed segment until normal tracheal tissue is reached (Fig. 10.17a
Endolaryngeal Operations
Indirect Endolaryngeal Operations
Surgical Principle
Indications
 Excisional biopsies.
Excisional biopsies.
 Excision of localized lesions of the vocal folds with the option of an intraoperative voice assessment.
Excision of localized lesions of the vocal folds with the option of an intraoperative voice assessment.
Contraindications
 Hyperactive gag reflex, poor visualization due to the anatomical situation.
Hyperactive gag reflex, poor visualization due to the anatomical situation.
 Lesions situated in the anterior commissure; extensive lesions (e. g., extensive Reinke edema and leukoplakia).
Lesions situated in the anterior commissure; extensive lesions (e. g., extensive Reinke edema and leukoplakia).
 Children under the age of 14 years.
Children under the age of 14 years.
 Allergy to topical anesthetics.
Allergy to topical anesthetics.
Special Instruments and Implants
Anesthesia
Surgical Technique
 Risks and Complications
Risks and Complications
 Hoarseness secondary to tissue defects, injury to the vocal fold (which may be caused by wrongly chosen and wrongly placed instruments or inadequate anesthesia), scarring of the vocal fold, web formation.
Hoarseness secondary to tissue defects, injury to the vocal fold (which may be caused by wrongly chosen and wrongly placed instruments or inadequate anesthesia), scarring of the vocal fold, web formation.
 Swelling of the larynx with subsequent dyspnea; tracheotomy may become necessary if a stenosis (secondary to a tumor or similar lesion) is already present.
Swelling of the larynx with subsequent dyspnea; tracheotomy may become necessary if a stenosis (secondary to a tumor or similar lesion) is already present.
 Recurrence.
Recurrence.
Postoperative Care
 Voice rest for 3–7 days, smoking and alcohol cessation.
Voice rest for 3–7 days, smoking and alcohol cessation.
 Oral intake 2 hours after completion of the operation at the earliest; inhalations; antitussive agents to suppress the urge to cough.
Oral intake 2 hours after completion of the operation at the earliest; inhalations; antitussive agents to suppress the urge to cough.
 If edema develops and/or a narrow glottis is present, observation under in-patient conditions; steroids if appropriate.
If edema develops and/or a narrow glottis is present, observation under in-patient conditions; steroids if appropriate.
Alternatives
Direct Endolaryngeal Operations
Direct Distending Laryngoscopy Under General Endotracheal Anesthesia (Microlaryngoscopy after Kleinsasser)
Surgical Principle
Indications
 Excisional biopsy, assessment of the extent of malignant lesions.
Excisional biopsy, assessment of the extent of malignant lesions.
 Excision of benign alterations, such as leukoplakia, hyperkeratosis, polyps, fibromas, papillomas, Reinke edema.
Excision of benign alterations, such as leukoplakia, hyperkeratosis, polyps, fibromas, papillomas, Reinke edema.
 Scar revision, resections of web formations and diaphragms.
Scar revision, resections of web formations and diaphragms.
 Reduction of arytenoid cartilage dislocations.
Reduction of arytenoid cartilage dislocations.
 Endolaryngeal arytenoidectomy; augmentation or lateralization of the vocal folds, glottic expansion.
Endolaryngeal arytenoidectomy; augmentation or lateralization of the vocal folds, glottic expansion.
 Endolaryngeal resection of laryngeal and hypopharyngeal carcinomas.
Endolaryngeal resection of laryngeal and hypopharyngeal carcinomas.
Contraindications
 General disorders that preclude general anesthesia.
General disorders that preclude general anesthesia.
 Anatomical alterations of the cervical spine, which prevent a (sufficient) reclination of the head (ankylosing spondylitis, fractures, extensive spinal osteochondrosis) or disk herniation in the region of the cervical spine, mandibular prognathism, significantly protruding upper teeth.
Anatomical alterations of the cervical spine, which prevent a (sufficient) reclination of the head (ankylosing spondylitis, fractures, extensive spinal osteochondrosis) or disk herniation in the region of the cervical spine, mandibular prognathism, significantly protruding upper teeth.
 Trismus.
Trismus.
 Larynx too narrow, exposure impossible.
Larynx too narrow, exposure impossible.
Specific Points Regarding Informed Consent
 Dental damage or even loss of teeth.
Dental damage or even loss of teeth.
 Mucosal injury.
Mucosal injury.
 Disturbances of swallowing (dysphagia), nasogastric tube.
Disturbances of swallowing (dysphagia), nasogastric tube.
 Hoarseness or even loss of voice.
Hoarseness or even loss of voice.
 Dyspnea, tracheotomy.
Dyspnea, tracheotomy.
 Pneumonia, atelectasis.
Pneumonia, atelectasis.
 Mediastinitis.
Mediastinitis.
 Pressure injury to the lingual, hypoglossal, or glossopharyngeal nerve, possibly causing loss of function.
Pressure injury to the lingual, hypoglossal, or glossopharyngeal nerve, possibly causing loss of function.
 Recurrence.
Recurrence.
Special Instruments and Implants
Anesthesia
Surgical Technique
 Rules, Tips, and Tricks
Rules, Tips, and Tricks
 Risks and Complications
Risks and Complications
 Dental damage (chipping of tooth enamel, fractures of the tooth neck or loosening of teeth, tooth extractions); mandibular joint problems secondary to hyperextension.
Dental damage (chipping of tooth enamel, fractures of the tooth neck or loosening of teeth, tooth extractions); mandibular joint problems secondary to hyperextension.
 Hematomas and abrasions in the region of the palatal arches, tonsils, and base of the tongue.
Hematomas and abrasions in the region of the palatal arches, tonsils, and base of the tongue.
 In extremely rare cases, dysfunction of the hypoglossal, lingual, or glossopharyngeal nerves secondary to pressure damage, resulting in disturbances of sensation, motion, and taste.
In extremely rare cases, dysfunction of the hypoglossal, lingual, or glossopharyngeal nerves secondary to pressure damage, resulting in disturbances of sensation, motion, and taste.
 Edema formation in the larynx, producing a risk of dyspnea in the presence of pre-existing stenosis.
Edema formation in the larynx, producing a risk of dyspnea in the presence of pre-existing stenosis.
 Hoarseness or increase of any pre-existing hoarseness, scar formation, and web formation with voice impairment.
Hoarseness or increase of any pre-existing hoarseness, scar formation, and web formation with voice impairment.
 Jet ventilation carries the risk of bursting an emphysematous bleb.
Jet ventilation carries the risk of bursting an emphysematous bleb.
Postoperative Care
 Voice rest, the duration of which depends on the endolaryngeal procedure being undertaken, consider voice therapy; daily inhalations may be indicated.
Voice rest, the duration of which depends on the endolaryngeal procedure being undertaken, consider voice therapy; daily inhalations may be indicated.
 Consider suppressing an irritated cough with antitussive agents and administering steroids to counteract the risk of edema.
Consider suppressing an irritated cough with antitussive agents and administering steroids to counteract the risk of edema.
Alternatives to Surgery Under Intubation
Direct Laryngotracheoscopy Using the Ventilation Laryngotracheoscope
Surgical Principle
Indications
 Direct laryngoscopy, incision biopsy, polypectomy, where narrow access or special anatomical conditions preclude intubation.
Direct laryngoscopy, incision biopsy, polypectomy, where narrow access or special anatomical conditions preclude intubation.
 Emergency endoscopy in the presence of intubation difficulties, laryngeal and tracheal tumors, laryngeal and tracheal injuries.
Emergency endoscopy in the presence of intubation difficulties, laryngeal and tracheal tumors, laryngeal and tracheal injuries.
Contraindications
Specific Points Regarding Informed Consent
Special Instruments and Implants
Anesthesia
Surgical Technique
 Rules, Tips, and Tricks
Rules, Tips, and Tricks
 Excisional biopsies, polypectomies, and similar procedures are done with long double-cup grasping forceps. The instruments are guided with the right hand by right-handed surgeons, while the left hand stabilizes the tube, which is then advanced back past the glottis, and ventilation is re-commenced. Hemostasis is achieved with a cotton bud soaked in naphazoline.
Excisional biopsies, polypectomies, and similar procedures are done with long double-cup grasping forceps. The instruments are guided with the right hand by right-handed surgeons, while the left hand stabilizes the tube, which is then advanced back past the glottis, and ventilation is re-commenced. Hemostasis is achieved with a cotton bud soaked in naphazoline.
 For difficult intubations: insert emergency tube into the trachea. Then advance a thin, well-lubricated bougie as far as the bifurcation and withdraw the tube. Then an intubation tube, which has been lubricated on its inner and outer surface, is threaded over the bougie and advanced into the larynx and trachea under digital guidance. The bougie is then withdrawn (Fig. 10.7).
For difficult intubations: insert emergency tube into the trachea. Then advance a thin, well-lubricated bougie as far as the bifurcation and withdraw the tube. Then an intubation tube, which has been lubricated on its inner and outer surface, is threaded over the bougie and advanced into the larynx and trachea under digital guidance. The bougie is then withdrawn (Fig. 10.7).
 For cases where identification of the laryngeal aperture is difficult due to edema, tumor, or trauma: once the pharynx has been well visualized with the aid of the laryngoscope blade, have firm pressure applied to the chest; the escaping air stream indicates the way to the glottis.
For cases where identification of the laryngeal aperture is difficult due to edema, tumor, or trauma: once the pharynx has been well visualized with the aid of the laryngoscope blade, have firm pressure applied to the chest; the escaping air stream indicates the way to the glottis.
 Always consider performing flexible fiberoptic intubation over a thin bronchoscope. This can be done via a transnasal route; however, the transoral route is preferable in an emergency situation. For this purpose, the tube is threaded over the flexible bronchoscope and secured with a tape at the transition to the handle, at that point where it can no longer be advanced further cranially. Then the intubation blade is inserted by an assistant, who pulls the right-hand corner of the mouth laterally. Now the person undertaking the intubation advances the bronchoscope over the tip of the intubation blade under direct vision as far as the epiglottis and then directs it under endoscopic guidance through the level of the glottis into the trachea as far as the bifurcation. Only now is the threaded tube advanced by the assistant, who maintains the position of the endoscope throughout the examination. After the tube has been placed, the endoscope is withdrawn.
Always consider performing flexible fiberoptic intubation over a thin bronchoscope. This can be done via a transnasal route; however, the transoral route is preferable in an emergency situation. For this purpose, the tube is threaded over the flexible bronchoscope and secured with a tape at the transition to the handle, at that point where it can no longer be advanced further cranially. Then the intubation blade is inserted by an assistant, who pulls the right-hand corner of the mouth laterally. Now the person undertaking the intubation advances the bronchoscope over the tip of the intubation blade under direct vision as far as the epiglottis and then directs it under endoscopic guidance through the level of the glottis into the trachea as far as the bifurcation. Only now is the threaded tube advanced by the assistant, who maintains the position of the endoscope throughout the examination. After the tube has been placed, the endoscope is withdrawn.
 Risks and Complications
Risks and Complications
 Dental damage or tooth loss, especially in the presence of preexisting dental damage or crowns.
Dental damage or tooth loss, especially in the presence of preexisting dental damage or crowns.
 Hoarseness or increase of any pre-existing hoarseness secondary to swelling, or even as a result of scar formation and web formation.
Hoarseness or increase of any pre-existing hoarseness secondary to swelling, or even as a result of scar formation and web formation.
 Laryngeal swelling with dyspnea, consider tracheotomy or intubation in the presence of pre-existing stenosis.
Laryngeal swelling with dyspnea, consider tracheotomy or intubation in the presence of pre-existing stenosis.
 Slipping and simultaneous brusque advancement of the telescope can, in exceptional cases, even result in hypopharyngeal perforation.
Slipping and simultaneous brusque advancement of the telescope can, in exceptional cases, even result in hypopharyngeal perforation.
Postoperative Care
 Antitussive agents against the urge to cough should already be given intraoperatively.
Antitussive agents against the urge to cough should already be given intraoperatively.
 With edema formation or in the presence of a narrow glottis: administer steroids before completion of the operation, postoperative observation.
With edema formation or in the presence of a narrow glottis: administer steroids before completion of the operation, postoperative observation.
 Voice rest, depending on the state of the larynx.
Voice rest, depending on the state of the larynx.
Transoral Cold-Steel Resection of Benign Lesions of the Larynx
Polyps of the Vocal Folds
Surgical Principle
Hyperkeratoses
Surgical Principle
Reinke Edema
Surgical Principle
 It should be emphasized that with Reinke edema, excision of the edema can be done bilaterally as long as the anterior commissure is not de-epithelialized. If the edema has extended as far as the anterior commissure, the contralateral side should not be approached during the same session, but completion of epithelialization should be awaited, 6–8 weeks later at the earliest.
It should be emphasized that with Reinke edema, excision of the edema can be done bilaterally as long as the anterior commissure is not de-epithelialized. If the edema has extended as far as the anterior commissure, the contralateral side should not be approached during the same session, but completion of epithelialization should be awaited, 6–8 weeks later at the earliest.
 Risks and Complications
Risks and Complications
Postoperative Care
Cysts
Surgical Principle
Indications
Contraindications
Surgical Technique
Laser Surgery
 Rules, Tips, and Tricks
Rules, Tips, and Tricks
Laryngeal Web
Surgical Technique
Postoperative Care
Alternatives
Incomplete Glottic Closure in the Presence of Unilateral Adductor Paralysis—Endolaryngeal Approach
Surgical Principle
Indications
Contraindications
Specific Points Regarding Informed Consent
Special Instruments
Surgical Technique
Augmentation
Open Approach
Surgical Principle
Indications
Contraindications
Specific Points Regarding Informed Consent
Special Instruments
Anesthesia
Surgical Technique
Friedrich Vocal Fold Medialization
 Rules, Tips, and Tricks
Rules, Tips, and Tricks
Postoperative Care
Alternatives
Transoral Laser Microsurgery
General Remarks
Special Instruments
Anesthesia
Benign Disorders
Granulomas
Indications
 The surgical removal of contact granulomas is indicated only in exceptional cases. Instead, speech therapy, in part supplemented by psychotherapy, forms the primary management modality. The possibility of reflux should be investigated.
The surgical removal of contact granulomas is indicated only in exceptional cases. Instead, speech therapy, in part supplemented by psychotherapy, forms the primary management modality. The possibility of reflux should be investigated.
 Intubation granulomas should not be excised earlier than 4 weeks after intubation. Exceptions are possible and include severe incidents of dyspnea or marked voice disorders.
Intubation granulomas should not be excised earlier than 4 weeks after intubation. Exceptions are possible and include severe incidents of dyspnea or marked voice disorders.
Anesthesia
Surgical Technique
 Rules, Tips, and Tricks
Rules, Tips, and Tricks
 Risks and Complications
Risks and Complications
Postoperative Care
Laryngocele
Surgical Principle
Indications
Specific Points Regarding Informed Consent
Surgical Technique
Papillomas
Surgical Principle
Indications
Specific Points Regarding Informed Consent
Anesthesia
Surgical Technique
 Rules, Tips, and Tricks
Rules, Tips, and Tricks
 Extubation is usually possible after surgery, even in very advanced cases.
Extubation is usually possible after surgery, even in very advanced cases.
 It has proved advantageous to maintain smaller areas of healthy mucosa between the individual papillomas to allow more rapid re-epithelialization of the endolarynx.
It has proved advantageous to maintain smaller areas of healthy mucosa between the individual papillomas to allow more rapid re-epithelialization of the endolarynx.
Postoperative Care
Alternatives
Laryngomalacia
Surgical Principle
Indications
Anesthesia
Surgical Technique
Membranous Laryngotracheal Stenosis
Laser Surgical Epiglottopexy
Surgical Technique
Laser Surgical Division of Short Aryepiglottic Folds
Surgical Technique
Hemangiomas and Vascular Malformations
Indications
 Subglottic hemangioma: progression in size with subsequent dyspnea and stridor.
Subglottic hemangioma: progression in size with subsequent dyspnea and stridor.
 Vascular malformations: progression in size with swallowing difficulties (dysphagia), disturbances of articulation, recurrent bleeding, recurrent infections, or dyspnea.
Vascular malformations: progression in size with swallowing difficulties (dysphagia), disturbances of articulation, recurrent bleeding, recurrent infections, or dyspnea.
Contraindications
Anesthesia
Surgical Technique
Subglottic Hemangiomas
Vascular Malformations
 Rules, Tips, and Tricks
Rules, Tips, and Tricks
 Risks and Complications
Risks and Complications
Postoperative Care
 Careful monitoring of the patient’s respiratory condition in order to counteract immediately any postoperative edema formation by the administration of steroids.
Careful monitoring of the patient’s respiratory condition in order to counteract immediately any postoperative edema formation by the administration of steroids.
Surgery for Glottic Stenosis
 Endo-extralaryngeal expansion of the glottis (e. g., after Lichtenberger).
Endo-extralaryngeal expansion of the glottis (e. g., after Lichtenberger).
 Endolaryngeal microlaryngoscopic glottic expansion.
Endolaryngeal microlaryngoscopic glottic expansion.
 Extralaryngeal laterofixation.
Extralaryngeal laterofixation.
 Combined extra-endolaryngeal approach after thyrotomy.
Combined extra-endolaryngeal approach after thyrotomy.
Lichtenberger Endo-Extralaryngeal Expansion of the Glottis
Surgical Principle
Indications
 Fresh bilateral paralysis of the recurrent laryngeal nerve.
Fresh bilateral paralysis of the recurrent laryngeal nerve.
 Inhalation with β-sympathomimetic agents and steroids.
Inhalation with β-sympathomimetic agents and steroids.
 Oral and, if necessary, antibiotic therapy with a cephalosporin.
Oral and, if necessary, antibiotic therapy with a cephalosporin.
Contraindications
Specific Points Regarding Informed Consent
Special Instruments and Implants
Anesthesia
Surgical Technique
 Rules, Tips, and Tricks
Rules, Tips, and Tricks
 Risks and Complications
Risks and Complications
Postoperative Care
Endolaryngeal, Microlaryngoscopic Expansion of the Glottis
Surgical Principle
Indications
Contraindications
Specific Points Regarding Informed Consent
 As for microlaryngoscopy.
As for microlaryngoscopy.
 As for laser surgery of laryngeal tumors, the operation cannot reproduce normal findings; compromise between loss of voice and improvement in breathing; tracheotomy is often required with the conventional approach.
As for laser surgery of laryngeal tumors, the operation cannot reproduce normal findings; compromise between loss of voice and improvement in breathing; tracheotomy is often required with the conventional approach.
Special Instruments
Surgical Technique
Transoral Arytenoidectomy
Endolaryngeal Laser Surgical Expansion of the Glottis After Dennis and Kashima (Posterior Cordectomy)
Surgical Principle
Surgical Technique
Modifications
Postoperative Care
 Extubation after a single-dose administration of a steroid (e. g., 250 mg prednisolone IV); a tracheotomy is not necessary.
Extubation after a single-dose administration of a steroid (e. g., 250 mg prednisolone IV); a tracheotomy is not necessary.
 Antibiotic coverage for 3 days.
Antibiotic coverage for 3 days.
 Revision surgery may be necessary to remove fibrin deposits and/or granulations, which can narrow the glottis.
Revision surgery may be necessary to remove fibrin deposits and/or granulations, which can narrow the glottis.
Extralaryngeal Lateral Fixation
Surgical Principle
Anesthesia
Surgical Technique
Modifications
 Risks and Complications
Risks and Complications
 Postoperative bleeding, formation of hematoma, or persisting edema with persistent glottic stenosis.
Postoperative bleeding, formation of hematoma, or persisting edema with persistent glottic stenosis.
 Dehiscence of the vocalis suture, perichondritis of the laryngeal framework.
Dehiscence of the vocalis suture, perichondritis of the laryngeal framework.
 Injury to the hypopharyngeal mucosa with fistula formation (surgical revision with coverage, release of the lower horizontal fibers of the inferior pharyngeal constrictor muscle).
Injury to the hypopharyngeal mucosa with fistula formation (surgical revision with coverage, release of the lower horizontal fibers of the inferior pharyngeal constrictor muscle).
 Hoarseness (inevitable), aphonia secondary to exaggerated lateral fixation.
Hoarseness (inevitable), aphonia secondary to exaggerated lateral fixation.
 Tracheal stenosis secondary to tracheotomy.
Tracheal stenosis secondary to tracheotomy.
Postoperative Care
Combined Extra-Endolaryngeal Expansion of the Glottis
Surgical Principle
Indications
 Recurrences following laterofixation.
Recurrences following laterofixation.
 Narrow glottis secondary to bilateral paralysis of the recurrent laryngeal nerve in addition to a laryngeal stenosis secondary to scar tissue formation.
Narrow glottis secondary to bilateral paralysis of the recurrent laryngeal nerve in addition to a laryngeal stenosis secondary to scar tissue formation.
 Traumatic or postoperative laryngeal stenosis.
Traumatic or postoperative laryngeal stenosis.
Contraindications
Special Instruments and Implants
Anesthesia
Surgical Technique
 Risks and Complications
Risks and Complications
 Risk of perichondritis, edema formation, pressure ulcers in the larynx or trachea, formation of granulation tissue, later scar formation with recurrent stenosis in the region of the larynx or trachea.
Risk of perichondritis, edema formation, pressure ulcers in the larynx or trachea, formation of granulation tissue, later scar formation with recurrent stenosis in the region of the larynx or trachea.
 Massive deterioration in voice quality, often aphonic.
Massive deterioration in voice quality, often aphonic.
Postoperative Care
 Antibiotic coverage.
Antibiotic coverage.
 Dilator must be left for several months.
Dilator must be left for several months.
Spasmodic Dysphonia
Surgical Principle
Indications
Specific Points Regarding Informed Consent
 As for microlaryngoscopy.
As for microlaryngoscopy.
 Anaphylactic shock.
Anaphylactic shock.
 Multiple injections.
Multiple injections.
Operative Planning
Special Instruments
Anesthesia
Surgical Technique
Modification
 Rules, Tips, and Tricks
Rules, Tips, and Tricks
Surgery for Stenosis of the Larynx and Trachea
Approach for Laryngeal Stenosis
Surgical Principle
 Rules, Tips, and Tricks
Rules, Tips, and Tricks
 Risks and Complications
Risks and Complications
Postoperative Care
Postoperative Care
Web Formation in the Region of the Anterior Commissure
Stenosis of the Proximal Larynx
Stenosis of the Laryngotracheal Junction
Resection
Surgical Principle
Indications
Specific Points Regarding Informed Consent
 Complications as for microlaryngoscopy, skin incision over the thyroid cartilage, stent placement, wound infection and wound breakdown, sensitivity, paralysis of the lingual nerve, dyspnea, tracheotomy.
Complications as for microlaryngoscopy, skin incision over the thyroid cartilage, stent placement, wound infection and wound breakdown, sensitivity, paralysis of the lingual nerve, dyspnea, tracheotomy.
 Placement of a stent for several months, repeated endoscopic follow-up examinations.
Placement of a stent for several months, repeated endoscopic follow-up examinations.
Operative Planning
Special Instruments and Implants
Anesthesia
Surgical Technique
 Scar tissue should not be removed from the inner lateral wall of the larynx, to prevent the recurrent formation of wound surfaces and subsequent scar formation.
Scar tissue should not be removed from the inner lateral wall of the larynx, to prevent the recurrent formation of wound surfaces and subsequent scar formation.
 Rules, Tips, and Tricks
Rules, Tips, and Tricks
 Retention time of the stent should not be less than 2 months, if possible, as otherwise shrinkage and subsequent narrowing of the lumen is to be expected.
Retention time of the stent should not be less than 2 months, if possible, as otherwise shrinkage and subsequent narrowing of the lumen is to be expected.
 It is imperative for the success of the operation to regularly check the position of the stent, initially every week.
It is imperative for the success of the operation to regularly check the position of the stent, initially every week.
 Risks and Complications
Risks and Complications
Postoperative Care
Management of Tracheal Stenosis
Lateropexy of the Trachea
Surgical Principle
Indications
Contraindications
 Severe underlying general condition.
Severe underlying general condition.
 Scarring of the mucosa or cartilage defects secondary to scar formation; intrathoracic development of a compression stenosis.
Scarring of the mucosa or cartilage defects secondary to scar formation; intrathoracic development of a compression stenosis.
Specific Points Regarding Informed Consent
Operative Planning
Anesthesia
Surgical Technique
Modification
 Rules, Tips, and Tricks
Rules, Tips, and Tricks
 Risks and Complications
Risks and Complications
 Recurrent collapse of the trachea associated with stridor.
Recurrent collapse of the trachea associated with stridor.
 Unilateral or bilateral injury to the recurrent nerve.
Unilateral or bilateral injury to the recurrent nerve.
 Postoperative bleeding with renewed compression of the trachea.
Postoperative bleeding with renewed compression of the trachea.
 Perichondritis of the tracheal cartilage.
Perichondritis of the tracheal cartilage.
 Mediastinitis, pneumothorax, injury to major intrathoracic vessels.
Mediastinitis, pneumothorax, injury to major intrathoracic vessels.
Postoperative Care
Transverse Tracheal Resection with End-to-End Anastomosis
Surgical Principle
Indications
Contraindications
 Length of stenosis—usually more than 5 cm.
Length of stenosis—usually more than 5 cm.
 Deep thoracic stenosis (not accessible via a collar incision).
Deep thoracic stenosis (not accessible via a collar incision).
 Stenosis at the cricotracheal junction (after resection of the cricoid there is a problematic difference of calibre between the lumen at the inferior border of the thyroid cartilage and that of the trachea, thus posing a relative contraindication).
Stenosis at the cricotracheal junction (after resection of the cricoid there is a problematic difference of calibre between the lumen at the inferior border of the thyroid cartilage and that of the trachea, thus posing a relative contraindication).
Specific Points Regarding Informed Consent
 Long-term mechanical ventilation.
Long-term mechanical ventilation.
 Suture tear-out with dislocation or slippage of the trachea into the thorax.
Suture tear-out with dislocation or slippage of the trachea into the thorax.
 Poor healing of the skin margins.
Poor healing of the skin margins.
 Cicatricial stenosis of the trachea, tracheitis.
Cicatricial stenosis of the trachea, tracheitis.
 Hoarseness, loss of voice, paralysis of the vocal fold nerve.
Hoarseness, loss of voice, paralysis of the vocal fold nerve.
 Difficulty with swallowing (dysphagia), insertion of a nasogastric tube.
Difficulty with swallowing (dysphagia), insertion of a nasogastric tube.
 Possible tracheotomy with insertion of a tracheotomy tube.
Possible tracheotomy with insertion of a tracheotomy tube.
 Possible extension of the operation, thoracotomy.
Possible extension of the operation, thoracotomy.
 Pneumonia.
Pneumonia.
 Pneumothorax, insertion of a chest drain.
Pneumothorax, insertion of a chest drain.
 Hemorrhage/surgical emphysema of the mediastinum with mediastinitis.
Hemorrhage/surgical emphysema of the mediastinum with mediastinitis.
 Chondritis.
Chondritis.
Operative Planning
Anesthesia
Surgical Technique
 Rules, Tips, and Tricks
Rules, Tips, and Tricks
 Bring the head into anteflexion before tying the knots (Fig. 10.16b).
Bring the head into anteflexion before tying the knots (Fig. 10.16b).
 The tracheostoma is included in the incision if there is a stenosis in the region of the tracheostoma. Intubation is performed via the tracheostoma; after the incision re-intubation is from a cranial approach by threading the tracheal stumps over the tube. Alternatively, a new tracheostoma may be created caudal to the anastomosis.
The tracheostoma is included in the incision if there is a stenosis in the region of the tracheostoma. Intubation is performed via the tracheostoma; after the incision re-intubation is from a cranial approach by threading the tracheal stumps over the tube. Alternatively, a new tracheostoma may be created caudal to the anastomosis.
 Strict anteflexion of the head should be observed during the postoperative observation period. With very extensive segment resections, some surgeons recommend maintaining the head in anteflexion by applying a head–thorax cast or suturing the suprasternal notch to the tip of the chin to reduce tension on the suture line.
Strict anteflexion of the head should be observed during the postoperative observation period. With very extensive segment resections, some surgeons recommend maintaining the head in anteflexion by applying a head–thorax cast or suturing the suprasternal notch to the tip of the chin to reduce tension on the suture line.
 Risks and Complications
Risks and Complications
 Suture-line dehiscence, residual stenosis associated with stridor.
Suture-line dehiscence, residual stenosis associated with stridor.
 Injury to the recurrent nerve, pleural injury.
Injury to the recurrent nerve, pleural injury.
 Mediastinitis.
Mediastinitis.
 Vascular injury, bleeding from vascular erosion in the presence of a deep tracheostoma.
Vascular injury, bleeding from vascular erosion in the presence of a deep tracheostoma.
Postoperative Care
Longitudinal Division of the Trachea
Surgical Principle
Indications
 Extensive cicatricial stenosis of the cervical trachea (with an extent of >5 cm).
Extensive cicatricial stenosis of the cervical trachea (with an extent of >5 cm).
 Stenosis at the cricotracheal junction.
Stenosis at the cricotracheal junction.
Contraindications
 Severe underlying general disorder.
Severe underlying general disorder.
 Inoperable coexisting laryngeal stenosis.
Inoperable coexisting laryngeal stenosis.
 Extension of the stenosis into the thorax.
Extension of the stenosis into the thorax.
Specific Points Regarding Informed Consent
Operative Planning
Special Instruments and Implants
Surgical Technique
![]()
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


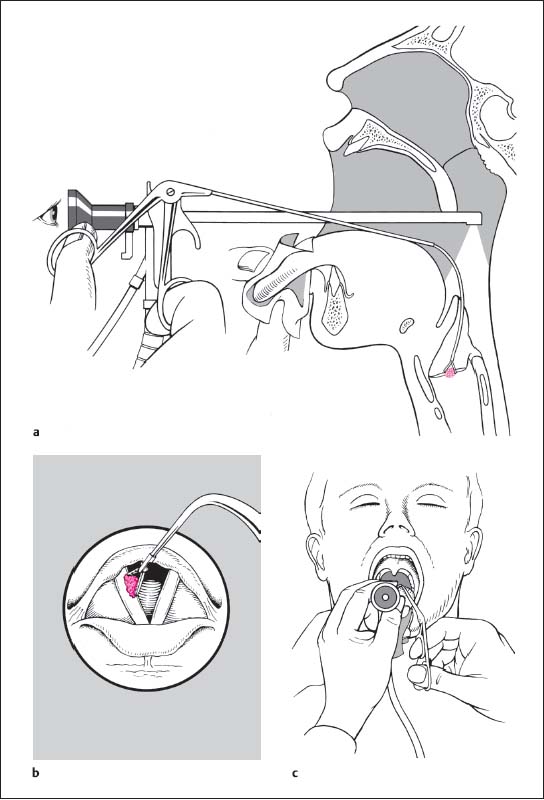
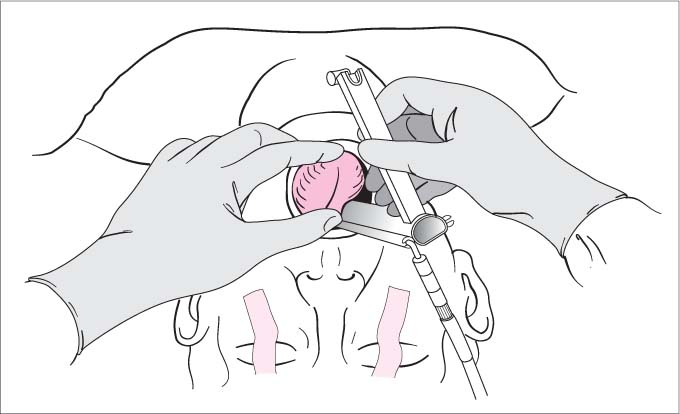
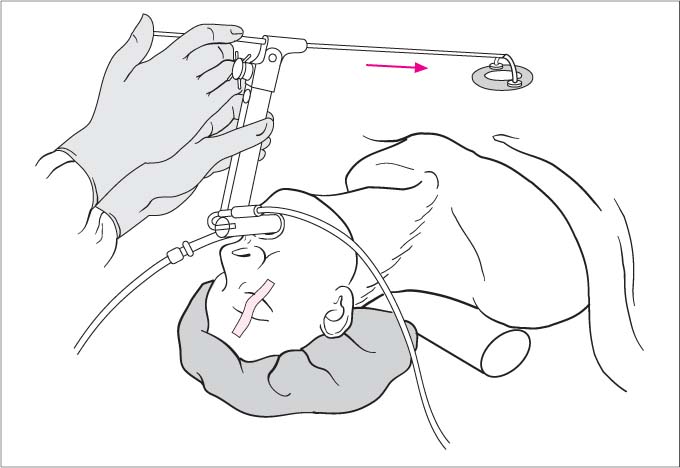
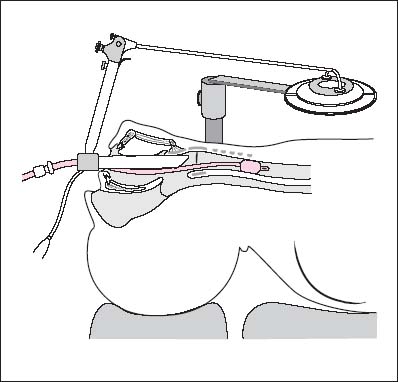
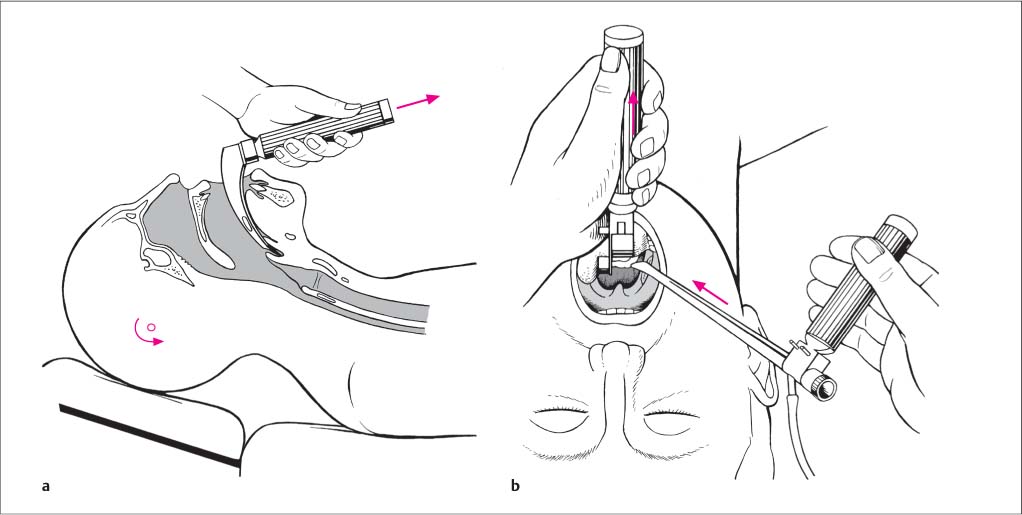
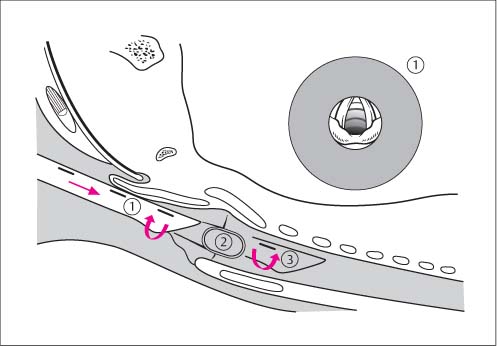
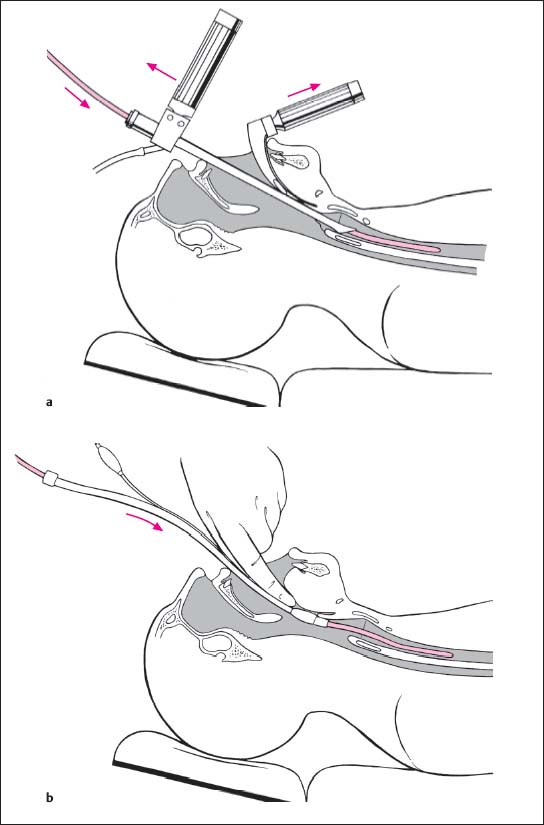
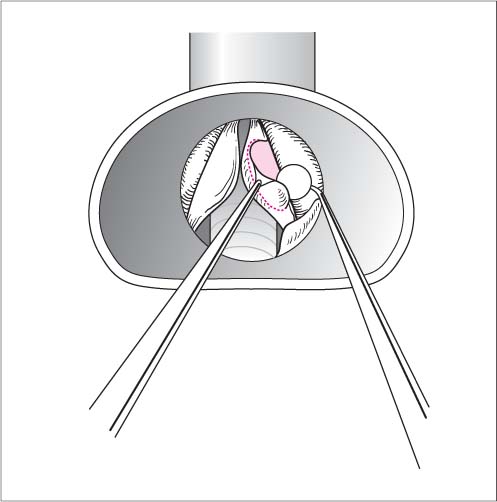
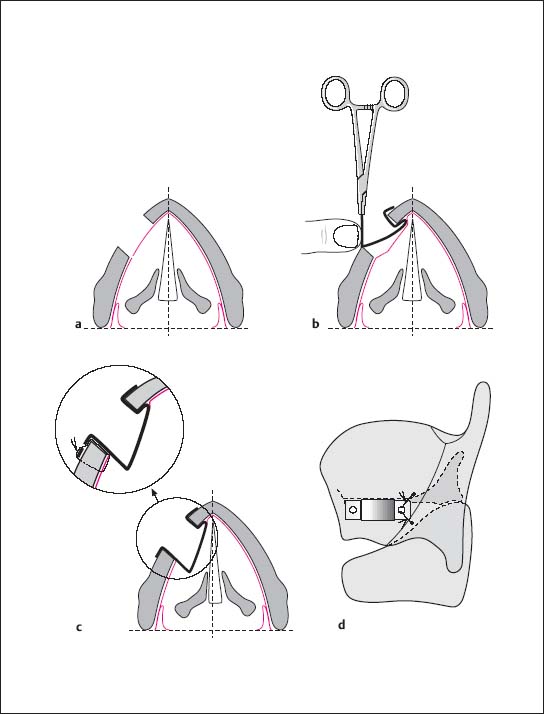
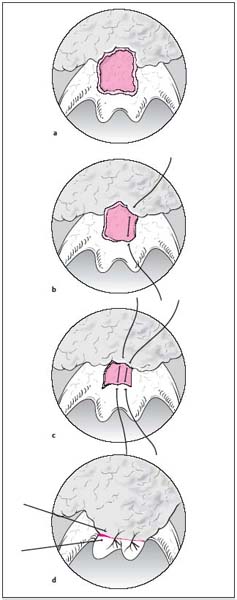
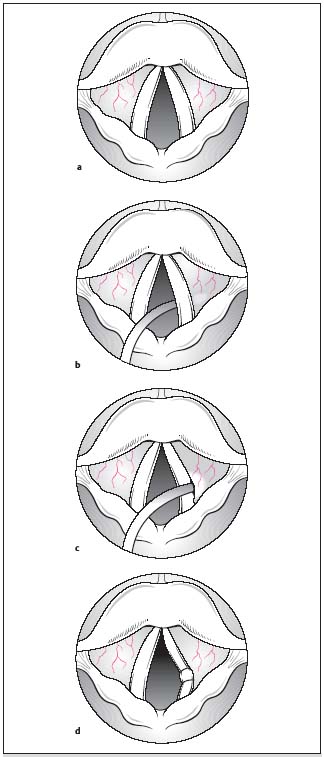
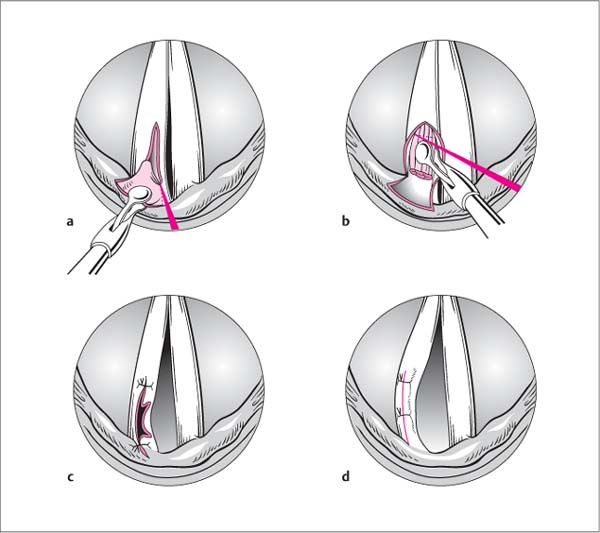
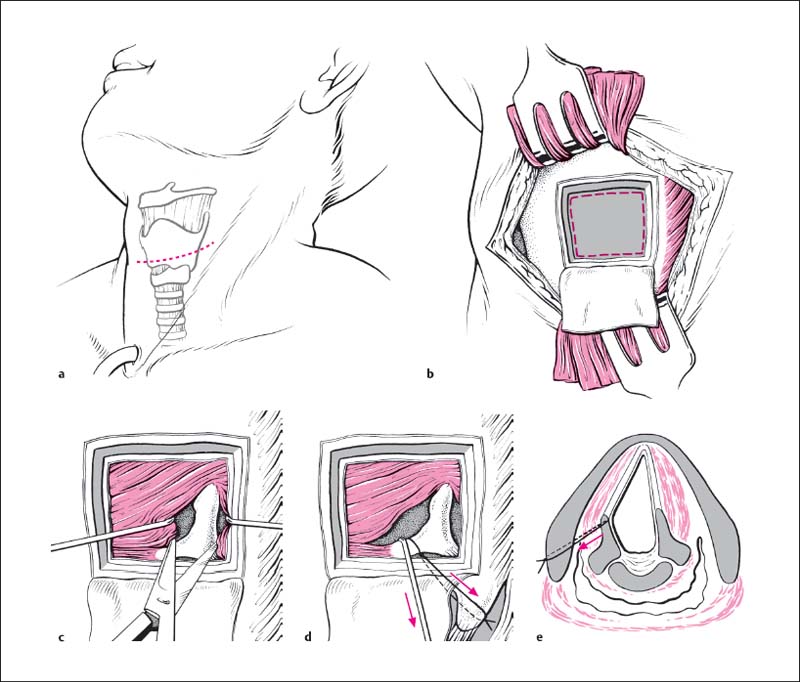
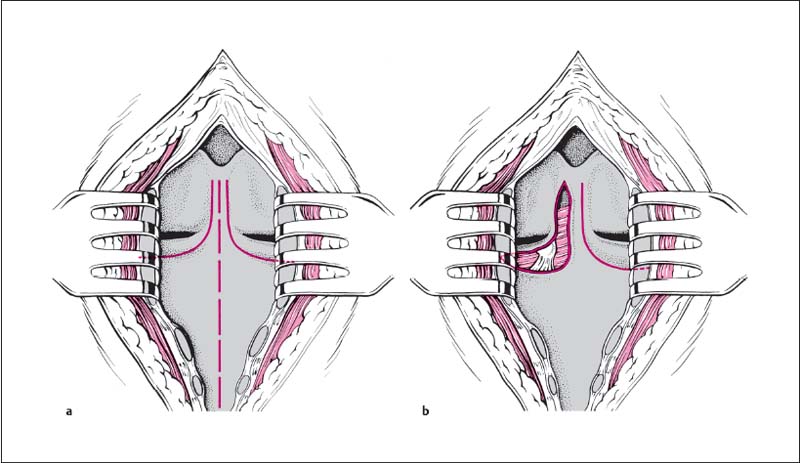
 Risks and Complications
Risks and Complications