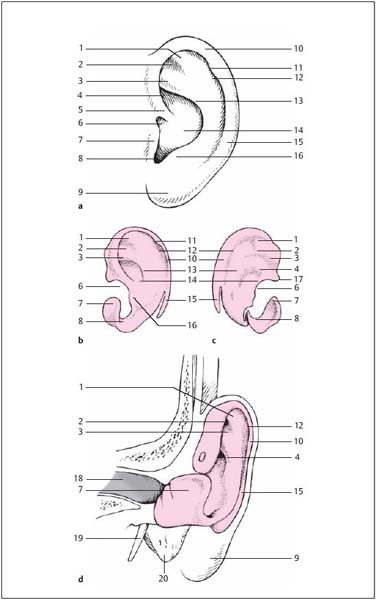
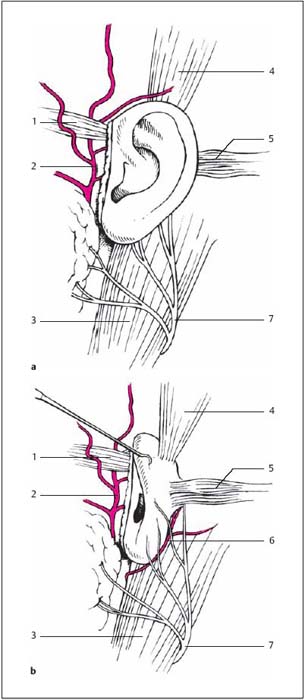
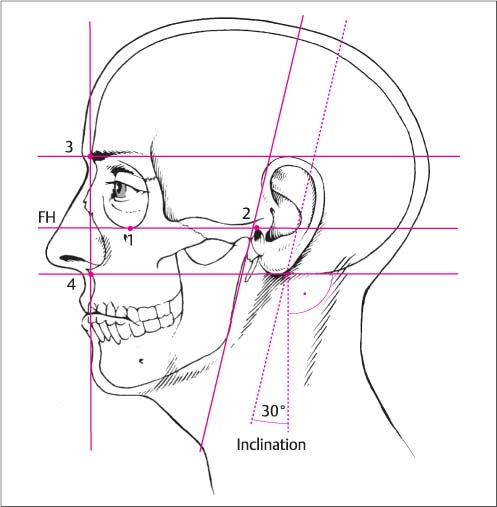
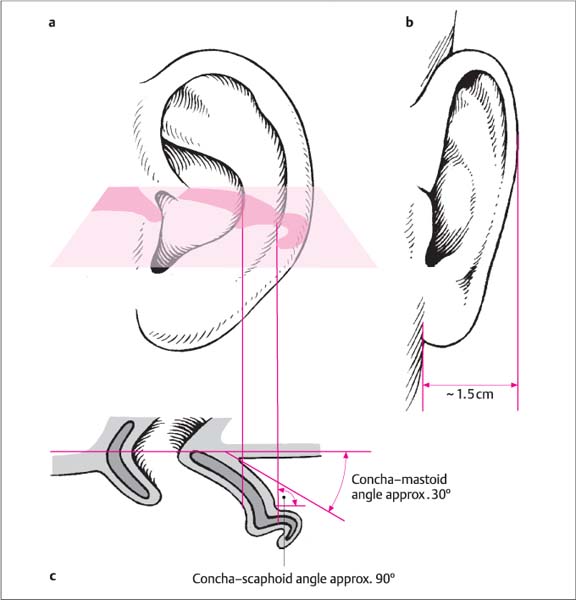
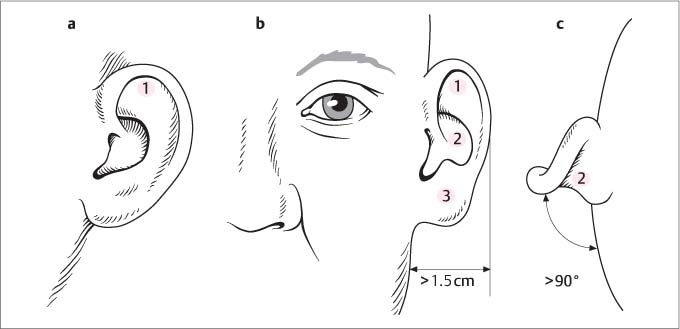
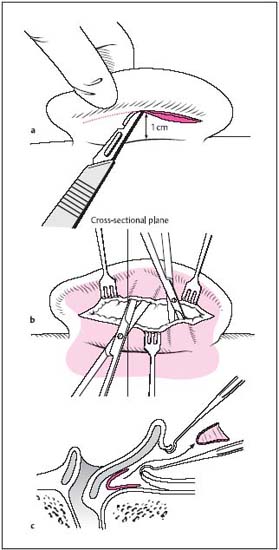
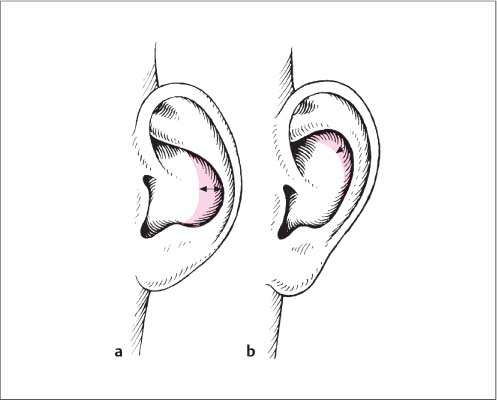
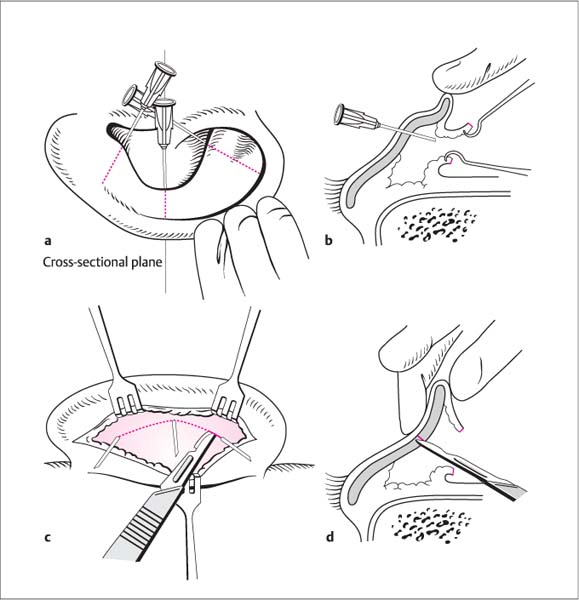
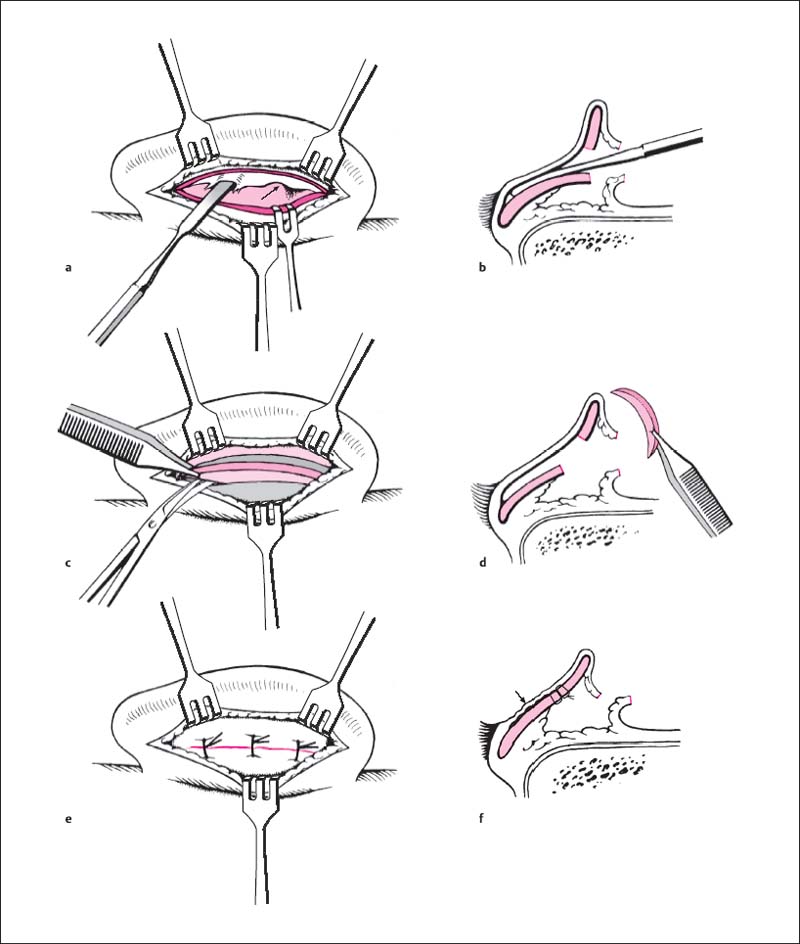
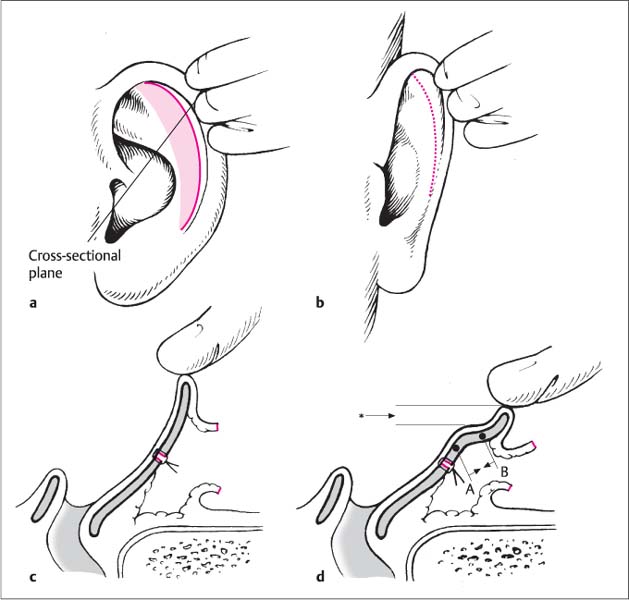
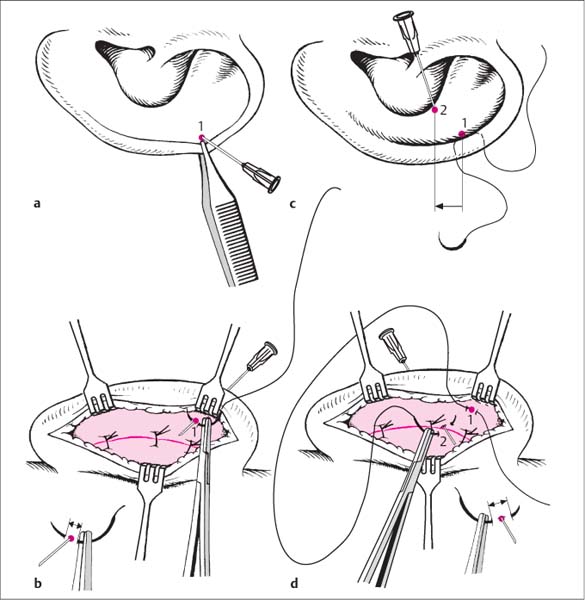
15 Surgery of the Auricle and Ear Canal The auricle, or pinna, develops from the fusion of six auricular hillocks of the first and second branchial arches (mandibular and hyoid arches). The ear canal derives from the first bran-chial cleft located between the arches. The range of variation of auricular shapes and deformities can be attributed to growth abnormalities or a failure of fusion of the auricular hillocks. A well-known example of an anatomic variant is the auricular tubercle, known also as Darwin’s tubercle, which corresponds to the point of the ear in mammals. The external ear consists of the auricle, the external ear canal (external auditory canal, external acoustic meatus), and the lateral surface of the tympanic membrane. The lateral contours of the ear are defined by prominences (eminences) and depressions (fossae) in the elastic auricular cartilage, which is directly apposed to the outer skin with no intervening fat. Only the earlobe and the free auricular border posterosuperior to the earlobe are formed by a noncartilaginous skin duplication that contains connective tissue and fat. Because there is no subcutaneous tissue layer, the anterior skin of the auricle is almost immovable relative to the perichondrium, which makes the auricle highly vulnerable to tangential trauma. This contrasts with the posterior side of the auricle, especially near the auricular root, which has a thick layer of subcutaneous fat. The lateral aspect of a normally shaped auricle presents typical surface features (Fig. 15.1a–d). The rim of the auricle, called the helix, forms a laterally curled ridge that terminates inferiorly in the tail of the helix, which is continuous with the earlobe (lobule). The helical skin widens anteriorly and blends with the skin over the zygomatic arch, while the tip of the helix curves downward and backward to terminate as the helical crus. Anterior and parallel to the helix is the antihelix, which divides superiorly into two crura (anterior and posterior). The depression between the crura is the triangular fossa. The variable depression between the helix and antihelix is called the scapha (scaphoid fossa). The external ear canal is covered anteriorly by the tragus. Opposite to the tragus, and separated from it by the intertragic notch, is the antitragus, which forms a tubercle at the inferior root of the antihelix. The deep central cavity of the auricle is the concha. The helical crus, which features a sharp anterior protrusion (the helical spine), divides the concha into the cymba conchae (between the anterior crus of the antihelix and the helical crus) and the conchal cavity, which is the actual vestibule leading to the external ear canal. The acoustic meatus, then, is framed by the cartilage of the conchal cavity, by the tragus anteriorly, and by the helical crus superiorly. Between the tragus and helical crus is a cartilage-free space (anterior notch) covered only by connective tissue and muscle (superficial: auricularis anterior muscle; deep: temporalis muscle). This makes it a useful site for an “endaural auxiliary incision” to enlarge the meatal opening. The auricular cartilage basically defines the surface anatomy of the auricle (Fig. 15.1b, d) except for the earlobe, the cartilage-free gap between the antitragus and helical tail, and the anterior notch. The medial (posterior) surface of the auricular cartilage (Fig. 15.1c) forms a less prominently developed “negative” of the lateral surface contours (Fig. 15.1b). The variable anterior and posterior surface anatomy of the auricle can hamper anatomical orientation in surgical procedures, which are most commonly performed on the medial (“posterior”) cartilage surface to modify the shape of the lateral (“anterior”) surface. Thus, characteristic depressions in the lateral surface of the auricle (triangular fossa, auricular concha, scapha) correspond to prominences (eminences) on the medial surface. Conversely, prominences in the lateral surface (helical crus, antihelix) correspond to depressions (fossae) in the medial cartilage surface. These prominences and depressions can be difficult to identify during posterior dissection of the auricle because they are compensated by the variable thickness of the auricular cartilage and because depressions are bridged by connective tissue or even muscle (between the concha and scapha). The anterior auricular surface presents conspicuous surface features while the posterior surface is mostly featureless. As a result, corresponding points on the anterior and posterior surfaces can be positively identified only by piercing the auricle with marking needles. Fig. 15.1a–d Infrastructure of the auricle and ear canal (left side). a Auricular surface anatomy, lateral view. b Cartilaginous framework, anterior view. c Cartilaginous framework, posterior view. d Coronal section through the auricle and ear canal. 1 Posterior crus of antihelix 2 Triangular fossa 3 Anterior crus of antihelix 4 Cymba conchae 5 Crus of helix 6 Anterior notch 7 Tragus 8 Intertragic notch 9 Earlobe (lobule) 10 Helix 11 Darwin tubercle 12 Scapha 13 Antihelix 14 Conchal cavity 15 Tail of helix 16 Antitragus 17 Spine of helix 18 Ear canal 19 Styloid process 20 Mastoid tip The posterior auricular skin is relatively smooth and forms an angle only between the scapha and concha (scaphoconchal angle). The fold located at the junction with the mastoid skin is called the postauricular sulcus. The normal surface area of the posterior auricular skin is considerably smaller than on the anterior side because the anterior surface presents conspicuous surface features and because fibrofatty tissue and the auricularis posterior muscle occupy the angle between the concha and mastoid (Fig. 15.2a, b). Nevertheless, redundant skin is usually present on the posterior side of the auricle in patients with prominent ears. The ear canal (Fig. 15.1d) consists of a medial bony part, which occupies approximately one-third of its total length, and a lateral cartilaginous framework. The floor and sidewalls of the bony ear canal are formed by the tympanic part of the temporal bone, the roof by the squamous part. The meatal cartilage is not a closed tube but forms a trough that is open posteriorly and superiorly and has additional gaps in its floor. These cartilage-free gaps are covered by connective tissue, which completes the tubular shape of the cartilaginous canal. Fig. 15.2a, b Muscles, nerves, and blood vessels of the auricle (left side). a Lateral view. b Posterior view. 1 Auricularis anterior muscle 2 Superficial temporalis muscle 3 Sternocleidomastoid muscle 4 Auricularis superior muscle 5 Auricularis posterior muscle 6 Posterior auricular artery 7 Greater auricular nerve The tragus is the direct lateral continuation of the meatal cartilage, which is connected to the auricle itself only at its inferior end (intertragic notch). Because the tympanic membrane is at an oblique angle relative to the long axis of the ear canal, the anterior wall of the ear canal is longer (approx. 26 mm) than the posterior wall (approx. 21 mm). The auricular skin is continuous with the skin lining the ear canal. It is very thin in the bony ear canal, adherent to the periosteum, and covers the lateral surface of the tympanic membrane. The skin at the meatal opening contains hairs with sebaceous glands and cerumen glands (specialized sweat glands) whose pigments are responsible for the brown coloration of the cerumen. The auricle, like all openings in the face, is surrounded by muscles that are classified as mimetic muscles and are supplied by the facial nerve (Fig. 15.2a, b). They have no functional significance but may have to be exposed and, if necessary, divided or resected in some surgical procedures. They are interconnected by the galea aponeurotica to form a muscular system. The galea is a tendinous expansion beneath the scalp that stretches between the occipitalis and frontalis muscles. A mobile tissue plane, the subaponeurotic layer, separates the galea from the periosteum of the cranial vault (pericranium). The muscles converge toward the auricular cartilage in a stellate pattern from the posterior, superior and anterior sides. The auricularis anterior muscle inserts on the helical spine. The auricular skin derives most of its sensory innervation from the great auricular nerve. This main branch of the cervical plexus becomes superficial at the posterior border of the sternocleidomastoid muscle (punctum nervosum), descends on the muscle, and divides into an anterior and posterior branch. Smaller branches from the vagus nerve and auriculotemporal nerve (branch of the mandibular nerve) supply portions of the anterior auricular surface, the ear canal, and the temporal skin. The auricle receives its blood supply from the posterior auricular artery (branch of the occipital artery) and from the superficial temporal artery (superficial terminal branch of the external carotid artery). The vascular network is so rich that even small tissue bridges left by trauma to the ear are sufficient to maintain adequate blood flow to the auricle. The arterial blood supply is compromised less by superior tears than by inferior tears. The auricle is generally evaluated with respect to its size, position, and shape. The size of a normal auricle from the superior helical rim to the earlobe (Fig. 15.3) is approximately equal to the distance from the glabella (at the level of the eyebrows) to the subnasale (junction of the columella and upper lip). Macrotia refers to an auricle that significantly exceeds that size. Often this condition affects only the superior third (scapha) or inferior third (lobule) of the auricle. An abnormally small auricle (microtia) can have a variety of presentations ranging from excessive overhang of the upper helix (“cup ear”) to a rudimentary auricle. Pronounced forms are associated with meatal atresia. The position of the auricle relative to the head is evaluated from the anterior, lateral, and superior aspects (see Fig. 15.6). When the head is viewed in profile (Fig. 15.3), the longitudinal axis of the auricle forms a ca. 30° angle to a perpendicular line through the Frankfurt horizontal (imaginary line connecting the infraorbital rim to the roof of the ear canal). Thus it is roughly parallel to the vertical ramus of the mandible. When viewed from the front (Fig. 15.4b), the antihelix and helix should be at approximately the same level or the helix should be just outside the antihelix. The auricle is described as “prominent” if the helix is conspicuously visible from the front and projects more than 1.5 cm from the mastoid plane. These relationships are described by two angles that are measured in the superior view (Fig. 15.4c). The angle between the concha and scapha behind the ear should be ca. 90°. If the angle is greater than 90 °, the antihelical fold is absent and the helix is protuberant. If the angle is less than 90°, the helix is curled medially and is hidden by the antihelix when viewed from the front. The relationship of the auricle to the skull is described by the concha–mastoid angle (cephaloauricular angle). The cross-sectional axes of the auricle and mastoid normally form a ca. 30° angle. Analysis of the auricular shape in the lateral view should include at least four structures (Fig. 15.4a): Otoplasty to correct an auricular deformity should create normal anatomical relationships whenever possible. It is important to avoid overcorrection in the form of flat (“pinned back”) ears or a helical rim that is not visible from the front. When findings have been described according to this scheme, preoperative photographic documentation is strongly recommended. The forehead and chin should be visible in photographs taken from the front and side. The workup should include an occipital view to document auricular position and full-frame lateral photographs of the auricles to document surface anatomy. Clips should be used to hold back the hair, if necessary. Fig. 15.3 Anatomical relations of the auricle. FH = Frankfurt horizontal through the infraorbital rim (1) and roof of the ear canal (2). The longitudinal axis of the auricle runs at an angle of ca. 30° (inclination) to the frontal plane (perpendicular to FH), making it roughly parallel to the vertical ramus of the mandible. The height and position of the auricle are defined by lines parallel to the FH through the supraorbitale (the most prominent part of the forehead between the eyebrows = 3) and the subnasale (junction of the columella and upper lip = 4). Because elective surgical procedures on the auricle are generally done for aesthetic improvement, preoperative counseling is essential. In case of total or subtotal auricular reconstruction the patient should not have unrealistic expectations about the outcome of an auricular reconstruction. It should always be emphasized that reconstructions can approximate a natural auricle but can rarely, if ever, achieve it. The alternative of a bone-anchored auricular prosthesis should be discussed. If autologous grafts are needed, the patient should understand the potential for donor site morbidity when the grafts are harvested (e. g., costal cartilage). Auricular surgery is easily performed under local anesthesia. If the operation lasts less than 1 hour, local anesthesia is even appropriate for cooperative children 12 years of age or older. Auricular surgery requires an intravenous line, premedication (e. g., midazolam), and appropriate monitoring (ECG, pulse oximetry, blood pressure in older patients). Fig. 15.4a–c Position of the auricle and angular measurements in cross-section (left auricle). a Lateral view showing the transverse plane (c) at the level of the ear canal. Corresponding vertical lines indicate the position of the antihelix and scapha. b Normally the helix projects no more than 1.5 cm from the head when viewed from the front. c Cross-section at the level of the ear canal. The retroauricular angle between the concha and scapha (scaphoconchal angle) is ca. 90°. The angle between the auricle and mastoid plane (concha– mastoid angle) is ca. 30°. General anesthesia is recommended in patients with heavy scarring of the operative site, in long operations involving extensive reconstruction, and in small children. Preschool age (4–5 years) is an excellent time for the surgical correction of prominent ears. This is recommended because very little auricular growth occurs after 5 years of age and because the auricular cartilage is still soft and pliable in this age group. The possibility of combining the otoplasty with other necessary procedures (adenoidectomy, paracentesis, inguinal hernia, phimosis) should be discussed with the parents. Local anesthesia is induced by injecting up to 10 mL of 1 % lidocaine solution with epinephrine (1:200 000). The needle is inserted in the retroauricular skin, and the anesthetic is injected in a fan-shaped pattern. The sensory branches of the vagus nerve and auriculotemporal nerve are blocked by an additional injection anterior to the tragus, directing the needle tip toward the floor of the ear canal. This may induce temporary, reversible facial paralysis, and this possibility should be disclosed during informed consent. Whenever possible, avoid shaving the scalp hairs for a standard otoplasty. It is sufficient to apply adhesive surgical drapes, and if necessary the (freshly washed) hair should be pulled back from the operative field and secured with clips or tied in a ponytail. Despite the potential for contamination, perioperative antibiotic prophylaxis is necessary only for complex reconstructions and graft procedures. It is also advisable in these cases to trim the hairs short in the operative area. Close shaving would obscure the hairline, which is an essential landmark in many reconstructive procedures. Instruments should permit the atraumatic handling of skin and cartilage. Subcutaneous fat and skin should be grasped with a fine surgical forceps, and cartilage with an Adson–Brown forceps. Dissection should be done with a pointed scissors. A single-pronged or small three-pronged hook should be used for the fixation of soft tissues and cartilage. Proper suture materials are essential for achieving a permanent result and avoiding complications. Cartilage incisions are sutured with absorbable material (e. g., 4–0 Vicryl). Nonabsorbable material should be used for cartilage-shaping sutures. Braided sutures predispose to infection and fistula formation due to their wicking action, so monofilament is preferred (e. g., 4–0 Ethibond). Clear sutures will be invisible through the thin skin. The removal of retroauricular skin sutures is often painful and difficult because the postoperative auricle cannot be retracted far from the head. Absorbable sutures that dissolve within approximately 8 days are advantageous, especially in children, but some subcutaneous sutures (e. g., 4–0 Vicryl) should also be used to stabilize the skin sutures. Fig. 15.5 Local anesthesia of the auricle and ear canal. The needle is inserted behind the postauricular sulcus, and local anesthetic is injected in a fan-shaped pattern to infiltrate the posterior auricular surface and especially the posterior circumference of the meatal opening. Local anesthetic is also injected anterior to the helical crus if an endaural auxiliary incision will be placed in the anterior notch. Surgery in the ear canal or skin mobilization anterior to the tragus also requires injection anterior to the tragus toward the temporomandibular joint. A prominent ear is generally corrected by reduction of the concha, the creation of an antihelical fold or roll, and setback of the corrected auricle. Conchal reduction is achieved by cartilage resection. An antihelix roll is created by approximating corresponding points on the auricular cartilage, with or without previous cartilage scoring, and general auricular setback is accomplished by suture fixation toward the mastoid plane. An antihelical fold is created by approximating pairs of anterior “cartilage points” with posteriorly placed sutures (with or without previous cartilage scoring). Historically, the methods for creating an antihelical fold are based on three major principles, all of which were published in 1963: Stenström (1963) found that simple manual reshaping of a prominent auricle could produce a normal-appearing ear. He believed it was unnecessary to remove cartilage and relied instead on creating an imbalance of stresses within the cartilage. In their pioneering study of hyaline rib cartilage, Gibson and Davis (1958) found that expansile forces generated by the matrix at the center of a cartilage cross-section counteracted the contractile forces exerted by the layer of close-packed chondrocytes on the cartilage surface. They called this the “balanced cross-section.” The perichondrium does not contribute to this balance of forces. When a layer of superficial cartilage is removed on one side, the balance is disrupted and the contractile force from the undamaged surface becomes dominant, causing the cartilage to curl in that direction. When Stenström did similar studies on auricular cartilage, he found that hyaline rib cartilage and elastic auricular cartilage behaved in the same way. He questioned the explanation of Gibson and Davis regarding contractile and expansile forces, however. The Stenström principle involves superficial scoring of the anterior surface of the antihelical cartilage. He separated the tail of the helix from the concha through a retroauricular skin incision and split the conchal cartilage in the direction of the helical crus. Access for cartilage scoring was gained by subcutaneous tunneling over the body of the antihelix, the posterior crus, and if necessary the anterior crus. He scored the cartilage using the blade of an Adson–Brown forceps with a Correction of Prominent Ears curved and elongated tip. An elliptical retroauricular skin excision at the level of the antihelix was an essential part of the Stenström procedure. Another method is to expose and score the anterior surface of the anti-helical cartilage “under vision” through a cartilage incision in the scapha (Chongchet 1963). The Scottish plastic surgeon Mustarde created an antihelix roll with posterior cartilage sutures made of soft silk (1963). This technique avoids the creation of sharp cartilage edges, and the cartilage is shaped by adjusting the tension under which the sutures are tied. He felt it was unnecessary to resect and reduce the conchal cartilage since the anti-helix can be “rolled back” with sutures. Luckett in New York had noted the possibility of shaping the antihelix with sutures in a much earlier publication (1910). He also claimed that the correction of auricular prominence by reducing the cephaloauricular angle did not address the underlying pathology, which required the creation of an antihelical fold. Potential problems of suture technique include suture fistula formation, recurrence due to “migration” of the cartilage sutures, and visibly tight sutures (like a violin bow) below the skin surface. Converse (1963) fashioned an antihelix and posterior crus by making parallel cartilage incisions in the scapha, triangular fossa, and concha and then joining the incisions with shaping sutures (chromic catgut ornylon). For very heavy cartilage, the correction was supported by thinning the retroauricular cartilage with a rotating wire brush. A posterior elliptical skin excision at the level of the antihelix completed the procedure. Our concept involves a graded approach. We use a suture-only technique when dealing with soft, malleable cartilage that does not show significant elastic recoil. Rigid cartilage is also weakened at selected sites by making incisions in the anterior cartilage surface (as practiced by Stenström and Chongchet). Once the auricle has been reshaped and the concha has been reduced if needed, the auricle is set back with concha–mastoid sutures (Furnas 1968). Besides general surgical risks such as infection (perichondritis) and bleeding (hematoma), the patient should understand the risks of excessive scarring (hypertrophic scars, keloids), auricular deformity, recurrence, and suture fistulas. A “prominent ear” does not present simply as a protruding auricle with an otherwise normal morphology. The affected auricle generally shows anatomical abnormalities, which is why this condition is considered a deformity rather than a normal variant (see Table 15.2). There are three typical deformities of auricular structure that require specific surgical correction to achieve a “normal” ear (Fig. 15.6a–c). When viewed from the front, the helix projects more than 1.5 cm from the lateral facial region. Protrusion of the upper two-thirds of the helix is caused mainly by absence or deficiency of the antihelical fold, especially the posterior crus. Middle-third prominence is accentuated by a deep concha, and lower-third prominence by frequent lateral protrusion of the earlobe. If the antihelix roll is absent and the concha is continuous with the scapha, a bowl-shaped auricle results. This deformity is characterized by prominence of the middle third of the auricle, which usually stands well away from the mastoid plane (concha–mastoid angle = 90°). The auricle should also be analyzed for additional deformities correctible with surgical techniques that go beyond a “standard otoplasty.” This would include the correction of a large scapha, which is usually associated with an absent or diminished helical fold (see Fig. 15.27). A lop ear may present initially as a simple auricular deformity. In reality, though, it is based on an abnormally short helical rim, which requires an entirely different surgical approach (see Fig. 15.28). Another problem is disproportion of the lower third of the auricle caused by excessive length of the earlobe. This problem can also be corrected with special techniques (see Fig. 15.24). Fig. 15.6a–c Analysis of the prominent auricle. a Lateral view. b Anterior view. c Superior view. 1 Absence of the antihelical fold 2 Prominent conchal bowl 3 Protruding earlobe The helix projects more than 1.5 cm from the mastoid plane. The concha–mastoid angle is approximately 90°. Lateral protrusion of the antitragus is a technically difficult problem to correct. Surgical correction should not be attempted without a compelling indication, which is rarely present. Patients should be advised of this special circumstance so that they will not attribute pre-existing prominence of the antitragus to the surgery itself. Timing: Prominent ears are usually corrected at 4–5 years of age, before the child begins school. The auricle should not undergo significant additional growth after age 5. In typical cases that require correction of the size, shape, and position of the auricle, the surgical procedure can be divided into several steps. These “building blocks” are largely independent of one another and can be assembled in a modular fashion to meet individual requirements. The operative steps are listed below and illustrated in Fig. 15.7. Additionally, the planning and conduct of the surgery should follow this principle: Retroauricular incision, exposure of the posterior cartilage surface and mastoid plane (Fig. 15.8a–c). The skin incision is made ca. 1 cm lateral and parallel to the postauricular sulcus. This will make the scars less conspicuous than an incision closer to the helix and will provide broad skin coverage for the antihelix shaping sutures (to prevent suture fistulas). The incision should extend far enough superiorly to furnish easy access to the posterior crus of the antihelix. The lower part of the incision should terminate on the posterior surface of the earlobe. The skin incision should not violate the cartilage or perichondrium. The skin is mobilized in the epiperichondrial plane as far as the helical rim, leaving the skin attached to the rim itself. It is important to undermine the skin completely so that the auricular cartilage can be everted through the incision, exposing all of its posterior surface (Fig. 15.8b). Small bleeding sites can be accurately controlled with bipolar coagulating forceps. The dissection is extended medially and posteriorly to expose the periosteum of the mastoid plane. The auricularis posterior muscle is resected to make room for the conchal setback (Fig. 15.8c). The posterior auricular artery is coagulated at this time. Care is taken to obtain adequate posterior mobilization of the mastoid skin. The mobilized area should approximately equal the area covered by the posterior auricular surface. Reduction of the concha by cartilage excision (Figs. 15.9, 15.10, 15.11). The concha is reduced by excising a crescent-shaped strip of cartilage. Generally the concha is most prominent in the middle third, and so the cartilage resection should be widest at that level (Fig. 15.9a). In a few cases the concha is most prominent in its upper third (Fig. 15.9b) or lower third, and the widest part of the excised crescent is shifted accordingly. The retroauricular cartilage incision is planned on the anterior auricular surface. The proposed cut edge of the cartilage should be “in the shadow” of the antihelix (Fig. 15.10a). Viewed in cross-section, an S-shaped transition will be created from the antihelix to the conchal bowl, with the cartilage incision placed at the transitional curve (Fig. 15.10b). The cartilage along this transition zone is pierced with three No. 16 hypodermic needles inserted from the anterior side of the auricle (Fig. 15.10a). The superior needle is inserted below the anterior crus, the middle needle at the site of maximum lateral protrusion, and the inferior needle below the antitragus. Next, the perichondrium and cartilage surface are incised from the retroauricular side with a No. 15 scalpel blade along an imaginary semicircular line connecting the needles. This initial incision should be superficial for marking purposes (Fig. 15.10c). Then the needles are removed. Actual division of the cartilage is now performed in one step while the middle finger of the free hand provides counter-pressure and helps to keep the scalpel from penetrating the anterior perichondrium and skin (Fig. 15.10d). The full cartilage thickness should be divided in one action; a jagged line may result if the initial cut is superficial and then deepened by additional cuts. When the cartilage is properly incised to the anterior perichondrium, the cut edges of the cartilage can be cleanly separated. If the incision does penetrate the anterior skin despite precautions, the wound is oversewn with 6–0 monofilament suture material. Fig. 15.7 Individual steps in the surgical correction of prominent ears: 1 Retroauricular incision 2 Excision of conchal cartilage 3 Creation of an antihelical fold 4 Correction of the earlobe 5 Setback of the corrected auricle 6 Retroauricular sutures Fig. 15.8a–c Incision and exposure of the posterior auricular surface. a The skin is incised ca. 1 cm lateral to the postauricular sulcus. b The skin is undermined on the posterior cartilage surface while preserving the perichondrium. c Cross-section at the level of the ear canal (corresponding to Fig. 15.4). The skin is elevated from the mastoid, leaving the periosteum intact. The auricularis posterior muscle may be resected to facilitate later setback of the auricle. Fig. 15.9a, b Types of conchal prominence. a Middle-third prominence. b Upper-third prominence. The strip resection is widest at the level where the concha is most prominent. The cartilage resection may proceed only after the skin has been elevated from the anterior cartilage surface. This begins by stripping the perichondrium from the anterior cartilage surface at a circumscribed site until the cartilage can be broadly grasped with an Adson–Brown forceps. This broad purchase is necessary to hold the cartilage securely for further dissection. If only a very circumscribed tissue area is grasped, it may easily tear or slip out of the forceps. Further dissection of the skin proceeds in the subperichondrial plane with a pointed scissors or elevator, mobilizing the skin as far as the meatal opening and the crus of the helix (Fig. 15.11a, b). This extensive mobilization is necessary due to the relative skin excess that will form after the cartilage resection. Broad undermining can distribute the redundant skin over a larger area with less (transient) folding of the skin. Next, a crescent-shaped cartilage strip of the desired size is resected from the concha with a curved, pointed scissors (Fig. 15.11c, d). Over-resection should be avoided. It is better to reduce the concha to the desired size progressively by a series of smaller strip resections. All bleeding sites on the perichondrial surface are carefully coagulated with bipolar forceps before the cartilage sutures are placed. Fig. 15.10a–d Reduction of the concha: planning, cartilage exposure, and incision. a Needles mark the line of the retroauricular cartilage incision. One each is passed through the cartilage at the center of the concha, below the antitragus, and below the anterior crus. b Corresponding cross-section at the level of the ear canal. The needle is placed in the shadow of the antihelix that will be formed. c The cartilage is marked by superficial retroauricular incision of the perichondrium along an imaginary line connecting the three needles. d Corresponding cross-section. The cartilage is divided with a No.15 scalpel blade while the finger of the free hand protects the anterior skin. Fig. 15.11a–f Dissection of the anterior conchal surface, cartilage resection, and cartilage sutures. a The anterior auricular skin is mobilized in the subperichondrial plane to the meatal opening while exposing the helical crus (arrow). b Corresponding cross-section. c A crescent-shaped strip of cartilage is resected with scissors. The width of the cartilage strip should be greatest at the level of maximum conchal prominence. d Corresponding cross-section. e The cartilage edges are approximated with absorbable figure-of-eight sutures. f Corresponding cross-section. The relative skin excess forms small, temporary folds along the anterior surface (arrow). Fig. 15.12a–d Creation of an antihelical fold. a Creation of antihelical fold by manual setback of the helix in the lateral view. The straight line marks the location of the cross-sectional planes in c and d. b Anterior view. c, d Auricular cross-section before and after setback of the helix. The goal of corrective surgery is to set back the helix so that it just visible outside the antihelix (*). This is accomplished by approximating the two cartilage points A and B. Fig. 15.13a–d Defining a pair of points on the anterior auricular surface. The shaping sutures are placed on the posterior surface. a Point 1 on the anterior surface of the scapha is located by forceps pressure and marked with a needle. b A suture is passed through point 1, piercing the cartilage at a single point (see arrows at lower left). c Opposing point 2 is located in the shadow of the antihelix. It is then shifted slightly toward the earlobe (see arrow). d A wide suture bite is taken through the cartilage, generally in the area of the previous conchal incision (see arrows at lower right). The cut edges are re-approximated with cartilage sutures (Fig. 15.11e
Basic Principles and General Measures
Surgical Anatomy—Muscles, Nerves, and Vessels
External Ear
 Rules, Tips, and Tricks
Rules, Tips, and Tricks
 Rules, Tips, and Tricks
Rules, Tips, and Tricks
Ear Canal
 Rules, Tips, and Tricks
Rules, Tips, and Tricks
Muscles
Nerves
Vessels
Preoperative Diagnosis, Documentation, and Counseling
 Rules, Tips, and Tricks
Rules, Tips, and Tricks
 Helix: helical rim is flattened or unfolded (scapha too large). Helical circumference is too short, causing lateral overhang of the upper helix (cup ear, lop ear).
Helix: helical rim is flattened or unfolded (scapha too large). Helical circumference is too short, causing lateral overhang of the upper helix (cup ear, lop ear).
 Antihelix: prominent helix due to absence of the antihelical fold, especially its posterior crus.
Antihelix: prominent helix due to absence of the antihelical fold, especially its posterior crus.
 Concha: deepening of the conchal bowl causing middle-third protrusion of the auricle (viewed from the front).
Concha: deepening of the conchal bowl causing middle-third protrusion of the auricle (viewed from the front).
 Earlobe: large and pendulous, absent, or “attached.”
Earlobe: large and pendulous, absent, or “attached.”
Anesthesia and Preoperative Preparations
Anesthesia
Principle
Contraindications
 Severe cardiovascular disease with arrhythmia and hyper-tension.
Severe cardiovascular disease with arrhythmia and hyper-tension.
 Allergy to local anesthetics.
Allergy to local anesthetics.
 Anticoagulant therapy.
Anticoagulant therapy.
 Platelet aggregation inhibitors should be discontinued at least 2 weeks before surgery.
Platelet aggregation inhibitors should be discontinued at least 2 weeks before surgery.
Timing of Surgery
 Rules, Tips, and Tricks
Rules, Tips, and Tricks
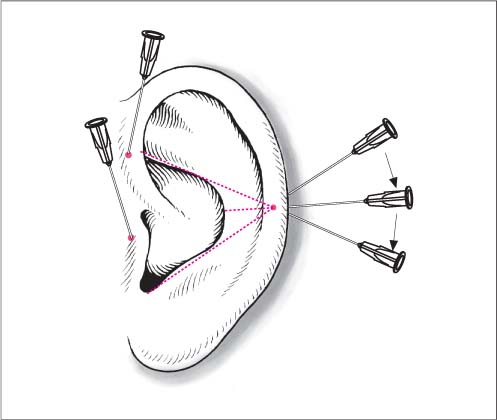
Technique of Local Anesthesia (Fig. 15.5)
Preoperative Preparations
Instruments and Suture Materials
Instruments
Suture Materials
Correction of Prominent Ears
Surgical Principle
 Rules, Tips, and Tricks
Rules, Tips, and Tricks
 Scoring only (Stenström).
Scoring only (Stenström).
 Sutures only (Mustarde).
Sutures only (Mustarde).
 Combination of scoring and sutures (Converse).
Combination of scoring and sutures (Converse).
Indications
 The indications depend on the degree of deformity. The criteria cited earlier, such as the concha–mastoid angle, scaphoconchal angle, lateral projection of the helix, and size of the conchal bowl, should be well outside the normal range.
The indications depend on the degree of deformity. The criteria cited earlier, such as the concha–mastoid angle, scaphoconchal angle, lateral projection of the helix, and size of the conchal bowl, should be well outside the normal range.
 Generally the more pronounced the abnormality, the more rewarding the surgical procedure. The correction of very mild deformities is difficult, but rarely gratifying for either patient or surgeon.
Generally the more pronounced the abnormality, the more rewarding the surgical procedure. The correction of very mild deformities is difficult, but rarely gratifying for either patient or surgeon.
 It is common to find differences in the degree and location of deformities between the two ears. It is still advisable in these cases to perform a bilateral correction, as experience has shown that the uncorrected ear will usually appear prominent relative to the operated side.
It is common to find differences in the degree and location of deformities between the two ears. It is still advisable in these cases to perform a bilateral correction, as experience has shown that the uncorrected ear will usually appear prominent relative to the operated side.
Contraindications
 A very mild degree of cosmetic deformity would contraindicate otoplasty, especially in adults. Patients seeking corrective surgery in this situation will generally have a significant psychological component, and in most cases the auricle is not the real problem. Even with a technically excellent otoplasty, the patient is likely to be dissatisfied with the result.
A very mild degree of cosmetic deformity would contraindicate otoplasty, especially in adults. Patients seeking corrective surgery in this situation will generally have a significant psychological component, and in most cases the auricle is not the real problem. Even with a technically excellent otoplasty, the patient is likely to be dissatisfied with the result.
 Otoplasty may be contraindicated for medical reasons including a high susceptibility to infections due to immune deficiency (diabetes, HIV infection, corticosteroid therapy) and proneness to hypertrophic scarring or keloids. The auricular skin is a site of predilection for keloid formation, which may occur in response to surgery or injury. Keloids appear as raised, lobulated, bluish-gray scars that transgress the boundaries of the original injury to involve healthy skin. Hypertrophic scars are also raised above the skin surface but are always confined to the injured area. Patients with pre-existing keloids are assumed to be prone to keloid formation and should not undergo auricular surgery—though it is not always helpful to make an individual risk assessment based on scars in other body regions, because a retroauricular skin incision may form a keloid even in patients with a normal-appearing appendectomy scar, for example.
Otoplasty may be contraindicated for medical reasons including a high susceptibility to infections due to immune deficiency (diabetes, HIV infection, corticosteroid therapy) and proneness to hypertrophic scarring or keloids. The auricular skin is a site of predilection for keloid formation, which may occur in response to surgery or injury. Keloids appear as raised, lobulated, bluish-gray scars that transgress the boundaries of the original injury to involve healthy skin. Hypertrophic scars are also raised above the skin surface but are always confined to the injured area. Patients with pre-existing keloids are assumed to be prone to keloid formation and should not undergo auricular surgery—though it is not always helpful to make an individual risk assessment based on scars in other body regions, because a retroauricular skin incision may form a keloid even in patients with a normal-appearing appendectomy scar, for example.
Specific Points Regarding Informed Consent
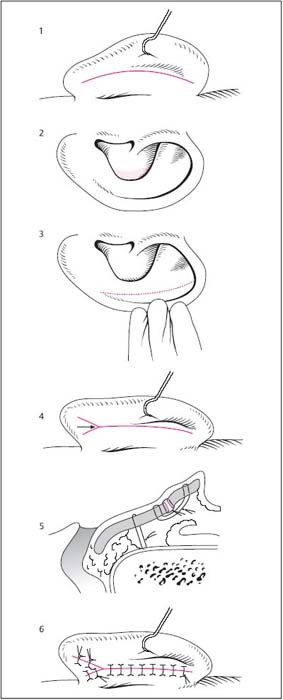
Operative Planning
Surgical Technique
 Rules, Tips, and Tricks
Rules, Tips, and Tricks
 Retroauricular incision.
Retroauricular incision.
 Excision of conchal cartilage.
Excision of conchal cartilage.
 Creation of an antihelical fold.
Creation of an antihelical fold.
 Correction of the earlobe.
Correction of the earlobe.
 Setback of the reduced and reshaped auricle.
Setback of the reduced and reshaped auricle.
 Retroauricular sutures.
Retroauricular sutures.
 The correction is planned on the anterior auricular surface and performed on the posterior auricular surface.
The correction is planned on the anterior auricular surface and performed on the posterior auricular surface.
 Rules, Tips, and Tricks
Rules, Tips, and Tricks
![]()
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree